To analyze the interventions aimed at the practice of sleep hygiene, as well as their applicability and effectiveness in the clinical scenario, so that they may be used by pediatricians and family physicians for parental advice.
Source of dataA search of the PubMed database was performed using the following descriptors: sleep hygiene OR sleep education AND children or school-aged. In the LILACS and SciELO databases, the descriptors in Portuguese were: higiene E sono, educação E sono, educação E sono E crianças, e higiene E sono E infância, with no limitations of the publication period.
Summary of the findingsIn total, ten articles were reviewed, in which the main objectives were to analyze the effectiveness of behavioral approaches and sleep hygiene techniques on children's sleep quality and parents’ quality of life. The techniques used were one or more of the following: positive routines; controlled comforting and gradual extinction or sleep remodeling; as well as written diaries to monitor children's sleep patterns. All of the approaches yielded positive results.
ConclusionsAlthough behavioral approaches to pediatric sleep hygiene are easy to apply and adhere to, there have been very few studies evaluating the effectiveness of the available techniques. This review demonstrated that these methods are effective in providing sleep hygiene for children, thus reflecting on parents’ improved quality of life. It is of utmost importance that pediatricians and family physicians are aware of such methods in order to adequately advise patients and their families.
Avaliar as intervenções visando práticas de higiene do sono em crianças, sua aplicabilidade e efetividade na prática clínica, para que as mesmas possam ser utilizadas na orientação dos pais pelos pediatras e médicos de família.
Fonte dos dadosFoi realizada busca na base de dados da Pubmed utilizando os descritores sleep hygiene OR sleep education AND child or school-aged, e nas bases Lilacs e Scielo, com as seguintes palavras-chave: higiene E sono, educação E sono, educação E sono E crianças, e higiene E sono E infância, não tendo sido limitado o período de busca.
Síntese dos dadosForam revisados 10 artigos cujos objetivos eram analisar efetividade de abordagens comportamentais e de técnicas de higiene do sono sobre a qualidade do sono das crianças e na qualidade de vida dos pais. Foram utilizadas uma ou mais das seguintes técnicas: rotinas positivas, checagem mínima com extinção sistemática e extinção gradativa ou remodelamento do sono, bem como diários do padrão de sono. Todas as abordagens apresentaram resultados positivos.
ConclusõesApesar de a abordagem comportamental no manejo do sono na faixa etária pediátrica ser de simples execução e adesão, existem poucos estudos na literatura que avaliaram sua efetividade. Os estudos revisados evidenciaram que estas medidas são efetivas na higiene e refletem em melhoria na qualidade de vida dos pais. É de fundamental importância os pediatras e médicos de família conhecerem estas abordagens, para que possam oferecer orientações adequadas a seus pacientes.
The prevalence of sleep disorders is high in childhood and may affect up to 30% of school-age children.1,2 These disorders are important due to the effects they can have not only on the child, but also on their families and society.3 Thus, a child with chronic sleep disorders may have learning and memory consolidation impairment at school, irritability and mood modulation alterations, difficulty sustaining attention, and behavioral alterations such as aggression, hyperactivity, or impulsivity.4–7 Furthermore, the chronic sleep deficit lowers the threshold for accidental injury and promotes metabolic changes that, in the long term, can cause other conditions, such as overweight and its consequences.8,9
Pediatricians and family physicians play a key role in promoting quality of sleep in children.10,11 For this purpose, they need to have knowledge of methods of sleep quality promotion, of physiology aspects and age-dependent sleep modifications, and of the importance of good-quality sleep in childhood.12 A recent study demonstrated that, although 96% of American pediatricians consider it to be their role to advise parents about sleep hygiene methods, only 18% reported having received formal training on the subject.10
Moreover, in the United States, the Sleep in America Poll, conducted in 2004, including approximately 1,500 families of children up to 10 years old, demonstrated that only 13% of pediatricians asked parents about possible sleep disorders.13 A survey conducted in pediatrics residency programs in the United States, Canada, Japan, India, Vietnam, South Korea, Singapore, and Indonesia observed that the mean time spent in sleep education at the institutions in those countries was two hours during the training period, and that a quarter of the reported programs offered no instruction on the subject.14
Sleep disorders are divided into eight different categories, which include insomnia, sleep disordered breathing, hypersomnia of central origin, circadian rhythm disorders, parasomnias sleep-related movement disorders, unresolved issues and isolated symptoms (which include snoring, somniloquy, and benign myoclonus), and other sleep disorders.15 The latter category includes sleep disorders considered to be physiological or environmental.16 The environmental disorders, often of behavioral origin, can be prevented if properly managed through sleep hygiene measures.17
ObjectiveThe objective of this article was to perform a systematic review of interventions aiming at sleep hygiene, and their applicability and effectiveness in pediatric clinical practice, so that they can be used in parental guidance.
MethodsBetween the months of March and April of 2014, a search was conducted in the PubMed database using the following keywords sleep hygiene OR sleep education AND children or school-aged. Review articles were excluded, as well as those including participants aged 10 years or more, or populations with comorbidities (hospitalization during the study, neurological or respiratory diseases, behavioral or psychiatric disorders).
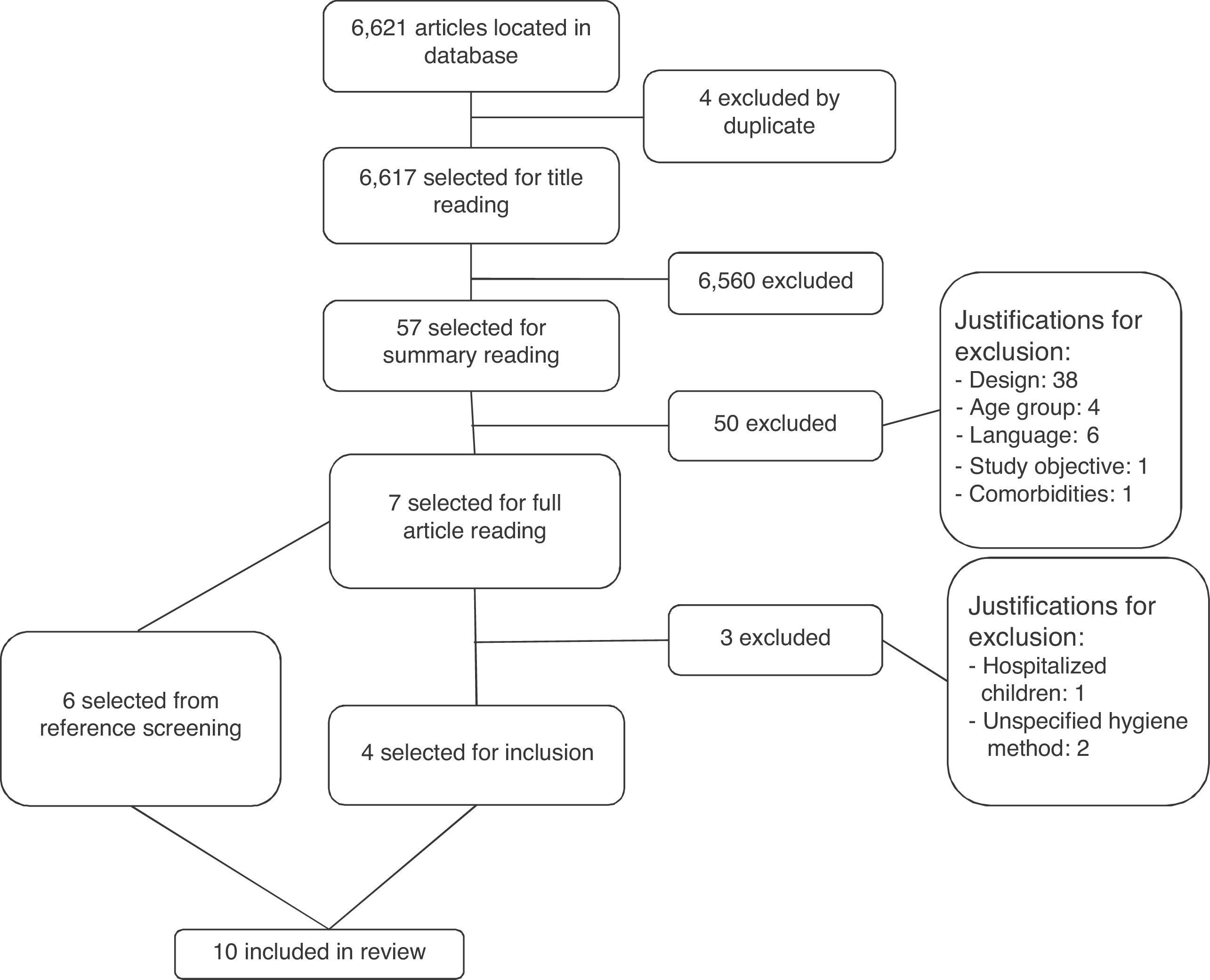
Studies of children with diagnosis of parasomnias were also excluded from this analysis, as well as those in which the sleep hygiene method was not properly specified in the methods section. Only studies published in Portuguese, English, and Spanish were reviewed. The search totaled 6,621 articles, of which four were excluded as duplicates. Of the remaining 6,617, after reading the titles, 57 were considered possibly relevant and had their abstracts reviewed. Of these, 50 were excluded for not meeting the inclusion criteria, and seven were selected to be read as full texts. Of these, four were considered relevant for this study.18–21
The same search, but with descriptors in Portuguese, was conducted in the LILACS and SciELO databases. The keywords used were higiene E sono, educação E sono, educação E sono E crianças, e higiene E sono E infância. In the LILACS database, two references were found, neither of which met the scope of this review. In the SciELO database, the descriptors higiene E sono resulted in 20 articles, none of which met the criteria for inclusion in this study. In this same database, the descriptors educação E sono E crianças resulted in five articles, none of which met the scope of this review.
The analysis of the studies and their references also offered the possibility of access to other publications, and thus a total of six new references were sought and included in this review.22–27Fig. 1 shows the process of search, selection, and exclusion of articles present in the current literature.
DefinitionsThe diagnosis of sleep disorders requires the presence of specific criteria, which must be present for a specific period of time and have negative consequences on the child and/or parents.1 Thus, mild or moderate symptoms are not considered disorders, although they can cause some degree of impairment.28
The mean latency to sleep onset is usually about 19 minutes in children up to 2 years of age, and 17minutes from the age of 3 until the beginning of adolescence.29 In children, insomnia, defined as difficulty initiating or maintaining sleep and comprising a number of sub-classifications, usually falls under the diagnosis of behavioral insomnia.30 That, in turn, is divided between 1) sleep-onset association type and 2) limit-setting type, or mixed form.
The most common subtype, “limit-setting type”, comprises the attempt to postpone going to sleep or refusing to do so, characterized by crying, refusing to stay in bed, or requests for food, drink, or the reading of stories. In this context, it is customary to identify parents with inconsistent routines that tend to give in to their children's requests.31 In the “sleep-onset association” subtype, certain behaviors need to be repeated at every waking episode for the child to resume sleep. Thus, a child that associates sleep onset with the presence of one or both parents, food, or being rocked to sleep, when awakening during the night - even with normal awakenings expected for their age group - needs to have the ritual repeated to resume sleep.32
Parents¿ perception of their child having poor quality sleep is directly related to the number of night wakings and to how demanding the child is to initiate sleep at bedtime and retake sleep after night wakings.29,33 A recent analysis of data from Brazilian birth cohort found, at 12 months, a prevalence of nocturnal awakenings of 64.4% in the two weeks preceding the study, with 56.5% of the children waking up every night, and most of them at least two times each night.34
The term “sleep hygiene” includes changes in sleep environment, as well as engaging the child and their parents on routine and practices that encourage sleep of good quality and sufficient duration. It also includes the practice of soothing activities during wakefulness aiming to propitiate sleep onset.11 The most usual practices are having consistent bedtime and wake-up time for both the nocturnal and daytime sleep (among children at the age group where naps are considered physiological), establishing the appropriate place to initiate sleep, and avoiding environmental and behavioral associations with sleep onset (being rocked to sleep, parents laying on the child's bed until sleep onset, nursing to sleep, watching TV in bed, or drinking beverages rich in caffeine close to bedtime).17
Children who need behavioral associations to fall asleep, upon awakening during the night, will need these resources again in order to resume sleep.1 The passive presence of a parent, however, appears to be positive at some age groups, as well as the use of the child's own resources, such as using a pacifier or thumb-sucking and sleeping with a transitional object.35
Methods of sleep hygiene promotionThe most studied methods are discussed below. These strategies appear to work better in children aged 2 years and older, when a reward system can be used.2 However, some studies have attempted to advise pregnant women or parents of infants in order to promote problem prevention.1,33
Extinction: Parents should put the child in bed at a pre-specified time and ignore the child until a certain time on the following morning, while monitoring for the possibility of injury. The method is based on eliminating the acts that reinforce certain behaviors (such as crying on awakening), aiming at their extinction over time.36 The greatest difficulty in implementing this strategy is the parents’ lack of consistency and the parental anxiety that is generated. As a result, some defend the strategy of extinction in the presence of parents, such that parents remain in the room but do not respond to the child's behavior.2,36
Gradual extinction: In spite of comprising different techniques, the gradual extinction method usually consists of ignoring the demands of the child for specific time periods; these periods are usually determined by the child's age and temperament and the parents’ discretion in relation to how long they tolerate their child's crying. Parents should calm the child for short periods, which usually range from 15seconds to one minute. The technique aims to promote the child's capacity to self-soothe and return to sleep, without undesirable associations or parental interference.1,2,36
When assessing 79 children with a mean age of 10.2 months (3-24 months) whose parents were instructed to implement the gradual extinction technique during nocturnal sleep, Skuladottir et al. observed that the duration of nocturnal sleep increased from 10.27hours to 10.57hours (p<0.001) after the intervention, as well as reducing the frequency of nocturnal awakenings (from 4.57 to 1.57 per night, p<0.001).18
Eckerberg conducted a study to assess whether recommendations provided only in written form to the parents of children treated at a clinic for sleep disorders would work as well as clinical follow-up, which had been previously advocated.19 Guidance to parents of children included in the study followed the gradual extinction method, the same provided by the physician during routine consultations. A total of 39 children between 4 and 30 months of age participated in the study, divided into an intervention group (written information sent by email, without contact with the clinician) and a control group (information given by the clinician). After the intervention, children from both groups fell asleep faster (p<0.001) and earlier (p<0.01), which amounted to 30minutes earlier after a one-month intervention.
In both groups, there was also a significant reduction in nocturnal awakenings (from 4.6 to 4.2 awakenings in the control and from 3.3 to 2.8 in the intervention group, p<0.001) in the two weeks following the intervention. The probability of resume sleep on their own also increased after the intervention (2.1-fold in the control and 2.0-fold in the intervention group, p<0.001). After three months, this decrease continued in both groups, and there was an increase in the duration of nocturnal sleep (by 59minutes in the control and by 72minutes in the intervention group) and a decrease in time of wakefulness during the night (from 82 to 18minutes, p<0.001), with no differences between the groups.
In an Australian case-control study carried out by Hiscock & Wake, 146 children between 7 and 9 months of age were recruited from an outpatient setting.22 The intervention group received specialized guidance on the physiology of sleep and the application of the gradual extinction method, whereas the control group received a newsletter about normal sleep patterns at the age range of 6-12 months. Two months later, children in the intervention group had resolved more sleep problems than those in the control group (p=0.005), and the remaining problems were less intense in the intervention group. Maternal depressive symptoms decreased in both groups after two months, but decreased more significantly in the intervention group (p=0.02), the group whose mothers also reported that their own sleep was of better quality (p=0.02) at the end of the follow-up.
Aiming to compare the effectiveness of the gradual extinction and extinction methods, and of these in relation to no sleep hygiene method, Reid MJ et al. analyzed 43 children aged 16 to 48 months (14 extinction, 13 gradual extinction, and 16 controls) prior to intervention, and at 21 days and two months after intervention.23 They observed that families allocated to the extinction group had more difficulty adhering to the method during the second week in relation to the gradual extinction group (interrupting the intervention on average 3.4 times each week, compared to 1.1 times in the other group, p=0.02). During the remaining time, adherence remained high and similar in both groups (p<0.01).
The intervention groups also had better assessments regarding quality at both the moment of sleep onset and sleep maintenance, when compared to the control group. In the subscale regarding quality of sleep in the CBCL (Child Behavior Checklist), both intervention groups also scored better in relation to the control group, and similarly to each other. Two months later, a new evaluation showed that the benefits remained in the groups that underwent interventions.
Minimal checking with systematic extinction: Similar to the extinction method, but the child can be checked every 5 to 10minutes, and the parent can comfort the child quickly when necessary, arranging the covers, and making sure that there are no complications.2
Adachi et al. analyzed 99 children taken for childcare consultation at 4 months of age, randomly dividing them between intervention and control groups.20 The intervention consisted of information about positive routines for initiating sleep, appropriate and inappropriate behaviors to resume sleep at night, and the method of minimal checking with systematic extinction. At the end of the study, the intervention group had a greater decrease in the rates of behaviors listed as “inadequate”. The characteristic of “giving food or a diaper change immediately” decreased from 66.7% to 36.4% (p=0.001), and the characteristic described as “holding and comforting immediately” decreased from 22.7% to 10.6% (p=0.021). In the control group, the number of nocturnal awakenings increased significantly from 53% to 66.7% (p=0.022), as did the number of awakenings with crying (from 8.1% to 19.4%, p=0.065).
An intervention conducted by Hall et al. included 39 families of infants aged 6 to 12 months, whose parents sought help through a telephone answering service for parents of infants with difficulty sleeping.21 The aim of the study was to analyze the improvement in the parents’ quality of life, and at the end of the intervention, a significant improvement in the parents’ quality of sleep was observed, as well as of symptoms of depressed mood and fatigue. The co-sleeping rates also decreased significantly (from 70% practicing them before the intervention to 74% not practicing them after the intervention, p<0.001), with no change in the practice of breastfeeding.
Positive routines: This method consists of the development of routines preceding bedtime, comprising peaceful and pleasurable activities.37 Another strategy that can be used is delaying the time to go to bed to ensure that, when lying down, the child will fall asleep quickly, until this habit of falling asleep quickly is consolidated. After that, start anticipating bedtime by 15 to 30minutes on successive nights until the time considered appropriate is achieved. The child should not sleep during the day, except at the age groups in which daytime sleep is physiological.2,36
Positive routines are often used in combination with other methods of sleep hygiene. Adachi et al. included behavioral recommendations in their intervention group. At the end of the intervention, they found that the practice of positive routines characterized by “playing and stimulating during the day” (p=0.003), “establishing a place to sleep” (p=0.008), and “establishing a timetable to sleep and wake up” (p=0.007) had increased significantly.20
Mindell et al. performed a study including children in two groups (7-18 months and 18-36 months), in which a routine preceding sleep was implemented, consisting of a bath followed by massage and quiet activities, with a time period between the bath and turning off the lights of 30minutes.24 The routine significantly reduced problem behaviors in both groups, with decreased sleep latency and the number and duration of nocturnal awakenings (p<0.001). The mothers in the group of children aged up to 18 months showed reduction in symptoms of stress, depression, anger, fatigue, lack of stamina, and confusion (p<0.001) and, in the group older than 18 months, there was an improvement in the symptoms of stress, anger, fatigue, and confusion (p<0.001).
This study had a long-term follow up, in which 65% of participants in the group aged up to 18 months were randomized into three groups: one received instructions exclusively via the internet, another received instructions via the internet in addition to those described in the previous study, and a third group was used as control.25 After one year, the improvements observed in the two groups that received the interventions regarding sleep latency, difficulty falling asleep, number and duration of nocturnal awakenings, period of continuous sleep, and maternal confidence in relation to her child's sleep management persisted (p<0.001). After three weeks of intervention, the quality of maternal sleep improved significantly (p<0.001); after one year, however, it decreased back to levels close to those at the start of the intervention.
Aiming to compare the effectiveness between positive routines and gradual extinction in reducing temper tantrums with bouts of anger at bedtime, Adams and Rickert followed, for six weeks, two groups of children targeted for each intervention compared to a control group, in a total of 36 children (12 per group) aged between 18 and 48 months.26 The children in the groups submitted to any of the interventions had significantly fewer bouts of anger, which were of shorter duration than the controls (p<0.05 and p<0.001, respectively). There was no significant difference in response between the intervention groups, although children in the group submitted to positive routines showed faster favorable responses. Parents in the group allocated to implement positive routines also scored better on the Marital Adjustment Scale at the end of the intervention, which was validated for that population, and investigates the perception that the couple has of their relationship.38
Programmed awakening: It consists in waking up the child at night, between 15 and 30minutes before the usual time of spontaneous awakening, and after that, comforting her to return to sleep. The number of programmed awakenings should vary with the usual number of spontaneous awakenings. Over time, it tends to extinguish spontaneous awakenings, and the process of reducing scheduled awakenings begins, resulting in increased sleep consolidation.1,2,36
Rickert & Johnson compared the methods of programmed awakening and systematic extinction with a control group in 33 children with a mean age of 20 months (6-54 months), randomly allocating them into three groups of 11 children (programmed awakening, systematic extinction, and a control group).27 The intervention lasted eight weeks, and parents were re-contacted three and six weeks later. Children who experienced the interventions showed, at the end of the experiment, fewer nocturnal awakenings (p<0.05), although this decrease occurred faster in the group submitted to the extinction method. This difference remained statistically significant during the reassessments.
Sleep remodeling: Consists of not allowing naps to occur at times that can disrupt nocturnal sleep onset, which comprises four hours before bedtime in children at an age range that allows two naps per day, and six hours before bedtime in children who usually have one nap a day.18
The study developed by Skuladottir et al. used this technique for daytime naps.18 As demonstrated above, they observed positive results regarding the duration of nocturnal sleep.
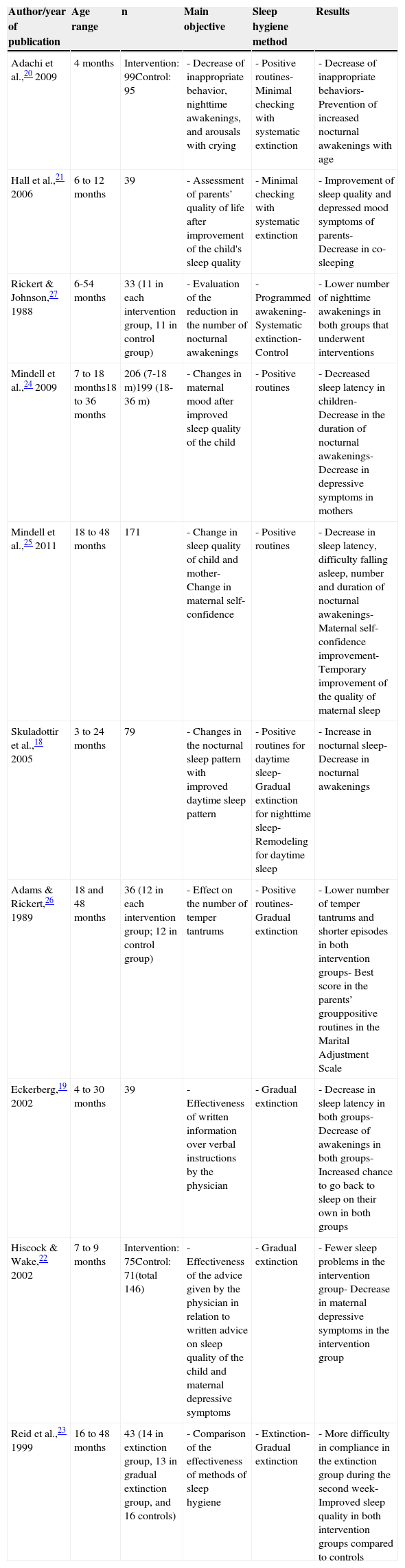
Table 1 summarizes the studies included in the present review by author, age group and sample size, objectives, type of intervention, and main results.
Studies reviewed, authors, age range of study, number of participants, objectives, type of intervention, and outcomes.
| Author/year of publication | Age range | n | Main objective | Sleep hygiene method | Results |
|---|---|---|---|---|---|
| Adachi et al.,20 2009 | 4 months | Intervention: 99Control: 95 | - Decrease of inappropriate behavior, nighttime awakenings, and arousals with crying | - Positive routines- Minimal checking with systematic extinction | - Decrease of inappropriate behaviors- Prevention of increased nocturnal awakenings with age |
| Hall et al.,21 2006 | 6 to 12 months | 39 | - Assessment of parents’ quality of life after improvement of the child's sleep quality | - Minimal checking with systematic extinction | - Improvement of sleep quality and depressed mood symptoms of parents- Decrease in co-sleeping |
| Rickert & Johnson,27 1988 | 6-54 months | 33 (11 in each intervention group, 11 in control group) | - Evaluation of the reduction in the number of nocturnal awakenings | - Programmed awakening- Systematic extinction- Control | - Lower number of nighttime awakenings in both groups that underwent interventions |
| Mindell et al.,24 2009 | 7 to 18 months18 to 36 months | 206 (7-18 m)199 (18-36 m) | - Changes in maternal mood after improved sleep quality of the child | - Positive routines | - Decreased sleep latency in children- Decrease in the duration of nocturnal awakenings- Decrease in depressive symptoms in mothers |
| Mindell et al.,25 2011 | 18 to 48 months | 171 | - Change in sleep quality of child and mother- Change in maternal self-confidence | - Positive routines | - Decrease in sleep latency, difficulty falling asleep, number and duration of nocturnal awakenings- Maternal self-confidence improvement- Temporary improvement of the quality of maternal sleep |
| Skuladottir et al.,18 2005 | 3 to 24 months | 79 | - Changes in the nocturnal sleep pattern with improved daytime sleep pattern | - Positive routines for daytime sleep- Gradual extinction for nighttime sleep- Remodeling for daytime sleep | - Increase in nocturnal sleep- Decrease in nocturnal awakenings |
| Adams & Rickert,26 1989 | 18 and 48 months | 36 (12 in each intervention group; 12 in control group) | - Effect on the number of temper tantrums | - Positive routines- Gradual extinction | - Lower number of temper tantrums and shorter episodes in both intervention groups- Best score in the parents’ grouppositive routines in the Marital Adjustment Scale |
| Eckerberg,19 2002 | 4 to 30 months | 39 | - Effectiveness of written information over verbal instructions by the physician | - Gradual extinction | - Decrease in sleep latency in both groups- Decrease of awakenings in both groups- Increased chance to go back to sleep on their own in both groups |
| Hiscock & Wake,22 2002 | 7 to 9 months | Intervention: 75Control: 71(total 146) | - Effectiveness of the advice given by the physician in relation to written advice on sleep quality of the child and maternal depressive symptoms | - Gradual extinction | - Fewer sleep problems in the intervention group- Decrease in maternal depressive symptoms in the intervention group |
| Reid et al.,23 1999 | 16 to 48 months | 43 (14 in extinction group, 13 in gradual extinction group, and 16 controls) | - Comparison of the effectiveness of methods of sleep hygiene | - Extinction- Gradual extinction | - More difficulty in compliance in the extinction group during the second week- Improved sleep quality in both intervention groups compared to controls |
The number of studies available in the literature on interventions targeting sleep hygiene in children without comorbid conditions is scarce.18–27 It is noteworthy that no Brazilian studies were found in this search. A recent cross-sectional study performed in the United States, with children aged 5 to 6 years from a low-income community consisting predominantly of Latino families, observed a four-fold higher prevalence of sleep alterations than normally expected at this age, suggesting that unfavorable socioeconomic conditions may contribute to poor sleep quality.39
This finding indicates the potential importance of this type of study and subsequent interventions in the Brazilian population, considering that the sleep quality improvement among children of different age ranges and socioeconomic levels could also contribute to the improvement of other indices of quality of life.
Some studies observed that groups of children receiving no intervention also obtained improvements in sleep quality indices at the reassessments. One possible explanation is the existence of an association between neural maturation and physiological circadian mechanisms, which in themselves act as a sleep regulator, improving sleep quality over time.1 However, it is noteworthy that children who received interventions consistently showed more significant improvements regarding indices of sleep quality. This fact suggests the importance of the external environment on the sleep maturation process.
Information provided only in writing (brochures, newsletters) can be equally effective.19 This is possibly due to the fact these can be consulted as often as parents deem necessary, and as doubts arise in the implementation of the techniques.
The interventions performed in the reviewed studies are simple and effective, and represent secondary educational measures for parents that do not imply additional cost to them or to the health system, because they basically consist of recommendations. It is possible that these interventions would actually imply cost savings to the system, as well to advised parents, whose children sleep better, and thus would probably have a lower chance of seeking specialized care, in addition to having better performance in their professional activities. The favorable results of all the interventions that objectively sought to analyze mood and quality of life of parents corroborate this hypothesis.
The reviewed studies addressed a broad age range, varying from 3 months to 4 years, mostly comprising children in their first year of life. The importance of this information lies in the fact that interventions in children younger than 2 years also appear to be effective, allowing early changes and preventing children's exposure to long periods of poor sleep.
The role of the health professional who works with children is to know the physiology of sleep and its physiological maturation process. The inclusion of questions about sleep quality and possible sleep impairment factors in the anamnesis, in addition to offering sleep hygiene guidelines regarding the prevention or treatment of pathological behaviors, should be part of every pediatric visit.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Halal CS, Nunes ML. Education in children's sleep hygiene: which approaches are effective? A systematic review. J Pediatr (Rio J). 2014;90:449–56.
Study conducted at Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brazil.