To systematize information about vitamin E concentration in human milk and the variables associated with this composition in order to find possible causes of deficiency, supporting strategies to prevent it in postpartum women and infants.
SourceStudies published between 2004 and 2014 that assayed alpha-tocopherol in human milk of healthy women by high performance liquid chromatography were evaluated. The keywords used were “vitamin E”, “alpha-tocopherol”, “milk, human”, “lactation”, and equivalents in Portuguese, in the BIREME, CAPES, PubMed, SciELO, ISI Web of Knowledge, HighWire Press, Ingenta, and Brazilian Digital Library of Theses and Dissertations databases.
Summary of the findingsOf the 41 publications found on the subject, 25 whose full text was available and met the inclusion criteria were selected. The alpha-tocopherol concentrations found in milk were similar in most populations studied. The variable phase of lactation was shown to influence vitamin E content in milk, which is reduced until the mature milk appears. Maternal variables parity, anthropometric nutritional status, socioeconomic status, and habitual dietary intake did not appear to affect the alpha-tocopherol levels in milk. However, the influence of the variables maternal age, gestational age, biochemical nutritional status in alpha-tocopherol, and maternal supplementation with vitamin E had conflicting results in the literature.
ConclusionAlpha-tocopherol concentration in milk decreases during lactation, until the mature milk appears. To confirm the influence of some maternal and child variables on milk vitamin E content, further studies with adequate design are needed.
Sistematizar informações sobre a concentração de vitamina E no leite humano e variáveis associadas a essa composição, a fim de encontrar possíveis causas de deficiência, subsidiando estratégias para prevenção desta em puérperas e lactentes.
Fonte dos dadosForam avaliados estudos publicados entre 2004 e 2014 que determinaram o alfa-tocoferol no leite humano de mulheres saudáveis por Cromatografia Líquida de Alta Eficiência. Os descritores utilizados foram “leite humano”, “alfa-tocoferol”, “vitamina E”, “lactação” e seus equivalentes em inglês, nas bases de dados BIREME, Periódicos CAPES, PubMed, SciELO, ISI Web of Knowledge, HighWire Press, Ingenta e Biblioteca Digital Brasileira de Teses e Dissertações.
Síntese dos dadosDas 41 publicações encontradas sobre a temática, 25 foram selecionadas, por possuirem texto completo disponível e se encaixarem nos critérios de inclusão. As concentrações encontradas de alfa-tocoferol no leite foram semelhantes na maioria das populações estudadas. A variável fase de lactação mostrou influenciar o conteúdo dessa vitamina no leite, que vai sendo reduzido até o leite maduro. As variáveis maternas paridade, estado nutricional antropométrico, condição socioeconômica e ingestão dietética habitual parecem não afetar os níveis de alfa-tocoferol no leite. Entretanto, a influência das variáveis idade materna, idade gestacional, estado nutricional bioquímico em alfa-tocoferol e suplementação materna com vitamina E possui resultados conflitantes na literatura.
ConclusãoA concentração de alfa-tocoferol no leite diminui durante a lactação, até chegar ao leite maduro. Para confirmar a influência de algumas variáveis maternas e da criança sobre a vitamina E do leite ainda são necessários mais estudos, com desenho adequado.
Alpha-tocopherol, the main component of a group of compounds known as vitamin E, is a powerful antioxidant and the main fat-soluble vitamin responsible for protecting cell membranes against peroxidation. As a lipophilic compound, it accumulates in circulating lipoproteins, cell membranes, and fatty deposits, reacting with free radicals and molecular oxygen, protecting polyunsaturated fatty acids (PUFAs) and lipoproteins from peroxidation.1,2
This vitamin is extremely important in the early stages of life, from conception to postnatal development. During pregnancy, placental transfer of vitamin E to the fetus is limited, making breast milk the only source of this nutrient for infants that are exclusively breastfed. This intake represents an important way to supply the newborn with an essential antioxidant protection and stimulate immune system development.3
Considering the importance of vitamin E for the newborn, many studies aimed to determine the levels of alpha-tocopherol in breast milk. However, the literature presents conflicting data regarding this level, such as those found by Schweigert et al.4 in German women, who observed alpha-tocopherol levels in the colostrum that were two-fold higher than those found in Bangladeshi women.5
These differences may be due to some factors that can cause changes in the concentration of alpha-tocopherol in milk. Nascimento and Issler6 highlight that changes in the nutritional composition of milk depend on the stage of lactation, time of the day, time since last meal, nutrition, maternal age, gestational age of the newborn, and other individual maternal aspects.
Studies on the association of variables with alpha-tocopherol content in human milk have been performed. Therefore, considering the importance of vitamin E and the breast milk for the newborn and the different findings in the literature about this subject, this review aimed to systematize information on the levels of alpha-tocopherol in human milk and variables associated with this concentration, in order to clarify which factors influence the composition of vitamin E in milk.
MethodsStudies published between January of 2004 and February of 2014 in the BIREME, CAPES journals, PubMed, SciELO, ISI Web of Knowledge, HighWire Press, Ingenta, and Brazilian Digital Library of Theses and Dissertations databases were searched. In order to find studies pertaining to the subject of interest, specific descriptors were used during the research: human milk, alpha-tocopherol, vitamin E, lactation, and their Portuguese equivalents.
Publications whose title or summary indicated they were studies on the levels of alpha-tocopherol in human milk were selected to be read in full. The review included only studies that used high performance liquid chromatography (HPLC) to determine alpha-tocopherol levels. Studies performed with non-healthy women were excluded, as well as those found on the topic, which although disclosed the levels of alpha-tocopherol obtained by the analysis of human milk, had as main objective to study vitamin loss processes, determination methods, among others, rather than the concentration of this nutrient in milk.
The variables considered for the review on their association with alpha-tocopherol content in milk were identified through the literature review. Thus, the variables selected were those most commonly used in the studies: stage of lactation (colostrum, transitional, and mature milk); maternal age; socioeconomic status; parity; gestational age of the newborn; biochemical nutritional status of maternal vitamin E; maternal anthropometric nutritional status; maternal habitual dietary intake; and supplementation with vitamin E.
Lactation stageColostrum milk is the first milk secretion, which remains until the seventh or tenth day postpartum. It is a thick liquid of high density and generally yellowish in color due to its high content of carotenoids. This milk is also rich in antibodies, protecting the baby against infections, and has the property of facilitating the establishment of a predominantly bifid intestinal flora and laxative effect, which aids in the elimination of meconium.6 Studies have demonstrated the protective effect of breastfeeding with colostrum milk within the first hour of life in fighting neonatal mortality, pointing to the importance of this practice immediately after delivery.7
Around the eight and up to the 15th day postpartum, the milk is called “transitional milk”, and changes in its composition continue to occur, until approximately two weeks postpartum, when the milk composition becomes more stable, thus being characterized as mature milk.6
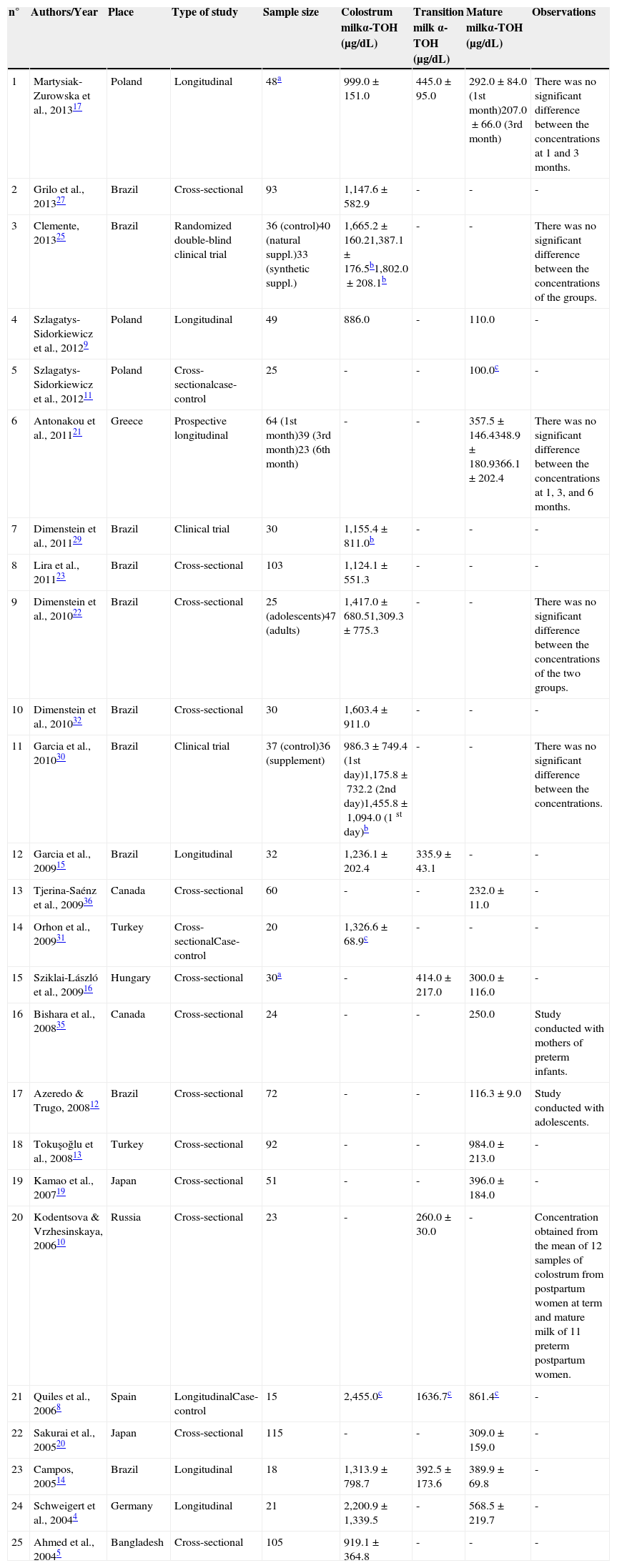
The concentration of alpha-tocopherol in colostrum milk in most of the studied populations is similar; however, some results diverge from the mean found by the others, such as the studies conducted in Germany4 and Spain,8 in which the values of the vitamin in the colostrum were much higher than those observed in Bangladesh5 and Poland,9 for instance. In the first two studies, however, it is emphasized that the sample size was small, and that the German study4 found a variation in the composition of alpha-tocopherol in milk, as demonstrated by the standard deviation (Table 1). Therefore, it would be interesting to study a greater number of lactating to confirm these values.
Studies on the concentration of alpha-tocopherol (μg dL) in breast milk at different stages of lactation published between 2004-2014, ordered by year of publication.
| n° | Authors/Year | Place | Type of study | Sample size | Colostrum milkα-TOH (μg/dL) | Transition milk α-TOH (μg/dL) | Mature milkα-TOH (μg/dL) | Observations |
|---|---|---|---|---|---|---|---|---|
| 1 | Martysiak-Zurowska et al., 201317 | Poland | Longitudinal | 48a | 999.0±151.0 | 445.0±95.0 | 292.0±84.0 (1st month)207.0±66.0 (3rd month) | There was no significant difference between the concentrations at 1 and 3 months. |
| 2 | Grilo et al., 201327 | Brazil | Cross-sectional | 93 | 1,147.6±582.9 | - | - | - |
| 3 | Clemente, 201325 | Brazil | Randomized double-blind clinical trial | 36 (control)40 (natural suppl.)33 (synthetic suppl.) | 1,665.2±160.21,387.1±176.5b1,802.0±208.1b | - | - | There was no significant difference between the concentrations of the groups. |
| 4 | Szlagatys-Sidorkiewicz et al., 20129 | Poland | Longitudinal | 49 | 886.0 | - | 110.0 | - |
| 5 | Szlagatys-Sidorkiewicz et al., 201211 | Poland | Cross-sectionalcase-control | 25 | - | - | 100.0c | - |
| 6 | Antonakou et al., 201121 | Greece | Prospective longitudinal | 64 (1st month)39 (3rd month)23 (6th month) | - | - | 357.5±146.4348.9±180.9366.1±202.4 | There was no significant difference between the concentrations at 1, 3, and 6 months. |
| 7 | Dimenstein et al., 201129 | Brazil | Clinical trial | 30 | 1,155.4±811.0b | - | - | - |
| 8 | Lira et al., 201123 | Brazil | Cross-sectional | 103 | 1,124.1±551.3 | - | - | - |
| 9 | Dimenstein et al., 201022 | Brazil | Cross-sectional | 25 (adolescents)47 (adults) | 1,417.0±680.51,309.3±775.3 | - | - | There was no significant difference between the concentrations of the two groups. |
| 10 | Dimenstein et al., 201032 | Brazil | Cross-sectional | 30 | 1,603.4±911.0 | - | - | - |
| 11 | Garcia et al., 201030 | Brazil | Clinical trial | 37 (control)36 (supplement) | 986.3±749.4 (1st day)1,175.8±732.2 (2nd day)1,455.8±1,094.0 (1 st day)b | - | - | There was no significant difference between the concentrations. |
| 12 | Garcia et al., 200915 | Brazil | Longitudinal | 32 | 1,236.1±202.4 | 335.9±43.1 | - | - |
| 13 | Tjerina-Saénz et al., 200936 | Canada | Cross-sectional | 60 | - | - | 232.0±11.0 | - |
| 14 | Orhon et al., 200931 | Turkey | Cross-sectionalCase-control | 20 | 1,326.6±68.9c | - | - | - |
| 15 | Sziklai-László et al., 200916 | Hungary | Cross-sectional | 30a | - | 414.0±217.0 | 300.0±116.0 | - |
| 16 | Bishara et al., 200835 | Canada | Cross-sectional | 24 | - | - | 250.0 | Study conducted with mothers of preterm infants. |
| 17 | Azeredo & Trugo, 200812 | Brazil | Cross-sectional | 72 | - | - | 116.3±9.0 | Study conducted with adolescents. |
| 18 | Tokuşoğlu et al., 200813 | Turkey | Cross-sectional | 92 | - | - | 984.0±213.0 | - |
| 19 | Kamao et al., 200719 | Japan | Cross-sectional | 51 | - | - | 396.0±184.0 | - |
| 20 | Kodentsova & Vrzhesinskaya, 200610 | Russia | Cross-sectional | 23 | - | 260.0±30.0 | - | Concentration obtained from the mean of 12 samples of colostrum from postpartum women at term and mature milk of 11 preterm postpartum women. |
| 21 | Quiles et al., 20068 | Spain | LongitudinalCase-control | 15 | 2,455.0c | 1636.7c | 861.4c | - |
| 22 | Sakurai et al., 200520 | Japan | Cross-sectional | 115 | - | - | 309.0±159.0 | - |
| 23 | Campos, 200514 | Brazil | Longitudinal | 18 | 1,313.9±798.7 | 392.5±173.6 | 389.9±69.8 | - |
| 24 | Schweigert et al., 20044 | Germany | Longitudinal | 21 | 2,200.9±1,339.5 | - | 568.5±219.7 | - |
| 25 | Ahmed et al., 20045 | Bangladesh | Cross-sectional | 105 | 919.1±364.8 | - | - | - |
α-TOH, alpha-tocopherol.
In the case of Bangladesh, the observed concentration may be due to the characteristics of the study population, i.e., extremely poor women with very bad health indicators, which makes them more prone to the development of nutritional deficiencies. However, despite the lower levels of this nutrient in the milk of these women, that study demonstrated that this amount is sufficient to meet the nutritional requirements of the infant. According to Ahmed et al.,5 this fact can be explored to promote colostrum feeding in developing countries such as Bangladesh, where a certain rejection of that milk has been recorded.
In transition milk, the values found in different populations were also similar, with the exception of one study conducted in Russia,10 which presented lower mean values, as well as the study by Quiles et al.,8 whose values were higher than others. Kodentsova and Vrzhesinskaya,10 however, used samples of women who were between the third and tenth days of lactation together with others, who were between the 14th and 20th days, which may have influenced the results.
In mature milk, Polish studies9,11 have also observed lower values when compared to others. The same was observed in a group of Brazilian adolescents, demonstrating that age influences the content of vitamin E in breast milk, according to the authors.12 Another observation in relation to mature milk refers to the study conducted by Tokuşoğlu et al.13 in Turkey, which showed levels of alpha-tocopherol that were similar to those in colostrum milk. Quiles et al.,8 in Spain, also showed results that were higher than the mean values for this milk; but this value refers to only 15 women and the small sample size may have influenced the results.
Table 1 shows that there is a downward trend in the content of alpha-tocopherol secreted in breast milk over the course of lactation stages, being higher in colostrum.4,8,9,14–17 According to Debier,3 these changes occur due to the increase in fat globules as the milk matures. After the first days of lactation, triglyceride synthesis in the mammary gland and its secretion in milk increase, without a proportional increase in the secretion of phospholipids and other components of the globule membrane.
Therefore, there is a significant reduction in the amount of some components of the fat globule, including alpha-tocopherol, since most of the vitamin E is secreted as a constituent of the membrane of these globules.
Although the amount of alpha-tocopherol offered to the infant is higher at the phase of colostrum milk when compared to transitional and mature milk, there is an increase in the volume of milk ingested by the newborn with time, in order to meet the infant's nutritional needs. However, Garcia et al.15 observed that the concentration of alpha-tocopherol, considering the infant's need (4mg/day)18 and the daily consumption of 780mL/day of milk, indicates an apparent nutritional inadequacy of transitional milk in their study, conducted in Northeastern Brazil. Considering this fact, it has been observed that other studies also showed this possible insufficient supply, when analyzing the content of alpha-tocopherol in transitional and mature milk.
Some authors have studied the content of alpha-tocopherol in breast milk in order to help establish a DRI (Dietary Reference Intake) for infants.19,20 It is known that the recommendation of 4mg/day of vitamin E for children aged 0 to 6 months was estimated according to the mean intake of this nutrient through consumption of human milk by the infants. Moreover, it is an adequate intake (AI), which is the mean value estimated when the recommended dietary intake (RDA) has yet to be established.18 Traber1 states that the amount of vitamin E recommended for daily intake is still controversial, and several organizations have proposed different values.
Thus, it is necessary to review the recommendations for this vitamin to verify whether there is an overestimation of this requirement, as breast milk is considered a nutritionally complete food and no clinical signs of vitamin E deficiency are observed in healthy full-term children fed exclusively breast milk.
At the mature milk stage, when this secretion no longer undergoes major compositional variations, levels of alpha tocopherol appear to remain constant over time. This was verified in Poland17 and Greece,21 where collections of mature milk were performed in different months during the postpartum period, yielding values of alpha-tocopherol that did not differ significantly (Table 1).
Age and maternal socioeconomic statusThe consumption of vitamins by adolescences is quite deficient, especially fat-soluble vitamins.14 Adolescents are particularly susceptible to nutritional risks due to inadequate dietary habits, as they prefer to consume high-energy content foods that are low in micronutrients.12 Moreover, the pregnant adolescent has to add her own growth requirements to other requirements imposed by pregnancy.22
Therefore, when pregnancy and subsequent lactation occur in adolescence, nutritional risks associated with this condition may increase. Hence the hypothesis that the milk of adolescent mothers may show lower amounts of alpha-tocopherol than the milk of adult mothers.12
In the study by Dimenstein et al.,22 there was no difference (p=0.50) between alpha-tocopherol levels in the colostrum of Brazilian adolescent and adult mothers (Table 1). The authors emphasize, however, that the mean age for the adolescent mothers was 17.2±1.4 years, which minimizes the impact of menarche on their nutritional status, as it is the proximity between menarche and pregnancy that potentiates such impact. However, other studies have not found this association.5,13,23
Only Azeredo and Trugo,12 analyzing the content of alpha-tocopherol in mature milk of adolescents from southeastern Brazil, concluded that the concentration of this vitamin in their breast milk is equivalent to less than half of that reported for the milk of adult women in developing countries. However, this study did not use a control group of adult women, but only compared their results to studies with mature milk of adult postpartum women.
Maternal socioeconomic status also does not appear to be related to the concentration of alpha-tocopherol in milk. The association between these variables was studied by some authors, who observed that income and maternal educational level were not associated with vitamin E content in breast milk.5,13
However, if studies were performed in different locations, comparing the extremes of socioeconomic status categorization, these differences would perhaps appear, as the mean concentration of alpha-tocopherol in the milk of populations of extreme social deprivation is lower when compared to that of populations with better socioeconomic status (Table 1).
Parity and gestational age of the newbornIn some mammals, the number of births is directly associated with increased levels of vitamin E in milk. One possible explanation for this fact is the increased mobilization of tissues containing alpha-tocopherol, such as the adipose tissue.4
Some authors suggest that parity may influence vitamin levels such as retinol in breast milk, when the previous lactation generated a high mobilization of the reserves and high transfer to the mammary gland. This mobilization is also influenced by maternal adiposity in multiparous women, and may contribute to higher vitamin content in the breast milk of these women.24 This hypothesis can be extended to alpha-tocopherol, as the latter, similarly to retinol, is a fat-soluble vitamin stored in adipose tissue.
The majority of studies on the association between parity and the concentration of alpha-tocopherol in breast milk found no association between these variables.5,23,25 However, Campos,14 in Brazil, found larger amounts in the transition milk of primiparous women. Regarding the mature milk, multiparous women had higher concentrations of the vitamin. However, further studies are needed to clarify this association, as this study was performed with a small sample size (nine primiparous and nine multiparous women).
Another variable whose association with the nutritional composition of human milk was studied was the newborn's gestational age. Premature neonates (less than 37 weeks of gestation) are at most risk of developing vitamin E deficiency, as they require a greater supply of antioxidant nutrients due to exposure to oxidative stress caused by infections, oxygen, mechanical ventilation, and intravenous nutrition. Premature infants with vitamin E deficiency have low hemoglobin levels, morphological alterations such as anisocytosis and fragmented red cells, reticulocyte response, increase in the number of platelets, and hyperbilirubinemia.26
The hypothesis of differences in vitamin E concentration depending on the duration of pregnancy has not been confirmed.10,23,27 Quiles et al.,8 however, in a study of Spanish women, observed that milk from mothers of full-term infants had significantly higher amounts of this vitamin at all stages of lactation (p<0.05).
These conflicting data demonstrate the need for further studies regarding the concentration of vitamin E in the milk of mothers of preterm infants, as the placental transfer of this vitamin during pregnancy is limited.28 This limitation makes the supply of alpha-tocopherol through breast milk even more essential, especially for preterm infants, whose gestational age, and therefore, transfer of nutrients to the fetus through the placenta, is even lower.
Biochemical nutritional status in alpha-tocopherol and maternal anthropometric nutritional statusMost studies that evaluated the association between the concentration of alpha-tocopherol in blood and maternal milk demonstrate that this correlation does not exist in colostrum and mature milk,12,15,23,29–32 indicating to a probable vitamin transfer limitation from plasma to the mammary gland.
In Brazil, Dimenstein et al.32 studied the association between alpha-tocopherol in colostrum and plasma under fasting and postprandial conditions and concluded that the correlation between alpha-tocopherol in colostrum after fasting and postprandial and the absence of correlation between plasma and colostrum excludes the existence of passive transfer mechanisms during the passage of vitamin E to milk. According to the authors, there are probably different mechanisms of vitamin transport to the mammary glands, which are independent from plasma concentrations.
Although the mechanisms involved in the uptake of alpha-tocopherol by the mammary gland are not completely understood, it is believed that part of alpha-tocopherol reaches the milk through LDL receptors and another part can be transported through cell surface receptors (SR-B1) that bind to HDL and LDL without lipoprotein internalization. There is also the suggestion that it occurs via lipoprotein lipase (LPL), as observed in experiments with rats.3,33 Additionally, a study in cows demonstrated that the secretion of alpha-tocopherol to the milk follows the Michaelis-Menten kinetics, i.e., its passage from blood to milk occurs through active transport through membranes, with no further increase in the secretion of this vitamin in milk when the maximum secretion capacity has been reached.34
Dimenstein et al.29 point out that the suggestion of distinct mechanisms of transport and the fact that there is no association between alpha-tocopherol in plasma and in colostrum under supplementation conditions, reinforce the hypothesis that the mammary gland can express alpha-TPP protein, the alpha-tocopherol carrier protein. Azeredo and Trugo12 also suggest that the transport of vitamin E to milk may involve membrane and intracellular receptors for alpha-TTP in mammary epithelial cells.
The study by Garcia et al.,15 however, found a positive correlation between the biochemical nutritional status in alpha-tocopherol and its concentration in transitional milk (r=0.456, p=0.009), demonstrating the importance of adequate maternal nutritional status. A study performed in Russia also demonstrated this correlation.10 However, this association has been studied only in the milk of mothers of preterm newborns, with a small sample size (13 women).
According to Garcia et al.,15 the presence of an association between the levels of alpha-tocopherol in plasma and in milk found only in the transition phase indicates that the vitamin transport mechanisms to the colostrum are more complex, probably involving other routes in addition to those that are predominant in transitional and mature milk. There is an open field for studies evaluating the association between the concentration of vitamin E in plasma and breast milk, especially in colostrum and mature milk.
Regarding the maternal anthropometric nutritional status during pregnancy, the most commonly used indicator to assess its association with alpha-tocopherol in milk is the body mass index (BMI). The hypothesis that maternal BMI may be related to the content of the vitamin in milk presupposes that this indicator is, in most cases, proportional to body fat content. Therefore, since adipose tissue is a storage site for alpha-tocopherol, the higher the BMI of the lactating woman, the greater the levels of vitamin stored in this tissue and consequently released into the milk.
However, no study has demonstrated an association between BMI and vitamin E in breast milk.5,12,13,23 Thus, the present results indicate that the levels of alpha-tocopherol in milk appear to be independent from the maternal body mass.
Maternal habitual dietary intake and vitamin E supplementationA variable widely studied by researchers that analyzed vitamin E in breast milk is maternal dietary intake of micronutrients, in order to understand whether the diet influences the nutritional composition of breast milk.
Antonakou et al.,21 in Greece, asked women in the postpartum period regarding the intake of foods rich in vitamin E through three dietary recalls. The results indicate that the intake of vitamin E appears to have no effect on its concentration in breast milk, which is corroborated by the fact that, although the mean intake of vitamin by the women was lower than the recommended, the micronutrient content in milk achieved the recommended levels for infants.
In Canada, Bishara et al.35 used a semiquantitative food frequency questionnaire to assess dietary intake of vitamin E by mothers of low-birth weight preterm infants. In that study, no association was found between alpha-tocopherol intake and its concentration in milk.
Szlagatys-Sidorkiewicz et al.,9 based on a three-day nutritional diary made by 49 Polish women, observed that the concentration of vitamin E in breast milk was not correlated with their respective dietary intake. In that study, the concentration of vitamin E in milk was not higher in women who received the vitamin supplements recommended for pregnant and lactating women, compared to those who did not (p=0.332). Also in Poland, Martysiak-Zurowska et al.17 obtained similar results, with no correlation between dietary vitamin E intake and the use of supplements with the concentration of alpha-tocopherol in breast milk.
Another study, which analyzed breast milk in Russian women who received vitamin supplements containing alpha-tocopherol during gestation and lactation, also found no difference in the concentration of vitamin E in the milk of these women, when compared to those who did not receive the multivitamins.10 However, a study in Canada observed a positive correlation between vitamin E found in milk and multivitamin supplementation, as reported by survey participants.36
Dimenstein et al.,29 when analyzing tocopherol in the milk of 30 adult women in Northeastern Brazil, observed that supplementation with a capsule containing synthetic vitamin E (49.4mg dl-alpha-tocopherol) did not lead to an increase in the concentration of the vitamin in colostrum 24hours after supplementation. According to the authors, this indicates that the passage of this vitamin is limited and raises the question of the validity of offering supplements containing vitamin E with racemic mixtures.
However, in their study in the same Brazilian population, Garcia et al.,30 using a supplemented and a non-supplemented group, observed that 24hours after supplementation with the abovementioned capsule, there was a significant increase in the amount of alpha-tocopherol in the colostrum of the supplemented group (p=0.04), which did not occur in controls. Thus, the fact that Dimenstein et al.29 did not find any influence of supplementation might have been caused by the absence of a control group in the study, as the content of alpha-tocopherol in colostrum tends to decrease over the first few days of lactation.
Therefore, the concentration of vitamin in the milk on the day after the supplementation should have been compared to the concentration in the same period in a non-supplemented control group, and not to the concentration in the same group on the day before supplementation, which is usually higher.
The capsule offered to women in the two abovementioned studies also contained an overdose of vitamin A. According to Green et al.,37 in situations of supplementation, the transfer of vitamin A to the mammary gland also occurs via chylomicrons and depends on the binding site of the latter and lipolysis of triacylglycerols via LPL action. Garcia et al.30 concluded, therefore, that this increase in circulating chylomicrons, with the increase in LPL activity in the mammary gland, also stimulated the uptake of alpha-tocopherol present in the capsule or dietary tocopherol, by increasing its bioavailability.
Clemente25 also found significantly higher amounts of alpha-tocopherol in colostrum of Brazilian postpartum women supplemented in the postpartum period with both natural and synthetic alpha-tocopherol, when compared to a control group that was not supplemented. It is noteworthy that 24hours after supplementation, women that received supplements with natural vitamin had 101% more vitamin in the colostrum than women in the control group, while the mothers in the group that received the synthetic supplementation had only 51.6% more, showing a greater effectiveness of natural supplementation compared to synthetic.
Based on the results of these studies, it can be concluded that maternal dietary intake of vitamin E through the usual diet does not affect the vitamin concentration in breast milk. However, in situations of supplementation, studies have shown increased levels of alpha-tocopherol in breast milk (especially when this is performed in the postpartum period), while others did not observe this association.
Thus, the actual effects of supplementation on tocopherol levels in breast milk are still unknown, and there is a great need for new studies to investigate this association. Furthermore, it is important to note which type of supplementation is offered, as its absorption may or may not be favored, depending on the chemical form used.
Final considerationsThe knowledge of factors that can influence vitamin E content in human milk can provide important information for the prevention of its deficiency in postpartum women and infants, as some of these variables can be controlled.
Based on this review, it was observed that the concentration of alpha-tocopherol tends to decrease as the milk becomes mature. Parity, anthropometric nutritional status, socioeconomic status, and habitual dietary intake of vitamin E by the mother do not appear to affect the levels of this nutrient in breast milk.
However, variables such as maternal age, alpha-tocopherol biochemical nutritional status, gestational age, and maternal vitamin E supplementation still demonstrate controversies regarding their association with vitamin E content of human milk and thus, further studies are necessary.
However, it is important to observe that in most studies that observed an association between these variables, this association did not occur in colostrum milk, but in transitional and mature milk. This indicates possible milk homeostasis during colostrum secretion, in which the concentration of alpha-tocopherol does not vary in most cases, regardless of influencing factors. This fact highlights the importance of feeding the newborn in the first days postpartum, which will provide an important antioxidant defense and ensure the proper development of the immune system, as colostrum has a high concentration of alpha-tocopherol. Furthermore, the reduction of this vitamin content in the transitional and mature milk indicates the need to review the recommendations of vitamin E intake for infants, as current recommendations are not met by the milks at these stages of lactation in some populations studied.
Conflicts of interestThe authors declare no conflicts of interest.
To Heleni Aires Clemente, for her contribution and suggestions that improved this study.
Please cite this article as: Lima MS, Dimenstein R, Ribeiro KD. Vitamin E concentration in human milk and associated factors: a literature review. J Pediatr (Rio J). 2014;90:440–8.
Study conducted at the Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil.