To analyze and compare lung function of obese and healthy, normal-weight children and adolescents, without asthma, through spirometry and volumetric capnography.
MethodsCross-sectional study including 77 subjects (38 obese) aged 5–17 years. All subjects underwent spirometry and volumetric capnography. The evaluations were repeated in obese subjects after the use of a bronchodilator.
ResultsAt the spirometry assessment, obese individuals, when compared with the control group, showed lower values of forced expiratory volume in the first second by forced vital capacity (FEV1/FVC) and expiratory flows at 75% and between 25 and 75% of the FVC (p<0.05). Volumetric capnography showed that obese individuals had a higher volume of produced carbon dioxide and alveolar tidal volume (p<0.05). Additionally, the associations between dead space volume and tidal volume, as well as phase-3 slope normalized by tidal volume, were lower in healthy subjects (p<0.05). These data suggest that obesity does not alter ventilation homogeneity, but flow homogeneity. After subdividing the groups by age, a greater difference in lung function was observed in obese and healthy individuals aged >11 years (p<0.05).
ConclusionEven without the diagnosis of asthma by clinical criteria and without response to bronchodilator use, obese individuals showed lower FEV1/FVC values and forced expiratory flow, indicating the presence of an obstructive process. Volumetric capnography showed that obese individuals had higher alveolar tidal volume, with no alterations in ventilation homogeneity, suggesting flow alterations, without affecting lung volumes.
Analisar e comparar a função pulmonar de crianças e adolescentes obesos e eutróficos saudáveis, sem asma, pela espirometria e capnografia volumétrica.
MétodosEstudo transversal incluindo 77 indivíduos (38 obesos) com idade entre cinco a 17 anos. Todos os indivíduos realizaram espirometria e capnografia volumétrica. Os obesos repetiram as avaliações após o uso de broncodilatador.
ResultadosNa avaliação da espirometria, os indivíduos obesos, quando comparados ao grupo controle, apresentaram menores valores no volume expiratório forçado no primeiro segundo pela capacidade vital forçada (VEF1/CVF) e nos fluxos expiratórios a 75% da CVF e entre 25-75% da mesma (p<0,05). A capnografia volumétrica demonstrou que os obesos apresentam maior volume produzido de dióxido de carbono e volume corrente alveolar (p<0,05). Além disso, a relação entre o volume espaço morto e volume corrente, bem como o slope da fase 3 normalizado pelo volume corrente foram menores nos indivíduos saudáveis (p<0,05). Esses dados sugerem que a obesidade não altera a homogeneidade da ventilação, mas sim dos fluxos. Ao subdividir os grupos por idade, foi observada maior diferença na função pulmonar entre indivíduos obesos e saudáveis na faixa etária acima de 11 anos (p<0,05).
ConclusãoMesmo sem o diagnóstico de asma por critérios clínicos e sem resposta ao uso de broncodilatador, os indivíduos obesos apresentaram menores valores no VEF1/CVF e nos fluxos expiratórios forçados, indicando a presença de processo obstrutivo. A capnografia volumétrica indicou nos indivíduos obesos maior volume corrente alveolar, sem alterações na homogeneidade da ventilação, sugerindo alteração nos fluxos, sem comprometimento dos volumes pulmonares.
Childhood and adolescent obesity has currently reached epidemic proportions and is considered one of the greatest challenges for public health in the 21st century.1 Considering this rising prevalence, there is a special concern, as dysfunctions resulting from excess fat mass show an increasingly earlier onset, which affect the well-being of these individuals since childhood.2,3
One of the deleterious effects of obesity is lung function impairment. Among obese individuals in adulthood, this impairment is already evident in literature.4–7 It is known that the deposition of adipose tissue on the rib cage leads to an impairment in its compliance and, consequently, to the decrease in its expandability. The mechanical impairment triggers changes in the lung elastic properties, resulting in reduced functional residual capacity, tidal volume (TV), and expiratory reserve volume (ERV). Additionally, there is a reduction in forced vital capacity (FVC) and, consequently, of the total lung capacity.4–7
However, the mechanism through which obesity impairs lung function appears to be different in the young population. The results shown in the literature are divergent in relation to the lung function of obese children and adolescents. Discrepancies regarding findings might be influenced by changes in body structure during this period. Moreover, studies include different age and ethnic groups.8–15
Spirometry is the most used tool for the analysis of lung function. Its use has been described in increasingly younger populations.16 However, it is an effort-dependent test that requires understanding and cooperation of the assessed individual, which can generate difficulties in younger subjects. Therefore, the search for new evaluation methods that can be used in this population has been encouraged.
In this context, volumetric capnography (VC) has emerged as an alternative tool for the detection of lung dysfunctions. It is a simple and inexpensive test that does not use inert gases, as it analyzes the carbon dioxide (CO2) produced by the lungs. The test consists in analyzing CO2 as a function of the exhaled TV, and the exhalation pattern is divided into three phases: phase 1, which is compatible with air in the conduction airways and dead space; phase 2 encompasses the proximal airways; and phase 3, known as the alveolar plateau, is related to the peripheral airways.
The advantage of VC is that it does not require forced maneuvers, being easy to perform, even in younger individuals. VC was first developed for use in individuals undergoing mechanical ventilation,17–23 and its use in spontaneously breathing individuals is recent, with few published studies, especially in children.24–29 There is no standardization for data analysis in VC in the literature.
Therefore, the study aimed to evaluate lung function in obese children and adolescents (without asthma) through spirometry and VC, and to compare the results with a control group of healthy, normal-weight individuals in the same age group.
MethodsStudy subjectsThe study included 38 obese subjects (20 boys) aged 5–17 years and 39 healthy subjects (17 boys) in the same age group. The sample size calculation was based on spirometry markers, obtained in a pilot study, and considering an α error of 0.05 and a β error of 0.20. With these assumptions, the achieved sample value comprised 31 individuals in each group (obese and healthy controls) for FVC and 17 for mean forced expiratory flow between 25% and 75% of FVC (FEF25–75%) – the variables that showed greater variability. In this context, the study sample power was higher than 80%.
The obese individuals included in the present study are regularly followed-up at the Multidisciplinary Outpatient Clinic for Obese Children and Adolescents. To define obesity, the Center for Disease Control and Prevention (CDC) criteria were used for individuals aged 2–20 years. Individuals who were above the 95th percentile for body mass index (BMI) were considered obese. The study included only individuals with exogenous obesity.
Healthy, normal-weight individuals with BMI within the normal range (BMI between the 5th and 85th percentile), who comprise the database of the Lung Physiology Laboratory of the Center for Pediatric Research at Unicamp were included in the control group.
To be included in the study, participants’ parents or guardians signed the free and informed consent form and none of the included patients were smokers and/or had any current respiratory diseases, such as colds.
A response to the use of bronchodilator (BD) greater than 10% for forced expiratory volume in the first second of the FVC (FEV1) was considered as an exclusion criterion, as it is indicative of asthma. However, none of individuals had to be excluded for that reason.
Individuals with a clinical history of any other respiratory diseases, such as chronic obstructive pulmonary disease and sleep apnea, were also excluded. This evaluation was performed through the analysis of the outpatient medical records of the study subjects. The study was approved by the Ethics Committee of the University (#1165/2009).
Study designThis was a cross-sectional and analytical study with a control group comparing lung function in obese and healthy children and adolescents through spirometry and VC.
BMIRegarding obesity, the CDC criteria were used for the inclusion of individuals in the study (girls: http://www.cdc.gov/growthcharts/data/set1/chart16.pdf and boys: http://www.cdc.gov/growthcharts/data/set1/chart15.pdf). Subsequently, for the statistical purposes of the study, the data were transformed into z-scores, according to the World Health Organization criteria.
Lung function assessmentsPrior to the evaluations, all subjects rested for at least 10min. First, the VC was performed, as it is a passive evaluation; subsequently, the spirometry was performed, because it is effort-dependent. Obese subjects repeated the evaluations 20min after the use of a BD. Albuterol (C13H21NO3 [400mg]) was administered for bronchodilation.
SpirometrySpirometry was performed according to the standards of the European Respiratory Society and American Thoracic Society. The acceptance criterion for the spirometry test comprised at least three acceptable and two reproducible standard curves. All study subjects met the criteria for acceptance.
A CPFS/D spirometer (Medical Graphics Corp., MN, USA) was used with the software BREEZE PF Windows version 3.8 (Medical Graphics Corp., MN, USA). The data were converted to z-scores according to the normality criteria established by Quanjer et al. (2012) using the GLI2012 software, produced by the Global Lung Initiative (GLI), a Task Force of the European Respiratory Society.16
The z-scores of the following variables were analyzed: FVC, FEV1, FEV1/FVC, forced expiratory flow at 75% of FVC (FEF75%), and FEF25–75%. The ERV was also evaluated by the percentage of the predicted value.
Volumetric capnographyThe VC analysis was performed using the non-invasive CO2SMO monitor (Dixtal, São Paulo, Brazil), using the Analysis Plus® software, Windows version. Participants performed the test in the sitting position, using a nasal clip and no visual contact with the monitor, to prevent visual influence on the respiratory pattern. They were instructed to breathe calmly, for 5min, into the mouthpiece connected to the monitor. Respiratory cycles were corrected so that there was no variation greater than 25% of expired volume (EV) and 5% of CO2 at the end of expiration (EtCO2), according to the pattern of previous studies.25,27
At the statistical analysis, the corrected mean values of the following variables were used: total minute volume (MVt); minute alveolar volume (MValv), TV; alveolar tidal volume (TValv); dead space volume (DSV); the DSV/TV ratio (DSV/TV); volume of expired CO2 (VCO2); EtCO2; respiratory rate (RR); peripheral oxygen saturation (SpO2); slopes of phases 2 and 3 (Slp2 and Slp3), which are numerical representations of CO2 exhalation curve; normalization of slopes by TV, to equalize the differences in height and weight (Slp2/VC and Slp3/VC)27; and the capnography index, proposed by Fuchs et al. (Slp3/Slp2)×100) to quantify ventilation homogeneity.26
Analysis of resultsThe SPSS 21.0 software (SPSS Inc., IL, USA) was used for statistical analysis. The comparisons between the study categorical variables were performed using the chi-squared test. The comparisons of numerical variables between two groups was performed using the Mann–Whitney test. Linear regression was used to quantify the association between lung function variables and BMI z-score. All data were corrected by the Bonferroni test, considering an α<0.05/number of tests performed with each variable.
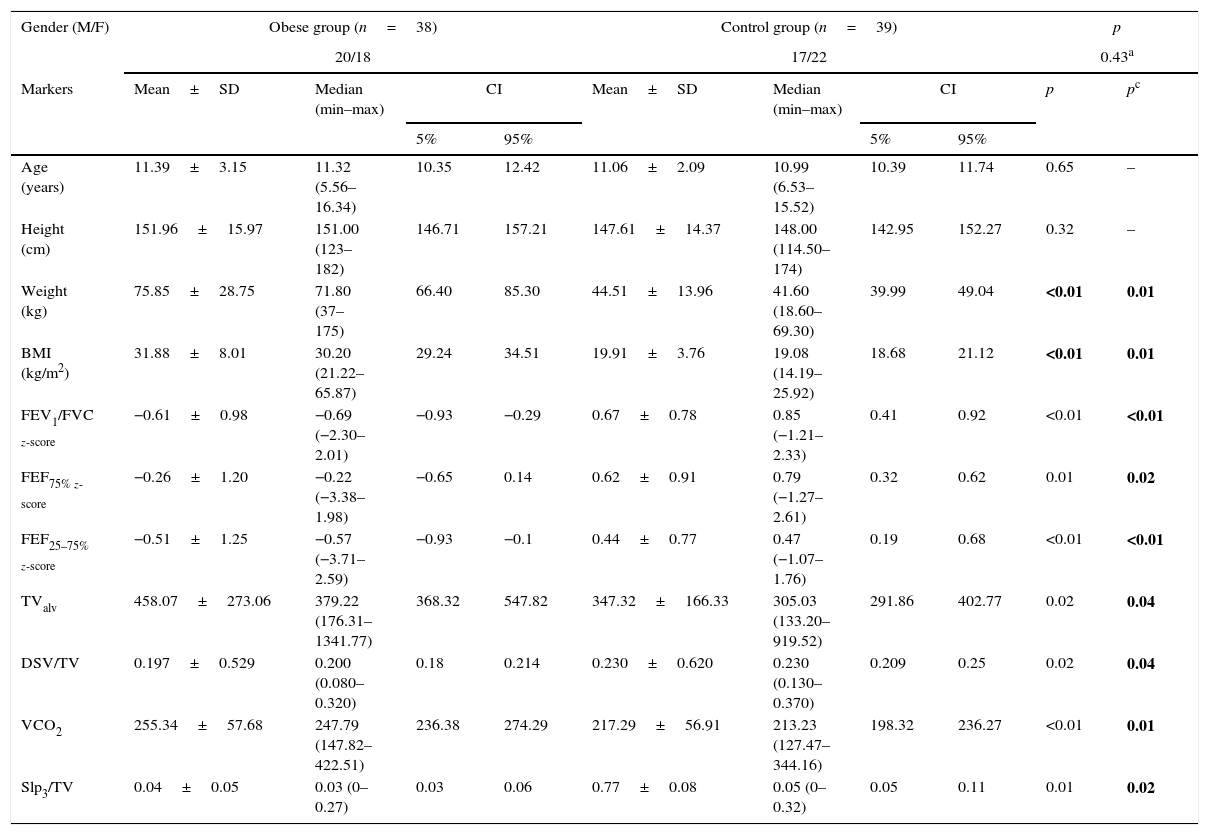
ResultsStudy subjectsThe study comprised 38 obese (20 boys) and 39 healthy (17 boys) individuals, whose age ranged from 5.56 to 16.54 years. The descriptive analysis of the anthropometric data of the participants is shown in Table 1. Body weight and BMI were different between the groups, and there was no difference between the groups regarding age, gender, and height.
Comparison between the groups’ anthropometric data with spirometry and volumetric capnography variables that showed a positive association.
| Gender (M/F) | Obese group (n=38) | Control group (n=39) | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 20/18 | 17/22 | 0.43a | ||||||||
| Markers | Mean±SD | Median (min–max) | CI | Mean±SD | Median (min–max) | CI | p | pc | ||
| 5% | 95% | 5% | 95% | |||||||
| Age (years) | 11.39±3.15 | 11.32 (5.56–16.34) | 10.35 | 12.42 | 11.06±2.09 | 10.99 (6.53–15.52) | 10.39 | 11.74 | 0.65 | – |
| Height (cm) | 151.96±15.97 | 151.00 (123–182) | 146.71 | 157.21 | 147.61±14.37 | 148.00 (114.50–174) | 142.95 | 152.27 | 0.32 | – |
| Weight (kg) | 75.85±28.75 | 71.80 (37–175) | 66.40 | 85.30 | 44.51±13.96 | 41.60 (18.60–69.30) | 39.99 | 49.04 | <0.01 | 0.01 |
| BMI (kg/m2) | 31.88±8.01 | 30.20 (21.22–65.87) | 29.24 | 34.51 | 19.91±3.76 | 19.08 (14.19–25.92) | 18.68 | 21.12 | <0.01 | 0.01 |
| FEV1/FVC z-score | −0.61±0.98 | −0.69 (−2.30–2.01) | −0.93 | −0.29 | 0.67±0.78 | 0.85 (−1.21–2.33) | 0.41 | 0.92 | <0.01 | <0.01 |
| FEF75% z-score | −0.26±1.20 | −0.22 (−3.38–1.98) | −0.65 | 0.14 | 0.62±0.91 | 0.79 (−1.27–2.61) | 0.32 | 0.62 | 0.01 | 0.02 |
| FEF25–75% z-score | −0.51±1.25 | −0.57 (−3.71–2.59) | −0.93 | −0.1 | 0.44±0.77 | 0.47 (−1.07–1.76) | 0.19 | 0.68 | <0.01 | <0.01 |
| TValv | 458.07±273.06 | 379.22 (176.31–1341.77) | 368.32 | 547.82 | 347.32±166.33 | 305.03 (133.20–919.52) | 291.86 | 402.77 | 0.02 | 0.04 |
| DSV/TV | 0.197±0.529 | 0.200 (0.080–0.320) | 0.18 | 0.214 | 0.230±0.620 | 0.230 (0.130–0.370) | 0.209 | 0.25 | 0.02 | 0.04 |
| VCO2 | 255.34±57.68 | 247.79 (147.82–422.51) | 236.38 | 274.29 | 217.29±56.91 | 213.23 (127.47–344.16) | 198.32 | 236.27 | <0.01 | 0.01 |
| Slp3/TV | 0.04±0.05 | 0.03 (0–0.27) | 0.03 | 0.06 | 0.77±0.08 | 0.05 (0–0.32) | 0.05 | 0.11 | 0.01 | 0.02 |
n, number of patients; p, p-value; pc, p-value corrected by the Bonferroni test; M, male; F, female; CI, confidence interval; SD, standard deviation; min, minimum; max, maximum; BMI, body mass index; kg/m2, kilograms per square meter; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; FEF75%, forced expiratory flow at 75% of FVC; FEF25–75%, forced expiratory flow between 25% and 75% of FVC; TValv, alveolar tidal volume; DSV, dead space volume; TV, tidal volume; VCO2, exhaled carbon dioxide volume; Slp3/TV, phase-3 slope corrected by TV.
Bold means “Statistically Significant”.
Study participants underwent lung function testing through spirometry and VC. Table 1 shows the variables that were different between the groups at the lung function analysis. FEV1/FVC, FEF75%, and FEF25–75% were lower in the obese group, even after the Bonferroni correction. In the sample, 36.8% of obese individuals had FEF25–75% below 70% of the predicted value, characterizing obstructive flow disorders. There were no alterations in subjects from the control group at this evaluation. There was no difference between the groups regarding FVC, FEV1, and ERV.
Regarding the VC, a difference was observed between the groups for DSV/TV and Slp3/TV, which were lower in obese patients, and in TValv and VCO2, which were higher. There was no difference regarding the capnography index between the groups.
When analyzing the response of obese individuals to the use of BD, it was verified that none of the participants showed a response higher than 10% in FEV1, disproving the diagnosis of asthma. Regarding FVC (p=0.05), a reduction after medication was observed, and consequently an increase in FEV1/FVC (p=0.02). In the VC, the use of BD resulted in a reduction in MVt (p=0.01), MValv (p=0.01), and VCO2 (p=0.02), and an increase in DSV (p<0.01) and DSV/TV (p<0.01). Therefore, the obese individuals did not show a positive response to the use of BD.
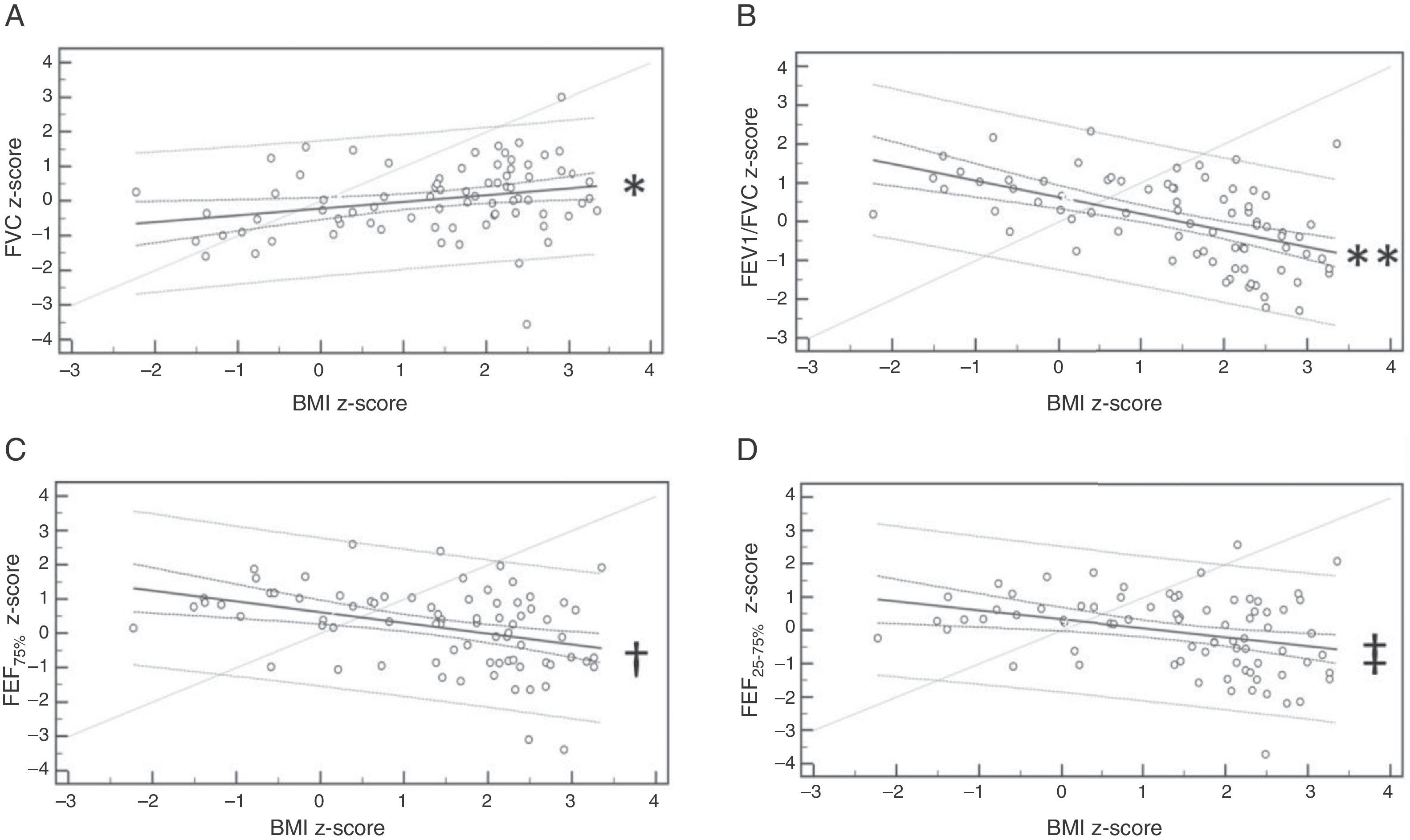
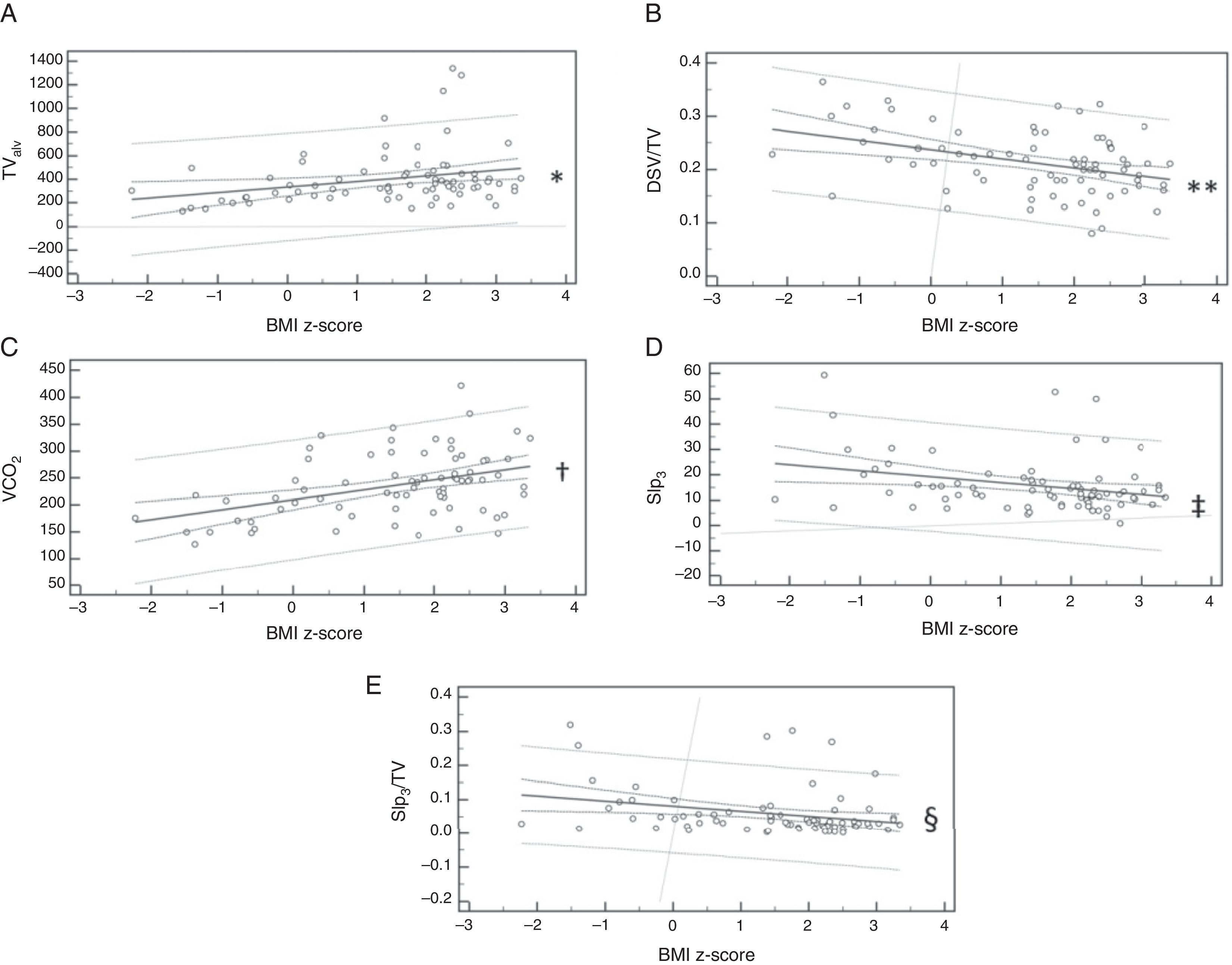
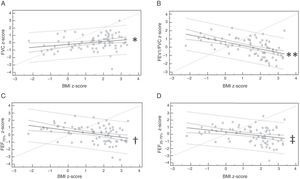
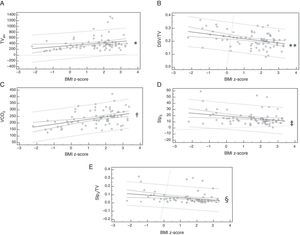
Lung function and body massFigs. 1 and 2 show, respectively, the spirometry and VC variables that were influenced by the BMI z-score. In the analysis of linear regression, it was verified that BMI influences FVC, FEV1/FVC, FEF75%, and FEF25–75%. In the VC, the variables TValv, DSV/TV, VCO2, Slp3, and Slp3/TVwere influenced by BMI.
Linear regression of spirometry variables influenced by z-score of body mass index (BMI). (A) Forced vital capacity (FVC) z-score: y=−0.21+0.20x; *p=0.020; (B) ratio between forced expiratory volume in the first second and FVC (FEV1/FVC) z-score: y=0.64−0.43x; **p<0.001; (C) forced expiratory flow at 75% of FVC (FEF75%) z-score: y=0.63−0.31x; †p=0.001; (D) forced expiratory flow between 25% and 75% of FVC (FEF25–75%) z-score: y=0.34−0.27x; ‡p=0.005.
Linear regression of the volumetric capnography variables influenced by the body mass index (BMI) z-score. (A) Alveolar tidal volume (TValv): y=335.26+47.45x; *p=0.050; (B) ratio between the dead space volume and tidal volume (DSV/TV): y=0.24−0.02x; **p=0.003; (C) exhaled carbon dioxide volume (VCO2): y=209.98+18.51x; †p=0.003); (D) phase 3-slope (Slp3): y=19.32−2.32x; ‡p=0.041; (E) phase-3 slope corrected by tidal volume (Slp3/TV): y=0.08−0.01x; §p=0.044.
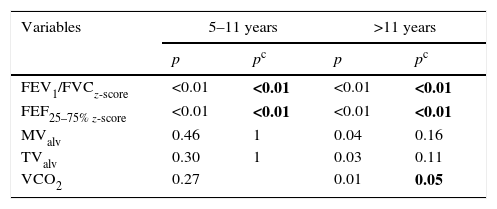
The study participants were subdivided into two subgroups according to the age range (ages 5–11 and age >11 years), to verify whether differences in lung function occurred even at the youngest age groups or started when the individual was already in the process of pubertal maturation.
It was observed that the obese individuals had lower FEV1/FVC values, even at the younger age groups. However, the changes in FEF and increase in lung volumes, analyzed by VC, were significant only in the older group. Table 2 shows the p-values that were significant in lung function analysis according to the age group.
Differences between obese and healthy patients in lung function evaluation according to age range.
| Variables | 5–11 years | >11 years | ||
|---|---|---|---|---|
| p | pc | p | pc | |
| FEV1/FVCz-score | <0.01 | <0.01 | <0.01 | <0.01 |
| FEF25–75% z-score | <0.01 | <0.01 | <0.01 | <0.01 |
| MValv | 0.46 | 1 | 0.04 | 0.16 |
| TValv | 0.30 | 1 | 0.03 | 0.11 |
| VCO2 | 0.27 | 0.01 | 0.05 | |
p, p-value; pc, p-value corrected by the Bonferroni test; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; FEF25–75%, forced expiratory flow between 25% and 75% of FVC; MValv, alveolar minute volume; TValv, alveolar tidal volume; VCO2, exhaled carbon dioxide volume. The Mann–Whitney test was used for statistical analysis, considering an alpha=0.05.
Bold means “Statistically Significant”.
The complexity of obesity and its close association with other diseases encourages the search for an understanding of the mechanisms involved in the chain of deleterious effects caused by excess body weight. When analyzing the effects of obesity during childhood and adolescence, the analysis should be even more careful, as this period is marked by changes in body structure.28
The interaction between such dynamic and intense processes may be the reason for the divergence in the literature that addresses the influence of obesity on lung function in children and adolescents. In addition to the subject complexity, the studies differ in relation to age group and population characteristics.
Among the adult population, the literature is clear in establishing that obesity affects lung function through a restrictive process.5,7 In young individuals, studies highlight the association between obesity and asthma, but there are few conclusions regarding the subject in individuals without asthma.
In the present study, it was observed that the obese individuals had lower FEV1/FVC and FEF values. The findings regarding the expiratory flows should be analyzed with caution due to the variability of the technique and the method used. It was also observed that obese individuals had higher FVC values; however, after the Bonferroni correction, this difference did not remain significant.
Among the findings, what is more frequently observed in the literature and that is consistent with the present study, is the lower FEV1/FVC value among the obese individuals. Regarding FVC and FEV1, the findings are contradictory, with studies showing positive, negative, or no association in the comparison of obese and healthy individuals. The inconsistency of the findings is maintained for the analysis of expiratory flows and ERV.8–15
It is known that lung capacity depends on the body dimensions and efficiency of the systems that constitute the human body. Thus, both body growth and pubertal development may influence lung function. As there are differences in the onset and duration of each individual's growth and puberty periods, the analysis of lung function, subdividing the groups by pubertal development, could provide a better understanding of how growth influences the alterations in lung function. This was a limitation of the present study.28,29
Therefore, the authors sought to improve the accuracy and reliability of the study by using two different mechanisms of pulmonary function assessment. In addition to spirometry, which is currently the most often used tool for this analysis, individuals were assessed through VC.
The use of VC in clinical practice started in the 1980s with Fletcher et al.17 However, it was mainly used in intubated individuals submitted to mechanical ventilation.18–21 The use of VC for the analysis of lung function in spontaneously breathing individuals is even more recent and has been applied in several clinical conditions.22–27 In the pediatric age group, the literature is even scarcer, and studies were found only in individuals with asthma, cystic fibrosis, and bronchopulmonary dysplasia.24–27 To the best of the authors’ knowledge, this is the first study to evaluate obese children and adolescents in spontaneous breathing through spirometry and VC, simultaneously.
Despite the scarce literature, VC is an option for the analysis of lung function in children and adolescents, as it is an easy-to-understand test, with no need for forced maneuvers, being inexpensive and not requiring the use of inert gases. Additionally, it provides information on lung volume and DSV, as well as ventilation homogeneity through the CO2 exhalation slopes.
In the present study, it was observed that obese individuals have greater lung volumes than healthy individuals (TValv and VCO2) and lower values of DSV/TV and Slp3/TV.
Slp3 and Slp3/TV are indicators of ventilation inhomogeneity when they are increased, as observed in cystic fibrosis, asthma, pulmonary bronchodysplasia, chronic obstructive pulmonary disease, and bronchiectasis.22–27 Obese individuals, therefore, despite flow alterations in spirometry, do not have alterations in ventilation homogeneity, as they have lower values in Slp3/TV and there were no differences between the groups for Slp3 and capnography index.
The explanation for lower values in Slp3/TV in obese individuals is consistent with the findings of Ream et al., who evaluated children and adolescents who were intubated and submitted to minor surgeries and found lower values of Slp3 in individuals with higher TV and a negative association between Slp3 and body weight and surface area.19 Therefore, obese individuals, who have higher weight, body surface area, and TV than the control group, showed lower Slp3/TV values.
The DSV/TV ratio is used to monitor respiratory disease severity in mechanically ventilated patients.18,21 In the present study, lower values were observed in obese patients than in healthy individuals, indicating absence of pulmonary disease. The lower values found in obese individuals were influenced by the higher TVs.
VC was shown to be a complementary tool to the spirometry, as it detected increased lung volumes during spontaneous breathing without forced maneuvers, a finding that was not detected by the spirometry. However, this tool is not capable of detecting changes in respiratory flows. For this reason, one evaluation does not replace the other, but the complementary use of both may improve the knowledge about the pulmonary status of the assessed individuals.
Lung volume analysis was relevant, mainly after the subdivision of the individuals by age groups. FEV1/FVC and forced expiratory flows were altered in the group aged 5–11 years, as well as in those older than 11 years. However, VCO2 was different only in the older group.
The increase in lung volume may be a response to increased cardiorespiratory demand in obese individuals, especially during pubertal development, which is characterized by changes in body structure.28,30 However, obese patients may have smaller-caliber airways due to the impairment of respiratory mechanics by adipose tissue. Thus, increasing volume in a smaller-caliber unit results in reduced respiratory flows.
Even without the diagnosis of asthma according to the clinical criteria and response to BD use, obese individuals showed lower values in FEV1/FVC and FEF, indicating the presence of an obstructive process, even at the younger age groups. However, the VC analysis showed that the highest values of TValv and VCO2 were observed in obese individuals, which was more significant in individuals older than 11 years. No changes were observed in Slp3, Slp3/TV, and in the capnography index. Thus, the study suggests that obese individuals show alterations in lung flow, even at the younger age groups, without compromising lung volumes and ventilation homogeneity.
Conflicts of interestThe authors declare no conflicts of interest.
MSF would like to thank the support from CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior). FALM would like to thank the support from FAPESP (Fundação de Apoio a Pesquisa do Estado de São Paulo) [2011/12939-4]; [2015/12858-5]; [2015/12183-8] and Fundo de Apoio à Pesquisa, ao Ensino e à Extensão da Universidade de Campinas [648/2015]. JDR would like to thank the support from FAPESP [2011/18845-1]; [2015/12183-8].
Please cite this article as: Ferreira MS, Mendes RT, Marson FA, Zambon MP, Antonio MA, Paschoal IA, et al. Spirometry and volumetric capnography in lung function assessment of obese and normal-weight individuals without asthma. J Pediatr (Rio J). 2017;93:398–405.