To determine if the efficacy of passive hypothermia and adverse events during transport are related to the severity of neonatal hypoxic-ischemic encephalopathy.
MethodsThis was a retrospective study of 67 infants with hypoxic-ischemic encephalopathy, born between April 2009 and December 2013, who were transferred for therapeutic hypothermia and cooled during transport.
ResultsFifty-six newborns (84%) were transferred without external sources of heat and 11 (16%) needed an external heat source. The mean temperature at departure was 34.4±1.4°C and mean transfer time was 3.3±2.0h. Mean age at arrival was 5.6±2.5h. Temperature at arrival was between 33 and 35°C in 41 (61%) infants, between 35°C and 36.5°C in 15 (22%) and <33°C in 11 (16%). Infants with severe hypoxic-ischemic encephalopathy had greater risk of having an admission temperature<33°C (OR: 4.5; 95% CI: 1.1–19.3). The severity of hypoxic-ischemic encephalopathy and the umbilical artery pH were independent risk factors for a low temperature on admission (p<0.05). Adverse events during transfer, mainly hypotension and bleeding from the endotracheal tube, occurred in 14 infants (21%), with no differences between infants with moderate or severe hypoxic-ischemic encephalopathy.
ConclusionThe risk of overcooling during transport is greater in newborns with severe hypoxic-ischemic encephalopathy and those with more severe acidosis at birth. The most common adverse events during transport are related to physiological deterioration and bleeding from the endotracheal tube. This observation provides useful information to identify those asphyxiated infants who require closer clinical surveillance during transport.
Determinar se a eficácia da hipotermia passiva e eventos adversos durante o transporte estão relacionados à gravidade da encefalopatia hipóxico-isquêmica neonatal.
MétodosEstudo retrospectivo de 67 neonatos com encefalopatia hipóxico-isquêmica (nascidos entre abril de 2009 e dezembro de 2013) transferidos para hipotermia terapêutica e resfriados durante o transporte.
ResultadosForam transportados 56 recém-nascidos (84%) sem fontes externas de calor e 11 (16%) precisaram de uma fonte externa de calor. A temperatura média na saída foi 34,4±1,4°C e o tempo médio de transporte foi 3,3±2,0 horas. A idade média na chegada foi 5,6±2,5 horas. A temperatura na chegada ficou entre 33-35°C em 41 (61%) neonatos, entre 35°-36,5°C em 15 (22%) e<33°C em 11 (16%). Neonatos com encefalopatia hipóxico-isquêmica grave apresentaram maior risco de temperatura < 33°C na internação (RC 4,5; IC de 95% 1,1-19,3). A gravidade da encefalopatia hipóxico-isquêmica e o pH da artéria umbilical foram fatores de risco independentes para uma baixa temperatura na internação (p<0,05). Eventos adversos durante o transporte, principalmente hipotensão e sangramento do tubo endotraqueal, ocorreram em 14 neonatos (21%), sem diferenças entre neonatos com encefalopatia hipóxico-isquêmica moderada ou grave.
ConclusãoO risco de super-resfriamento durante o transporte é maior em recém-nascidos com encefalopatia hipóxico-isquêmica grave e naqueles com acidose mais grave no nascimento. Os eventos adversos mais comuns durante o transporte estão relacionados a deterioração fisiológica e sangramento do tubo endotraqueal. Essa observação fornece informações úteis para identificar neonatos asfixiados que exigem maior vigilância clínica durante o transporte.
Hypoxic-ischemic encephalopathy (HIE) was once a disorder orphan of an effective therapy.1 It has become a time-dependent emergency, after clinical trials demonstrated the efficacy of cooling started within 6h of birth in reducing the risk of death or disability and increasing the rate of disability-free survival at 18–24 months of age.1–3 Animal models and infant studies have indicated that the earlier cooling is initiated after the injury, the more likely it is to be successful.4–6 Furthermore, experimental evidence has shown a lack of neuroprotective efficacy of hypothermia with delayed cooling.4,7
Most asphyxiated infants are born in non-tertiary neonatal units and they must be transferred urgently to a center equipped with a hypothermia program to start this therapy as soon as possible. In order not to delay the neuroprotection provided by cooling, it is recommended to begin this therapeutic intervention at the referring hospital before the transfer, by turning off the external sources of heat and keeping the infant cooled during transport.8–10
Most asphyxiated newborn infants being transferred are passively cooled. Several reports have studied the efficacy and safety of passive cooling during transport of asphyxiated newborns.9–16 Target temperatures are often not achieved and overcooling ranges from 11% to 34%.9–13 However, these studies do not outline medical complications during transport nor indicate whether the efficacy in maintaining target temperatures and complications are related to the severity of the HIE in the first 6h of life. The aim of the present study was to assess the relationship between the efficacy of passive hypothermia and adverse events during transport and the severity of the HIE.
MethodsDuring the five-year study period (January 2009–December 2013), the neonatal intensive care unit (NICU) of the Hospital Sant Joan de Deu – Hospital Clínic-Maternitat was one of the two regional centers offering therapeutic hypothermia for children with HIE born in Catalonia (32,000km2 territory, approximately 71,000 births per year). A coordinated program including both regional referral cooling centers and the pediatric transport service (Pediatric Emergency Medical System) was established in Catalonia in November 2009 for asphyxiated infants. The transport team includes a pediatrician, a pediatric nurse, and a driver/technician. The therapeutic hypothermia transport guideline establishes a target rectal temperature of 33–35°C and instructions for using the lowest possible dose of sedatives (fentanyl) if needed. Referring centers are instructed to remove external heat sources in asphyxiated infants. They are transferred in closed incubators, and rectal temperature is monitored every 15min. Infants with confirmed or suspected severe congenital disorder were excluded from the hypothermia protocol and they are not referred. The physicians who refer or transport the infant are in direct telephone contact with the referral NICU.
Data from all newborns≥34 weeks’ gestational age with HIE born at or transferred to this NICU (level IIIC) during the study period were collected and inserted into a prospective database. The database contains all records obtained during the transfer of outborn patients, including the temperatures after stabilization at birth, on departure from the referring center, during the transport (at least one every hour), and on admission to this unit. For this study, rectal temperatures at admission ranging from 33.0°C to 35.0°C were considered as in the target range, <33.0°C as overcooling, and from 35.0°C to 36.9°C as normothermic. Transport records were reviewed to assess noteworthy events occurring during transport. Adverse events were classified as (a) untoward incidents related to intensive care (e.g. accidental extubation, occlusion of endotracheal tube, and exhaustion of oxygen supply), or (b) physiological deterioration related to critical illness (e.g., worsening hypotension and increased inotropic support or hypoxemia, hypoglycemia, cardiac arrhythmia, major bleeding, and need for cardiopulmonary resuscitation).
On arrival at this unit, infants were considered to have HIE if they met the following criteria: (1) Apgar score≤5 at 10min, or need for resuscitation, including endotracheal intubation or mask ventilation for more than 10min after birth, or acidosis (pH≤7.0 and/or base deficit≥16mmol/L in umbilical cord blood or arterial, venous, or capillary blood) within 60min from birth; (2) neonatal encephalopathy, defined as a syndrome of neurologic dysfunction manifested by a subnormal level of consciousness with or without seizures (moderate or severe HIE) or palmary hyperexcitability, tremor, overactive myotatic reflexes, hypersensitivity to stimulation, or startle responses.17 Continuous aEEG recordings for 72h were initiated immediately after admission.
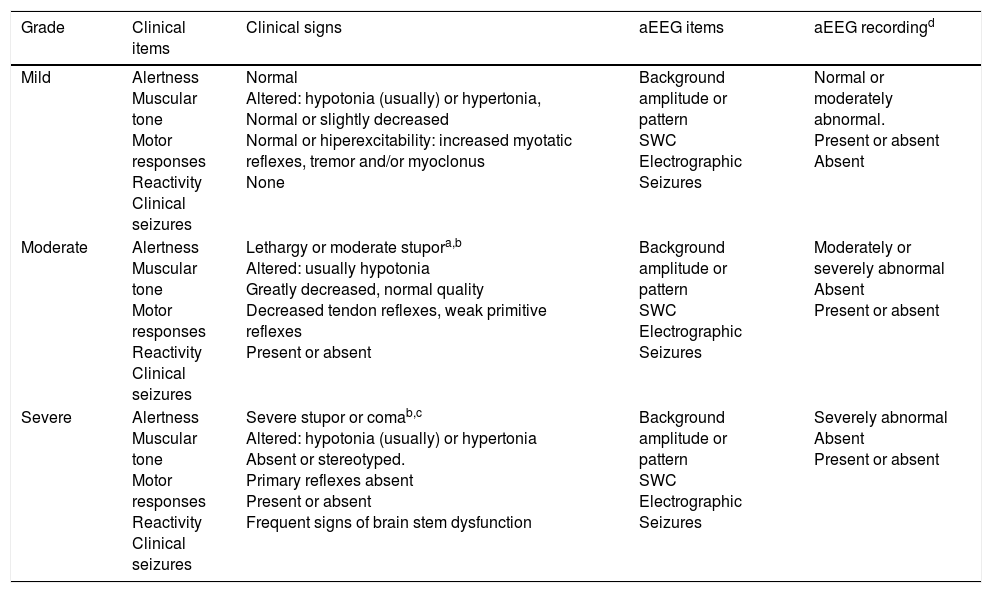
The severity of HIE was assessed immediately after admission and always before starting therapeutic hypothermia in the NICU. Encephalopathy was classified as mild, moderate, and severe in accordance with the semi-quantitative score which included the aEEG findings (Table 1).18,19 Infants who were sedated during the transfer were maintained in passive cooling for at least 3h in order to reduce the possible effect of the sedative on the neurological state. Then, an additional clinical examination and grading of HIE was performed. Newborns with moderate or severe HIE received whole-body cooling (Technotherm® TSmed 200 N, SP, Brazil or Criticool, MTRE Ltd, Israel.) and were maintained at a rectal temperature of 33.5°C for 72h, following which they were slowly rewarmed (≤0.5°C per hour). A systematic research protocol was followed in all patients with HIE transferred to or born in this hospital.
Scoring system for hypoxic-ischemic encephalopathy.
| Grade | Clinical items | Clinical signs | aEEG items | aEEG recordingd |
|---|---|---|---|---|
| Mild | Alertness Muscular tone Motor responses Reactivity Clinical seizures | Normal Altered: hypotonia (usually) or hypertonia, Normal or slightly decreased Normal or hiperexcitability: increased myotatic reflexes, tremor and/or myoclonus None | Background amplitude or pattern SWC Electrographic Seizures | Normal or moderately abnormal. Present or absent Absent |
| Moderate | Alertness Muscular tone Motor responses Reactivity Clinical seizures | Lethargy or moderate stupora,b Altered: usually hypotonia Greatly decreased, normal quality Decreased tendon reflexes, weak primitive reflexes Present or absent | Background amplitude or pattern SWC Electrographic Seizures | Moderately or severely abnormal Absent Present or absent |
| Severe | Alertness Muscular tone Motor responses Reactivity Clinical seizures | Severe stupor or comab,c Altered: hypotonia (usually) or hypertonia Absent or stereotyped. Primary reflexes absent Present or absent Frequent signs of brain stem dysfunction | Background amplitude or pattern SWC Electrographic Seizures | Severely abnormal Absent Present or absent |
SWC, sleep-wake cycle.
Lethargy; difficulty to wake up to noxious stimuli and when awake up maintains the alertness a few seconds (≤6″).
The worst aEEG segment of 30min to 1h in length before clinical evaluation. Grading: Normal trace: normal continuous voltage pattern (upper margin >10μV and lower margin >5μV); Moderately abnormal trace: discontinuous pattern (upper margin >10μV and lower margin ≤5μV). Severely abnormal trace: burst suppression pattern (upper margin <10μV and lower margin <5μV; often accompanied by bursts of high voltage activity), continuous low voltage (upper margin <10μV and lower margin <5μV), or isoelectric pattern (upper and lower margin <5μV, with no burst of activity).
Continuous variables were compared using Student's t-test, Mann–Whitney's U test, or the non-parametric Kruskall–Wallis test, as appropriate. Categorical variables were compared using the χ2 test or Fisher's exact test. The linear relationship between different variables and the departure, transport, and admission temperatures was evaluated using Pearson's (r) or Spearman's (rs) correlation coefficient. In order to study temperature curves according to HIE severity group, the General linear mixed model was used. Linear regression analysis was performed to adjust for the effect of confounding factors using binomial regression models. Relative risks (RR) adjusted were estimated using Poisson regression with robust error variance. A p-value of <0.05 was considered to indicate significance. All statistical analyses were performed using SPSS version 17 (SPSS Inc. – Chicago, IL, USA).
EthicsThe hospital ethics committee approved this study, and the parents’ permission was obtained in all cases prior to inclusion in the study.
ResultsFrom January 2009 to December 2013, 99 patients with HIE were attended in this unit, 68 of whom were referred for possible treatment with therapeutic hypothermia. Sixty-seven were transferred by the Pediatric Emergency Medical System of Catalonia. All were transferred by road ambulance, except for one who was born in the Balearic Islands and transferred by helicopter. One patient, who was born at home and transferred by a non-pediatric team, was excluded from the study.
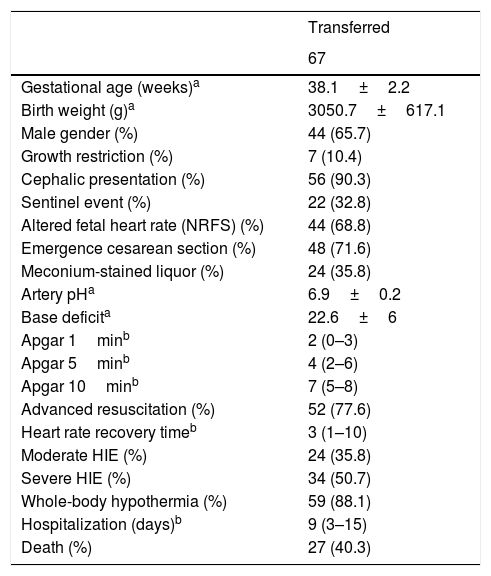
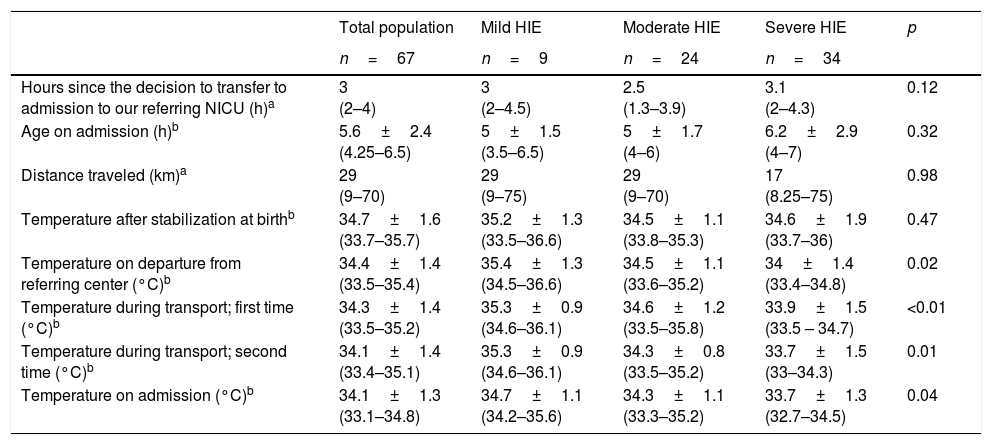
Perinatal data of the 67 infants transferred are shown in Table 2. All patients were passively cooled in their centers until the transport team arrived. Table 3 presents the median time from the decision to transfer to admission to this NICU; age on admission; distance traveled; and the temperatures after stabilization at birth, on departure from the referring center, during transport, and on arrival at this Unit. The mean distance traveled was 49±54km, and the longest was 172km, except for the patient transferred from the Balearic Islands (283km) by helicopter. There were no significant differences between the temperature on departure from the referring centers and the temperature on arrival at this unit (34.5±1.5 vs. 34.1±1.3°C; p=0.7).
Perinatal data of the newborns with hypoxic-ischemic encephalopathy transferred to this NICU.
| Transferred | |
|---|---|
| 67 | |
| Gestational age (weeks)a | 38.1±2.2 |
| Birth weight (g)a | 3050.7±617.1 |
| Male gender (%) | 44 (65.7) |
| Growth restriction (%) | 7 (10.4) |
| Cephalic presentation (%) | 56 (90.3) |
| Sentinel event (%) | 22 (32.8) |
| Altered fetal heart rate (NRFS) (%) | 44 (68.8) |
| Emergence cesarean section (%) | 48 (71.6) |
| Meconium-stained liquor (%) | 24 (35.8) |
| Artery pHa | 6.9±0.2 |
| Base deficita | 22.6±6 |
| Apgar 1minb | 2 (0–3) |
| Apgar 5minb | 4 (2–6) |
| Apgar 10minb | 7 (5–8) |
| Advanced resuscitation (%) | 52 (77.6) |
| Heart rate recovery timeb | 3 (1–10) |
| Moderate HIE (%) | 24 (35.8) |
| Severe HIE (%) | 34 (50.7) |
| Whole-body hypothermia (%) | 59 (88.1) |
| Hospitalization (days)b | 9 (3–15) |
| Death (%) | 27 (40.3) |
Values are presented as total value (percentage).
General transport data and temperature (°C) on departure, during transport and on admission.
| Total population | Mild HIE | Moderate HIE | Severe HIE | p | |
|---|---|---|---|---|---|
| n=67 | n=9 | n=24 | n=34 | ||
| Hours since the decision to transfer to admission to our referring NICU (h)a | 3 (2–4) | 3 (2–4.5) | 2.5 (1.3–3.9) | 3.1 (2–4.3) | 0.12 |
| Age on admission (h)b | 5.6±2.4 (4.25–6.5) | 5±1.5 (3.5–6.5) | 5±1.7 (4–6) | 6.2±2.9 (4–7) | 0.32 |
| Distance traveled (km)a | 29 (9–70) | 29 (9–75) | 29 (9–70) | 17 (8.25–75) | 0.98 |
| Temperature after stabilization at birthb | 34.7±1.6 (33.7–35.7) | 35.2±1.3 (33.5–36.6) | 34.5±1.1 (33.8–35.3) | 34.6±1.9 (33.7–36) | 0.47 |
| Temperature on departure from referring center (°C)b | 34.4±1.4 (33.5–35.4) | 35.4±1.3 (34.5–36.6) | 34.5±1.1 (33.6–35.2) | 34±1.4 (33.4–34.8) | 0.02 |
| Temperature during transport; first time (°C)b | 34.3±1.4 (33.5–35.2) | 35.3±0.9 (34.6–36.1) | 34.6±1.2 (33.5–35.8) | 33.9±1.5 (33.5 – 34.7) | <0.01 |
| Temperature during transport; second time (°C)b | 34.1±1.4 (33.4–35.1) | 35.3±0.9 (34.6–36.1) | 34.3±0.8 (33.5–35.2) | 33.7±1.5 (33–34.3) | 0.01 |
| Temperature on admission (°C)b | 34.1±1.3 (33.1–34.8) | 34.7±1.1 (34.2–35.6) | 34.3±1.1 (33.3–35.2) | 33.7±1.3 (32.7–34.5) | 0.04 |
HIE, hypoxic-ischemic encephalopathy.
Out of 67 infants referred, 56 (84%) were managed without any external heat source throughout transport, 11 (16%) needed an external heat source to prevent excessive cooling, and only one child who had fever needed to be cooled with cold water bags. Temperature on departure, during transport, or on arrival to this Unit were not related to the following perinatal variables: intrapartum sentinel event (i.e. uterine rupture, placental abruption, cord prolapse or amniotic fluid embolism), meconium-stained fluid, Apgar scores, and advanced resuscitation. However, emergency cesarean section, umbilical artery pH, and severe HIE were correlated with temperature on departure and on arrival at this NICU.
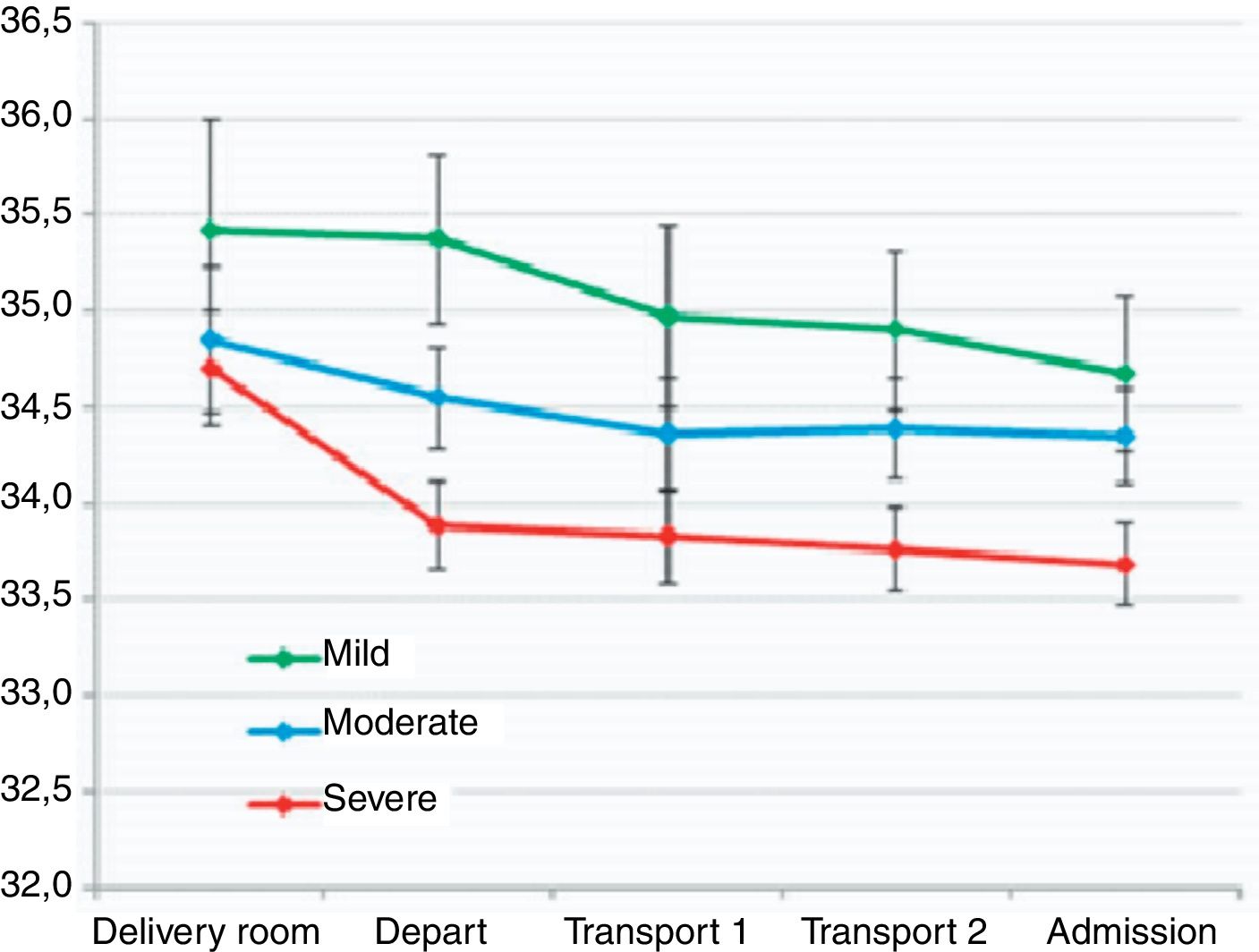
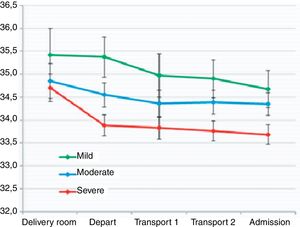
When stratifying by HIE severity, no significant differences were observed in temperature after stabilization at birth, time between the decision to transfer and admission, nor in age at admission. A correlation was observed between the temperature on departure and the temperature on admission to this hospital in infants with moderate (rs 0.65; p<0.01) and severe HIE (rs 0.745; p<0.001), but not in infants with mild HIE (rs 0.58; p=0.1). There were differences in rectal temperature on departure, during transport, and on arrival at this NICU according to the severity of HIE (Table 3, Fig. 1). In a stepwise regression analysis, the association between temperature on departure from the referring center and on arrival at this NICU remained significant regarding umbilical artery pH (B1.62; p<0.05 and 1.65; p<0.05, respectively) and severe HIE (B-0.96; p<0.05 and −0.72; p<0.05, respectively), after adjusting for birth weight, advanced resuscitation, and Apgar scores. When adjusting for all perinatal variables and transfer time, the subgroup of patients with severe HIE had a departure temperature 0.9°C lower than the other groups, as well as a 0.7°C lower arrival temperature. Infants with severe HIE had a greater risk of having temperature <33°C on admission (RR 4.5; 95% CI: 1.1–19.3).
Almost half (46%) of the transferred patients were sedated during transport. No significant associations were observed between sedation and the severity of HIE nor with the temperature on admission. Infants with severe HIE most often received inotropic support (21/27, 77.7%; p<0.001) and mechanical ventilation (28/45, 62%; p<0.01). Noteworthy events during transport were reported in 14 (21%) infants. A trend toward more complications or comorbidities during transport was observed in infants with severe HIE (29% vs. 12%; p=0.082). The main adverse event was physiological deterioration during transport (13/14), mainly hypotension and need for increased inotropic support with or without fluid expansion (7/14), hypoglycemia and need for glucose bolus (4/14), and bleeding from the endotracheal tube with desaturation (3/14), but only one patient needed to have the tube changed due to occlusion. One patient suffered cardiorespiratory arrest, requiring advanced resuscitation.
Of the 67 transferred infants, therapeutic hypothermia was finally applied to 59 (88%). Four infants with mild HIE were not cooled, and four infants with severe HIE did not receive therapeutic hypothermia, three due to a moribund state on admission and one due to arrival at more than 8h of age.
DiscussionIn this study, a strong negative association was observed between temperatures on departure from referring centers, during transport, and on arrival of asphyxiated infants at this NICU, and the severity of neonatal HIE and umbilical arterial cord pH.
A significant proportion of asphyxiated infants requiring therapeutic hypothermia for moderate or severe HIE are born outside centers equipped to provide it. The Spanish Society of Neonatology recommends the transfer of such neonates to hospitals that provide tertiary care including therapeutic hypothermia.20 Response time and transport time are not low enough, as HIE treatment is time-dependent, given the urgency to establish therapeutic hypothermia within 6h of birth. While it could be expected that the timeframes to referral to NICU would be greater in infants with mild or moderate HIE, the present data provide no evidence of substantial variation in timeframes to NICU referral depending on the severity of HIE. There are currently no evidence-based guidelines for the provision of cooling during transport of neonates with suspected HIE. Because there is limited evidence to support servo-controlled cooling during transport,10,11,16 nowadays most infants with HIE are transferred with passive cooling.9,10 In the present study, one-third of the infants who were passively cooled before and during transport were outside the target temperature range (33–35°C) upon arrival at the referral center. A similar ratio has been reported in some studies,13,15 but it was clearly lower than others reporting more than 70% of infants with temperatures outside the target range.14,16
The incidence of overcooling with passive hypothermia ranges from 11% to 34%,12–14,16,21 and it is higher than that observed when using servo-controlled cooling in neonatal transport (<11%).12,16 The present data are consistent with prior studies that demonstrated the safety of passive cooling, with a low rate of overcooling (16%) and complications (21%) during transport.13,15 Most neonates with HIE were transferred by road; although the distances were relatively short, the present overcooling rate was lower than those reported in other studies with patients covering shorter distances of transport.12,14,16 In these studies, over one-third of infants passively cooled were overcooled at admission. The lower rate of overcooling during transport observed in the present might be related to the regional guidelines for the referral centers and pediatric transport team, which recommend vigilant temperature control before referral and during transport. It is not known whether the rate of infants with severe HIE transferred was higher in the aforementioned studies.
Due to the range of severity of HIE of the patients transferred to this NICU, it was possible to analyze which factors were related with temperature during transport, providing unique and important insights about it. Umbilical artery pH and severity of HIE were the independent factors related with temperature on departure, during transport, and on admission, after adjusting for birth weight, advanced resuscitation, Apgar scores, and transfer time. The subgroup of patients with severe HIE showed a departure temperature 0.9°C lower than the other groups, as well as a 0.7°C lower arrival temperature. In the entire cohort of infants passively cooled during transport, overcooling was observed mostly in infants with severe HIE. It must be stressed that, in the present study, HIE severity was determined following a common scale supervised in every case by neonatologists with specific expertise in neonatal neurology, and that the clinical examination was supported in all cases by aEEG findings, which have been correlated with neurodevelopment outcome.22,23
It has been known for more than 50 years that asphyxiated infants lose temperature at a higher rate than their non-asphyxiated peers, in relation to reduced oxygen consumption and energy production.24,25 Asphyxiated neonates with hypoxemia cannot produce an adequate amount of heat to increase their temperature, and there is an active drop mechanism of thermoregulation.26,27 In 1958, Burnard & Cross reported that infants with asphyxia (defined as failure to establish respiration within three minutes of birth) presenting lower rectal temperatures, taking 18h to achieve temperatures similar to healthy infants.25 Similar data were reported by Robertson et al., who noticed that asphyxiated infants not exposed to hypothermia took 15.6±14.6h to achieve normothermia. The failure of the thermal adaptive response, “natural cooling”, is used to achieve passive cooling before and during neonatal transfer period.28 The impaired heat production should be more consistent after severe hypoxic-ischemic injury; this is indirectly supported by the present finding of a relationship between the umbilical artery pH and the severity of HIE and the temperature on departure, during transport, and on admission.
It is difficult to compare the rate of adverse events during transport of infants with HIE in passive hypothermia observed in the present study. It is not possible to elucidate whether adverse events reported would appear equally in infants transported non-passively cooled or in those actively cooled. O’Reilly et al. did not find differences in adverse events between newborns with and without passive hypothermia during transport.15 Akula et al. reported only a pulmonary hemorrhage and two device-related events, and they did not provide a full list of adverse events and differences between both groups, passively and actively cooled infants.11 In addition, factors that limit adverse events during transport, such as regular patient and equipment checks during transport, meticulous preparation of the patient, adapted sedation, use of protocols, and the level of education and experience of the teams, can differ in each geographic area. Nevertheless, the present study demonstrated that physiological deterioration, mainly hypotension and hypoglycemia, as well as bleeding from the endotracheal tube with desaturation, should be anticipated in patients with HIE transferred in passive hypothermia.
A limitation of the present study is its retrospective design; some additional unspecified data may have been overlooked and the reliability of the data recorded during transport could have been limited by the accuracy of patient transport records and narrative notes. Furthermore, a size effect (type II error) may have limited reaching a conclusion about whether children with severe HIE show more complications during transport. Pre-transport severity of the patients was not established as it is usual in pediatric transport (Pediatric Risk of Mortality score),29 and the severity of HIE was determined after arrival of asphyxiated infants at this NICU; therefore; it is not possible to rule out some degree of worsening of neurological status during transport. In addition, it is not possible to predict if efficacy would have been different in this sample if hypothermia-controlling devices had been used during transport. Other studies have revealed a greater number of infants who achieve target temperature when controlled hypothermia is used during transport.11,16
This study shows that the risk of overcooling during transport with passive hypothermia is higher in newborns with severe HIE and in those who had more severe acidosis at birth. This observation provides useful information to identify those asphyxiated infants who require closer clinical surveillance to ensure temperatures in the target range during transport. The most common adverse events that arise during the transport of infants with HIE with passive hypothermia are mainly related with physiological deterioration and bleeding from the endotracheal tube with desaturation.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Ms. Elia Pérez for her statistical analysis of the data and the team of Pediatric Emergency Medical System in Catalonia.
Please cite this article as: Carreras N, Alsina M, Alarcon A, Arca-Díaz G, Agut T, García-Alix A. Efficacy of passive hypothermia and adverse events during transport of asphyxiated newborns according to the severity of hypoxic-ischemic encephalopathy. J Pediatr (Rio J). 2018;94:251–7.