Obesity is associated with the abnormal glucose metabolism preceding type 2 diabetes mellitus. Thus, further investigation on the prediction of this lethal outcome must be sought. The objective was the profile glycemic assessment of asymptomatic obese children and adolescents from Salvador, Brazil.
MethodA fasting venous blood sample was obtained from 90 consecutive obese individuals aged 8–18 years, of both sexes, for laboratory determinations of glycated hemoglobin, basal insulin, and the Homeostasis Model Assessment Insulin Resistance index. The clinical evaluation included weight, height, waist circumference, assessment of pubertal development, and acanthosis nigricans research. The body mass index/age indicator was used for the severity of overweight assessment.
ResultsGlycemic alterations were evidenced clinically and biochemically, although these individuals had no complaints or symptoms related to blood sugar levels. Quantitative and qualitative variables were respectively expressed measures of central tendency/dispersion and simple/relative frequency, using the SPSS, version 20.0. A p-value <0.05 was considered significant.
ConclusionNotably, this study found a high prevalence of glucose and insulin disorders in asymptomatic obese children and adolescents.
A obesidade está associada ao metabolismo da glicose anormal que antecede a diabetes mellitus tipo 2. Assim, uma investigação adicional sobre a predição desse resultado letal deve ser antecipada. O objetivo era a avaliação do perfil glicêmico de crianças e adolescentes obesos assintomáticos de Salvador, Brasil.
MétodoUma amostra de sangue venoso em jejum foi obtida de 90 indivíduos obesos consecutivos com idade entre 8-18 anos, de ambos os sexos, para determinações laboratoriais de hemoglobina glicosilada, insulina basal e Índice do Modelo de Avaliação da Homeostase de Resistência à Insulina (HOMA-IR). A avaliação clínica incluiu peso, estatura, circunferência da cintura, avaliação do desenvolvimento puberal e pesquisa sobre a acantose nigricans. Utilizamos o indicador de índice de massa corporal/idade referente à gravidade da avaliação de sobrepeso.
ResultadosAlterações glicêmicas foram comprovadas clínica e bioquimicamente, apesar de esses indivíduos não apresentarem queixas ou sintomas relacionados a níveis de açúcar no sangue. Variáveis quantitativas e qualitativas foram, respectivamente, medidas expressas de tendência central/dispersão e amostra/frequência relativa, utilizando o software Pacote Estatístico para as Ciências Sociais, versão 20.0. O valor de p<0,05 foi considerado significativo.
ConclusãoObservamos, contudo, alta prevalência de distúrbios de glicose e insulina em crianças e adolescentes obesos assintomáticos.
Obesity is a major change of nutritional metabolism, characterized by excessive fat deposition in the body, frequently observed in children and adolescents in worldwide. As a consequence, this population can develop adverse health effects favoring metabolic disorders such as dyslipidemia, hypertension, insulin resistance, glucose intolerance, and type 2 diabetes mellitus (T2DM).1
Although glycemic alterations in the obese are expected, T2DM is an infrequent comorbidity in children and adolescents.2 This possibility is strongly associated with the occurrence of prior events, such as hyperinsulinemia and insulin resistance,3 even considering how uncommon insulin resistance is in pre-pubertal children. Studies report the occurrence of peaks during pubertal period, becoming normal in adulthood.4 In fact, in a study performed with Brazilian children and adolescents without excess weight, age variation of insulin levels and the HOMA-IR indicator was demonstrated.5 Furthermore, these situations in obese pediatric patients require drug therapy before T2DM diagnosis has been established, in case of failure in lifestyle modification. This study used laboratory testing that is not part of the standard investigative routine in primary health care, in order to detect abnormalities that precede the diagnosis of T2DM in obesity. Thus, the purpose of this article is to present the evaluation of the glucose profile of asymptomatic obese children and adolescents.
Materials and methodsA cross-sectional study in 90 consecutive obese patients was conducted, aged 8–18 years, of both sexes, evaluated in a weekly pediatric nutrition outpatient screening at the Federal University of Bahia, Brazil, carried out from January to December 2015. All participants were only included if their Tanner criteria stage was normal for their age (Tanner stages I–IV).6 The body mass index (BMI) was calculated by dividing weight (kg) by the square of height (m2). The z-score of the indicator BMI/age (BMI/A) and gender was used to classify the anthropometric status of participants as obese (z-score >+2) or severely obese (z-score >+3).7 The dermatosis acanthosis nigricans (indicative of insulin resistance) was assessed in the neck, armpits, interphalangeal space, and flexor surfaces of the limbs. When present, it was classified as mild, moderate, or severe.8 Waist circumference was obtained with a soft and inelastic tape, at the midpoint between the last rib and the anterior iliac crest.9 Those who were using drugs that could interfere with glucose metabolism were excluded, as well as patients with conditions that predispose them to being overweight (Cushing's syndrome, growth hormone deficiency, hypothyroidism, syndromic obesity, and abnormal puberty pattern). This study was approved by the Ethics Committee of the Federal University of Bahia, Brazil. Children's verbal assent was obtained and a written informed consent was obtained from their legal representatives.
Laboratory analysesA fasting venous blood sample was taken of all participants for laboratory determinations, in a single moment. Fasting plasma glucose was assessed by the hexokinase method (Wiener Lab.). Glucose levels between 100–125mg/dL and ≥126mg/dL were, respectively, classified as glucose intolerance and T2DM. The glycated hemoglobin (HbA1C) levels were determined by the turbidimetry method HbA1C (TURBITEST AA, Wiener lab®, SP, Brazil). Normal reference values were 4.8%-5.9%. HbA1c values between 5.7% and 6.4% were considered as high risk for developing diabetes, and ≥6.5%, considered as probable diabetes mellitus (DM). American Diabetes Association10 diagnosis criteria were used for both parameters. The insulin levels were evaluated by enzyme-linked immunosorbent assay (ELISA). Any values greater than 15.0μUI/mL were considered abnormal.11 The Homeostasis Model Assessment-Insulin Resistance (HOMA-IR) index (fasting glucose [mg/dL]×fasting insulin [μIU/mL]/405) was used to identify insulin resistance.12 The cut-offs adjusted by gender and age according to Almeida et al. were used,5 summing the mean value to 2 standard deviations to determinate cutoffs.
Statistical analysesQuantitative and qualitative data were respectively expressed by measures of central tendency, dispersion, and simple/relative frequency. The chi-squared test compared the frequency of individuals in each category. Continuous variables were tested for normality of distribution by the Kolmogorov–Smirnov test. The differences for these variables were analyzed using the Mann–Whitney U-test or Student's t-test, according to their distribution. Statistical Program for Social Sciences (IBM SPSS Statistics for Windows, Version 20.0. NY, USA) was utilized for statistical analyses. A p-value <0.05 was considered significant.
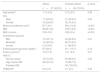
ResultsTable 1 show the main clinical and laboratory characteristics of this population. The fasting blood glucose ranged from 70.7 to 128.0mg/dL and was elevated in nine (10.0%) participants. One patient presented with glucose values above 126mg/dL. Insulin levels ranged from 2.5 to 52.9μUI/mL and were altered in 25 (27.8%) participants. As for HbA1c, the detected levels ranged from 4.2% to 6.8%, with 24 (26.6%) individuals presenting with abnormal values, six of them higher than 6.5%. The HOMA-IR index was abnormal in 47 (52.2%) participants. When comparing the group of severely obese and the obese group, a higher prevalence of insulin resistance was observed in the first group (65.4%; p<0.003).
Main clinical and laboratory characteristics of 90 asymptomatic obese children and adolescents in Salvador, Brazil.
| Obese | Severely obese | p-value | |
|---|---|---|---|
| n=27 (30.0%) | n=63 (70.0%) | ||
| Age (years)a | 11.4 (2.3) | 12.2 (2.9) | 0.28 |
| Sex | |||
| Male | 17 (64.6%) | 31 (35.4%) | 0.23 |
| Female | 10 (23.8%) | 32 (76.2%) | |
| Waist circumference (cm)a | 87.7 (9.1) | 98.3 (13.8) | <0.001 |
| BMI | 28.25 (3.5) | 33.57 (6.5) | <0.001 |
| BMI (z-score) | 2.52 (0.2) | 3.60 (0.8) | <0.001 |
| Acanthosis nigricans | |||
| Mild | 13 (35.1%) | 24 (64.9%) | 0.41 |
| Moderate | 12 (30.0%) | 28 (70.0%) | |
| Severe | 2 (15.4%) | 11 (84.6%) | |
| Fasting plasma glucose (mg/dL)a | 87.3(8.4) | 91.1 (10.1) | 0.15 |
| Insulin (μUI/mL)a | 12.0 (7.3) | 14.1 (9.5) | 0.51 |
| HbA1C | |||
| Normal values | 18 (31.6%) | 39 (68.4%) | 0.25 |
| High risk for DM | 09 (33.3%) | 18 (66.7%) | |
| Probably DM | – | 06 (100.0%) | |
| HOMA-IRa | 2.6 (1.6) | 3.1 (2.1) | 0.44 |
HOMA-IR, Homeostasis Model Assessment for Insulin Resistance; BMI, body mass index.
These results report a high prevalence of glucose metabolism and insulin abnormalities in this population of obese and severe obese children and adolescents, similarly to the findings described by D’Adamo and Caprio.13 It was also observed that almost 80% of the children and adolescents with severe obesity show altered glucose and insulin levels. In addition, this group also demonstrated the largest waist circumference measurements, regardless of age and sex. According to Martins and Marinho,14 visceral obesity is a leading cause of altered glucose/insulin homeostasis disorders. Thus, these findings reinforce the role of waist circumference as insulin resistance marker and an early predictor of T2DM.15 In this study, no association was detected between severe or moderate dermatosis acanthosis nigricans, severe obesity, and increased waist circumference.
Fasting blood glucose above the reference value was detected in nine cases. Surprisingly, in the case of an obese individuals (z score=+2.77), it was 126mg/dL and the HbA1c was in risk range for T2DM. The HbA1c values were higher than 6.5% in other six (9.5%) severely obese participants. These seven patients, therefore, show diabetes mellitus diagnostic parameters (prevalence of 7.8%). These tests were not repeated for confirmation.
The glycated hemoglobin reflects the degree of individual exposure to high glucose levels in the last 120 days. Although the proposed values of HbA1c in children and adolescents are not yet defined, values above 6.5% must be confirmed in another sample and waived in the event of symptoms or random blood glucose levels above 200mg/dL. Values between 5.7% and 6.4% are indicative of high risk for developing diabetes, according to the American Diabetes Association consensus, 2016.16
Hyperinsulinemia was observed in almost 30% of children and adolescents studied. These values could have been even greater if lower cutoff points were used, such as the European parameter, estimated at 12.6μIU/mL. However, this finding was not followed by abnormal increase in fasting glucose. These data are compatible with the pathophysiological compensatory process of high blood glucose levels that leads to increased insulin production, secondary to resistance to insulin action in the target organs. This is detected by a significant increase in the HOMA-IR index, an indicator of such condition. However, after a certain period, this compensatory increase in insulin is lost, resulting in hyperglycemia, featuring glucose intolerance, and eventually, T2DM.17 The current treatment with metformin for adolescents with documented insulin resistance, without the need of further laboratory diagnosis of DM, is recommended.18–20 However, this recommendation is not a consensus in literature, being used in an experimental way in selected patients.21
There is no consensus on the cut-off point to define insulin resistance. Some authors5,22,23 try to identify this cut-off by anthropometric measurements and metabolic indicators, among others, adjusted by age and sex. Cutoff values of approximately 3 are recommend to identify IR in children and adolescents.24–28
Similarly, the method used to determine insulin resistance is also controversial. In this study, HOMA-IR was used as a validated method for use in children and adolescents, easy to calculate when compared to quantitative insulin sensitivity check index (QUICKI) and for presenting values of measures that resemble those obtained with oral glucose tolerance test (OGTT) and hyperinsulinemic euglycemic clamp.5 Although considered gold standard, these methods present limitations, such as the high cost and the difficulty of execution, making it unfeasible to use them routinely, being used only in clinical studies.29
Insulin resistance may become an important predictor of the development of diabetes mellitus (DM) in the future. Two obese individuals presented abnormal levels of glucose and HOMA-IR, with normal HbA1c and insulin levels. The other detected changes were more prevalent among severely obese individuals. These results demonstrate a high prevalence of abnormal blood glucose, basal insulin, HOMA-IR, and HbA1c in obese children and adolescents. Nearly 8% of patients met established criteria for diabetes mellitus. However, the most important finding relates to the high prevalence of changes that precede DM in asymptomatic individuals with severe obesity. An important limitation of this study refers to cross-sectional design. Thus, a cause-effect relationship cannot be established between obesity and the abnormal glucose metabolism, although a significant association was observed between severe obesity and insulin resistance.
These results provide compelling evidence about the need to expand the laboratory investigation of these patients, with the inclusion of insulin and glycated hemoglobin measurement and HOMA-IR determination, beyond the isolated blood glucose level. Finally, these findings reinforce the need to develop programs for the effective prevention and intervention in childhood obesity, considering that diabetes is a chronic and deadly disease that can be detected by proper glycemic/insulinemic profiling of asymptomatic obese individuals, as part of the investigative routine.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Assunção SN, Boa Sorte NC, Alves CA, Mendes PS, Alves CR, Silva LR. Glucose alteration and insulin resistance in asymptomatic obese children and adolescents. J Pediatr (Rio J). 2018;94:268–72.