This study aims to assess the relationship of late-night cell phone use with sleep duration and quality in a sample of Iranian adolescents.
MethodsThe study population consisted of 2400 adolescents, aged 12–18 years, living in Isfahan, Iran. Age, body mass index, sleep duration, cell phone use after 9p.m., and physical activity were documented. For sleep assessment, the Pittsburgh Sleep Quality Index questionnaire was used.
ResultsThe participation rate was 90.4% (n=2257 adolescents). The mean (SD) age of participants was 15.44 (1.55) years; 1270 participants reported to use cell phone after 9p.m. Overall, 56.1% of girls and 38.9% of boys reported poor quality sleep, respectively. Wake-up time was 8:17 a.m. (2.33), among late-night cell phone users and 8:03a.m. (2.11) among non-users. Most (52%) late-night cell phone users had poor sleep quality. Sedentary participants had higher sleep latency than their peers. Adjusted binary and multinomial logistic regression models showed that late-night cell users were 1.39 times more likely to have a poor sleep quality than non-users (p-value<0.001).
ConclusionLate-night cell phone use by adolescents was associated with poorer sleep quality. Participants who were physically active had better sleep quality and quantity. As part of healthy lifestyle recommendations, avoidance of late-night cell phone use should be encouraged in adolescents.
Este estudo visa avaliar a relação entre o uso de celular à noite e a duração e a qualidade do sono em uma amostra de adolescentes iranianos.
MétodosA população estudada consistiu em 2400 adolescentes, com idades entre 12 e 18 anos, residindo em Isfahan, Irã. Foram documentados a idade, índice de massa corporal, duração do sono, uso de celular após as 21h00 e prática de atividade física. Para avaliação do sono, utilizamos o questionário de Índice de Qualidade do Sono de Pittsburgh (PSQI).
ResultadosA taxa de participação foi de 90,4% (n=2257 adolescentes). A idade média (DP) dos participantes foi de 15,44±(1,55) anos; 1270 participantes relataram o uso do celular após as 21h00. Em geral, 56,1% das meninas e 38,9% dos meninos relataram sono de má qualidade, respectivamente. Os indivíduos que utilizaram celular à noite acordaram às 8h17min (2,33) e os que não utilizaram acordaram às 8h03min (2,11). A maior parte (52%) dos usuários de celular à noite apresentou má qualidade de sono. Aqueles sem nenhum tipo de atividade física apresentaram maior latência do sono que seus outros pares. Os modelos ajustados de regressão logística binária e multinomial mostraram que os usuários de celular à noite foram 1,39 vezes mais propensos a ter má qualidade do sono que seus outros pares (valor de p<0,001).
ConclusãoO uso de celular à noite por adolescentes foi associado a pior qualidade do sono. Os participantes fisicamente ativos apresentaram melhor qualidade e maior tempo de sono. Como parte das recomendações de estilo de vida saudável, os adolescentes devem ser incentivados a evitar o uso de celular à noite.
It is well-documented that sleeping is a main component for solid cognitive and physical functions.1,2 Sleep has a crucial role in different aspects of life3; proper sleep is especially important for children and adolescents.4 It is suggested that sleep disturbances might increase the risk of physical and mental problems, especially during adolescence.5 Sleep deprivation among adolescents is not a new phenomenon; however, in recent years, its adverse health effects have drawn more clinical and academic attention.6
The technological revolution has made cell phones very attractive and popular.7,8 They have become a part of daily life,9 being increasingly used among children and adolescents,10 and have become one of the most common means of communication.5 Some children and adolescents are so dependent on their cell phones that they take them to bed, to ensure that they do not miss any incoming message.11
Due to the widespread use of cell phones, it is important to study possible adverse health effects of the exposure.12 Cell phone use has been reported to be associated with health problems.5 A number of studies have indicated that the use of cell phones as a part of electronic media is associated with sleep disorders. One study showed a significant correlation between cell phone use after lights out and sleep disturbances such as short sleep duration, low sleep quality, and excessive daytime sleepiness, as well as symptoms of insomnia among Japanese adolescents.5 King et al. demonstrated a decrease in objective sleep efficiency, total sleep time, and rapid eye movement sleep, along with an increased subjective sleep onset latency (SOL) in adolescents.13 According to Troxel et al., nighttime texting was associated with insufficient sleep.14
The various findings of studies in different populations may be due to cultural differences. The use of mobile devices is widespread in different countries, but most previous studies have been conducted in Western countries. To the best of the authors’ knowledge, no previous study has been conducted in this field in Middle Eastern children and adolescents. The experience in this regard in the pediatric population is limited. Studying different populations would help comparing the findings in different communities. This study aimed to assess, for the first time, the relationship of late-night cell phone use with sleep quality and duration in a sample of Iranian adolescents.
MethodsThis cross-sectional study was conducted in 2015 in Isfahan, the second largest city in Iran. This study was approved by the Research and Ethical Committee of the Isfahan University of Medical Sciences. An informed written consent was obtained from parents and oral assent from participants. To include participants with various socio-demographic levels, 2400 adolescents from 46 schools (23 all-female and 23 all-male) located in different parts of the city were selected. The questionnaires, along with the parents’ consent forms, were distributed among participants; the authors asked the students to complete it anonymously at home. Inclusion criteria consisted of students aged between 12 and 18 years who agreed to participate in the study. Individuals with neurological or psychological conditions that would have impaired the academic performance were not included in this study. Data were analyzed using IBM SPSS (IBM Corp. 2011. IBM SPSS Statistics for Windows, version 20.0. NY, EUA). Cramer's V and Gamma tests were run to determine the association between categorical variables. In order to compare the quantitative data, the t-test was applied, as well as the Mann–Whitney test for data that did not follow normal distribution. Kruskal–Wallis tests were performed to determine the mean differences between more than two groups with non-normal distribution. Proper binary and multinomial regression analyses were performed in order to omit the impact of confounding data. p-values<0.05 were considered to be significant.
Background and clinical variablesClinical variables consisted of age, sex, cell phone use after 9p.m., sleep duration, total sleep hour, sleep latency, length of actual sleep, bedtime, wake-up time, health status, and physical activity.
The Pittsburgh Sleep Quality Index (PSQI) questionnaire, which consists of 19 self-rated questions and five questions rated by the bed-partner or roommate, was used. The latter five questions are used for clinical information only – they are not tabulated in the scoring of the PSQI, and were not reported on in this study. The 19 self-rated questions assess a wide variety of factors relating to sleep quality, including estimates of sleep duration and latency, as well as frequency and severity of specific sleep-related issues. These 19 items are grouped into seven component scores, each weighted equally on a scale ranging from 0 to 3. The seven component scores are then added to yield a global PSQI score, which has ranges from 0 to 21; higher scores indicate worse sleep quality. A global sum of 5 or greater indicates poor sleep quality, while less than 5 indicates good sleep quality. In this study, in addition to the PSQI, another validated questionnaire was used to determine more information containing demographic variables such as age, sex, weight, height, parent's job, underlying illness, physical activity, and history of drug use, as well as health status and some behavior factors of the population. The Cronbach's alpha of the PSQI was 0.83.
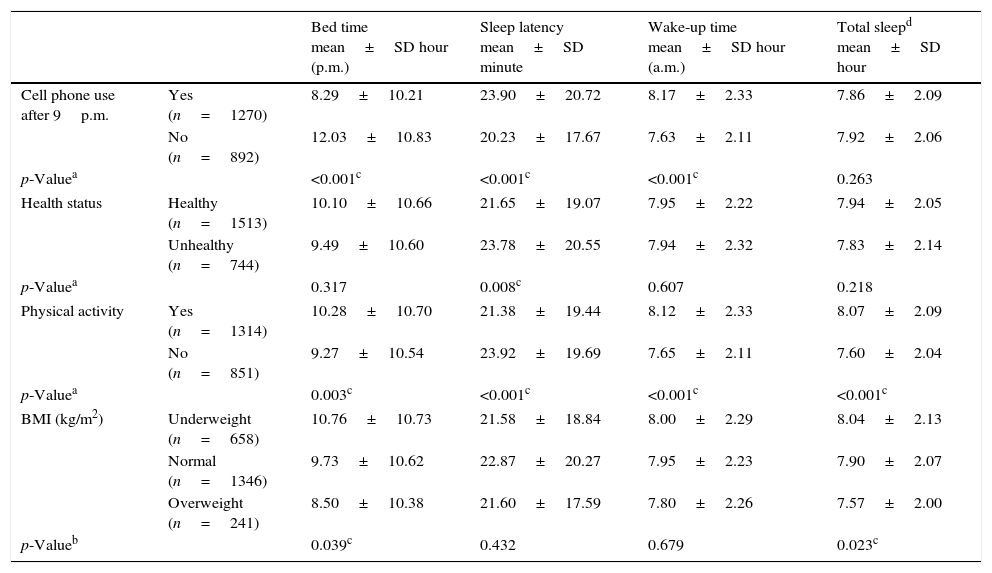
ResultsThe participation rate was 90.4%, and 2257 adolescents completed the PSQI (1169 males and 1086 females). The mean age (±SD) was 15.44±1.55 years. Overall, 1270 of participants had a positive history of using cell phone after 9p.m. and 892 of them did not have such history. Sleep latency was 24min (SD=21min) and 20min (SD=18min) in cell phone users and non-users, respectively. This finding suggests that cell phone users had significantly higher sleep latency than non-users (p-value<0.001). Those who used cell phone after 9p.m. had a mean wake-up time of 8:17a.m. whereas non-users had a mean wake-time of 8:03a.m. (p-value<0.001). No significant relationship regarding the difference of total sleep time in cell phone users and non-users was observed (p-value=0.263).
Physical activity was also an important clinical variable for the participants; 1314 of them reported to be physically active, whereas 851 participants did not. Sedentary participants had significantly longer sleep latency than those physically active (p-value<0.001). Total sleep time was also significantly higher in the physically active group (p-value<0.001). The mean wake-up time of sedentary participants 8:05a.m. (SD=131min), which was significantly earlier than the others, whose mean wake-up time was 8:12a.m. (SD=153min; p-value<0.001).
Another clinical variable that was measured among participants was the body mass index (BMI). The mean BMI was 20.36±3.32kg/m2 for girls, and 20.85±3.78kg/m2 for boys, and 20.59±3.55kg/m2 for the entire studied population. In total, 658 participants were underweight and had a total sleep time of 7.34h (SD=2.37h), 1346 were eutrophic and had a total sleep time of 7.26h (SD=2.35h), and 241 were overweight and had a total sleep time of 7.08h (SD=2.23h). As presented in Table 1, participants with higher BMI had lower total sleep time (p-value=0.023).
Characteristics of study participants.
| Bed time mean±SD hour (p.m.) | Sleep latency mean±SD minute | Wake-up time mean±SD hour (a.m.) | Total sleepd mean±SD hour | ||
|---|---|---|---|---|---|
| Cell phone use after 9p.m. | Yes (n=1270) | 8.29±10.21 | 23.90±20.72 | 8.17±2.33 | 7.86±2.09 |
| No (n=892) | 12.03±10.83 | 20.23±17.67 | 7.63±2.11 | 7.92±2.06 | |
| p-Valuea | <0.001c | <0.001c | <0.001c | 0.263 | |
| Health status | Healthy (n=1513) | 10.10±10.66 | 21.65±19.07 | 7.95±2.22 | 7.94±2.05 |
| Unhealthy (n=744) | 9.49±10.60 | 23.78±20.55 | 7.94±2.32 | 7.83±2.14 | |
| p-Valuea | 0.317 | 0.008c | 0.607 | 0.218 | |
| Physical activity | Yes (n=1314) | 10.28±10.70 | 21.38±19.44 | 8.12±2.33 | 8.07±2.09 |
| No (n=851) | 9.27±10.54 | 23.92±19.69 | 7.65±2.11 | 7.60±2.04 | |
| p-Valuea | 0.003c | <0.001c | <0.001c | <0.001c | |
| BMI (kg/m2) | Underweight (n=658) | 10.76±10.73 | 21.58±18.84 | 8.00±2.29 | 8.04±2.13 |
| Normal (n=1346) | 9.73±10.62 | 22.87±20.27 | 7.95±2.23 | 7.90±2.07 | |
| Overweight (n=241) | 8.50±10.38 | 21.60±17.59 | 7.80±2.26 | 7.57±2.00 | |
| p-Valueb | 0.039c | 0.432 | 0.679 | 0.023c | |
BMI, body mass index.
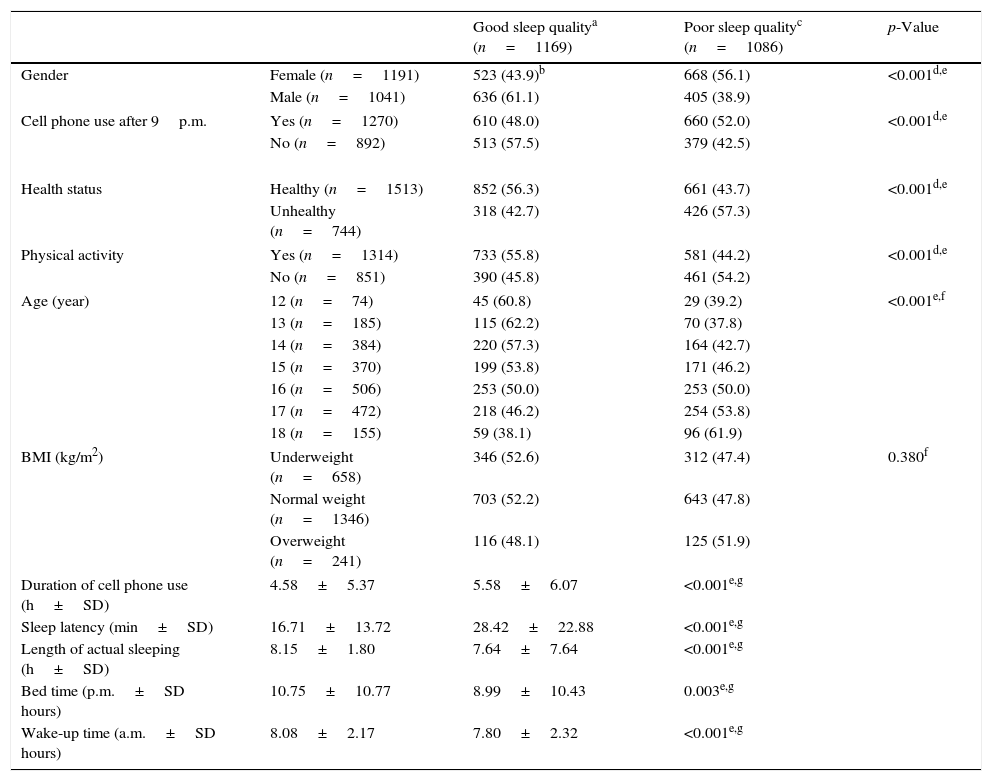
Table 2 presents the association of sleep quality (based on PSQI scores) with the clinical variables studied. Overall, 1270 participants had a positive history of using cell phones after 9p.m., 610 (48%) one of them had good-quality sleep, whereas 660 (52%) of them had poor quality of sleep. Conversely, 892 participants did not use cell phones after 9p.m. In this group, 513 (57.5%) of participants had good sleep quality, whereas 379 (42.5%) had poor sleep quality. Late-night cell phone use had a significant and negative impact on the sleep quality of participants (p-value<0.001). The duration of cell phone use among participants was also assessed: those with good quality of sleep used cell phones for 4h and 58min (SD=5h); for those with poor quality of sleep, this duration was 5h and 58min (SD=6h). It was observed that more time of cell phone use was associated with poorer sleep quality (p-value<0.001).
Association of sleep quality (based on PSQI scores) and demographic variables.
| Good sleep qualitya (n=1169) | Poor sleep qualityc (n=1086) | p-Value | ||
|---|---|---|---|---|
| Gender | Female (n=1191) | 523 (43.9)b | 668 (56.1) | <0.001d,e |
| Male (n=1041) | 636 (61.1) | 405 (38.9) | ||
| Cell phone use after 9p.m. | Yes (n=1270) | 610 (48.0) | 660 (52.0) | <0.001d,e |
| No (n=892) | 513 (57.5) | 379 (42.5) | ||
| Health status | Healthy (n=1513) | 852 (56.3) | 661 (43.7) | <0.001d,e |
| Unhealthy (n=744) | 318 (42.7) | 426 (57.3) | ||
| Physical activity | Yes (n=1314) | 733 (55.8) | 581 (44.2) | <0.001d,e |
| No (n=851) | 390 (45.8) | 461 (54.2) | ||
| Age (year) | 12 (n=74) | 45 (60.8) | 29 (39.2) | <0.001e,f |
| 13 (n=185) | 115 (62.2) | 70 (37.8) | ||
| 14 (n=384) | 220 (57.3) | 164 (42.7) | ||
| 15 (n=370) | 199 (53.8) | 171 (46.2) | ||
| 16 (n=506) | 253 (50.0) | 253 (50.0) | ||
| 17 (n=472) | 218 (46.2) | 254 (53.8) | ||
| 18 (n=155) | 59 (38.1) | 96 (61.9) | ||
| BMI (kg/m2) | Underweight (n=658) | 346 (52.6) | 312 (47.4) | 0.380f |
| Normal weight (n=1346) | 703 (52.2) | 643 (47.8) | ||
| Overweight (n=241) | 116 (48.1) | 125 (51.9) | ||
| Duration of cell phone use (h±SD) | 4.58±5.37 | 5.58±6.07 | <0.001e,g | |
| Sleep latency (min±SD) | 16.71±13.72 | 28.42±22.88 | <0.001e,g | |
| Length of actual sleeping (h±SD) | 8.15±1.80 | 7.64±7.64 | <0.001e,g | |
| Bed time (p.m.±SD hours) | 10.75±10.77 | 8.99±10.43 | 0.003e,g | |
| Wake-up time (a.m.±SD hours) | 8.08±2.17 | 7.80±2.32 | <0.001e,g | |
PSQI, Pittsburgh Sleep Quality Index; BMI, body mass index.
Overall, 1191 of participants were girls and 1041 of them were boys. It was that 43.9% of girls had good quality of sleep and 56.1% of them had poor quality sleep. Conversely, 61.1% of boys had good sleep quality and 38.9% of them had poor sleep quality. Boys had significantly better sleep quality than girls (p-value<0.001). Another clinical variable was BMI. Overall, 658 participants were underweight, 1346 were normal-weight, and 241 participants were overweight. Nevertheless, no significant differences were observed between sleep quality among groups with different BMI categories (p-value=0.38).
Another clinical variable studied was physical activity; of all participants, 1314 were physically active and 851 were inactive. It was observed that 55.8% of those who were active had good sleep quality and 44.2% had poor sleep quality. On the other hand, 45.8% of physically inactive participants had good sleep quality, whereas 54.2% of them had poor sleep quality. Physical activity had a significant and positive relationship with sleep quality (p-value<0.001). Age was also one of the clinical variables. Those with the best quality of sleep were the youngest (12-year-olds), whereas the oldest (18-year-olds) had worst quality of sleep (p-value<0.001).
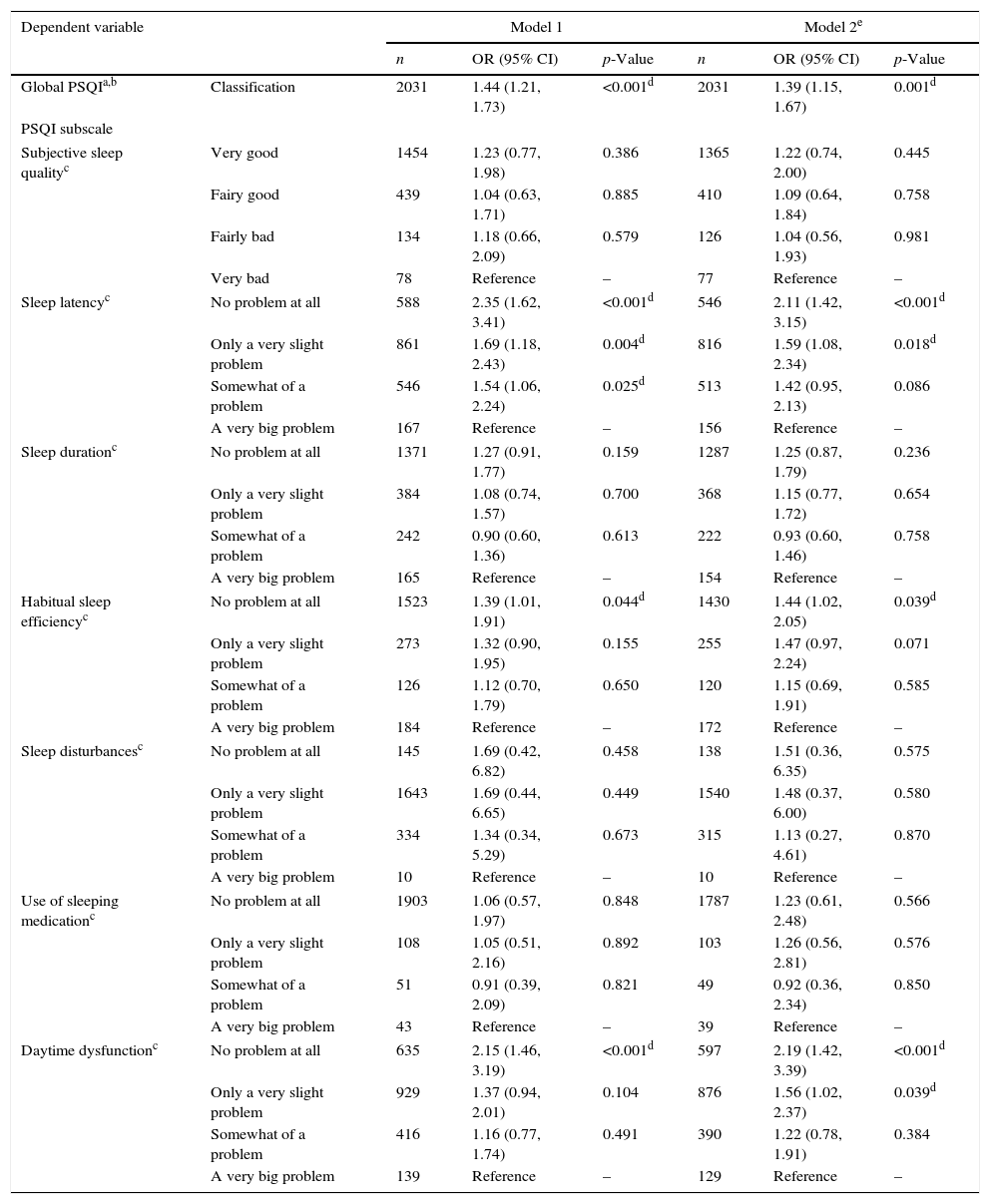
Regression models were made to ascertain the association of late-night cell phone use with sleep problems (Table 3). The first model was un-adjusted; the second was adjusted for potential confounders including gender, age, GPA, health status, and physical activity. Therefore, the association between overall PSQI score (good vs. poor) and late-night cell phone use (no, yes) was performed by a binary logistic regression model. The results of Model 2 showed that late-night cell phone users were 1.39 times more likely to have a poor sleep quality than non-users (p-value<0.001). Multinomial logistic regression analyses were made to investigate the relationship between each of the PSQI subscales (subjective sleep quality, sleep latency, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction) and late-night cell phone use (no, yes). As presented in Table 3, in the sleep latency PSQI subscale, those who were not late-night cell phone user were 1.22 times likely to be in the “no problem at all” group than in “a very big problem” group (p-value<0.001). Moreover, the odds ratio of being in the “only a very slight problem” group for non-users was 1.59 times more likely than to be in the “a very big problem” group regarding sleep latency (p-value=0.018). In the habitual sleep efficiency PSQI subscale, the odds ratios of being in the “no problem at all” group for non cell phone users was 1.44 times greater than to be in “a very big problem” group. Furthermore, in the daytime dysfunction PSQI subscale, non cell phone users were 2.19 times likely to be in “no problem at all” group than in “a very big problem” group (p-value<0.001). In this PSQI subscale, the odds ratio of being in “only a very slight problem” group for non-users were 1.56 times greater than to be in “a very big problem” group (p-value=0.039).
Association of late cell phone use and sleep disturbances in binary and multinomial logistic regression models.
| Dependent variable | Model 1 | Model 2e | |||||
|---|---|---|---|---|---|---|---|
| n | OR (95% CI) | p-Value | n | OR (95% CI) | p-Value | ||
| Global PSQIa,b | Classification | 2031 | 1.44 (1.21, 1.73) | <0.001d | 2031 | 1.39 (1.15, 1.67) | 0.001d |
| PSQI subscale | |||||||
| Subjective sleep qualityc | Very good | 1454 | 1.23 (0.77, 1.98) | 0.386 | 1365 | 1.22 (0.74, 2.00) | 0.445 |
| Fairy good | 439 | 1.04 (0.63, 1.71) | 0.885 | 410 | 1.09 (0.64, 1.84) | 0.758 | |
| Fairly bad | 134 | 1.18 (0.66, 2.09) | 0.579 | 126 | 1.04 (0.56, 1.93) | 0.981 | |
| Very bad | 78 | Reference | – | 77 | Reference | – | |
| Sleep latencyc | No problem at all | 588 | 2.35 (1.62, 3.41) | <0.001d | 546 | 2.11 (1.42, 3.15) | <0.001d |
| Only a very slight problem | 861 | 1.69 (1.18, 2.43) | 0.004d | 816 | 1.59 (1.08, 2.34) | 0.018d | |
| Somewhat of a problem | 546 | 1.54 (1.06, 2.24) | 0.025d | 513 | 1.42 (0.95, 2.13) | 0.086 | |
| A very big problem | 167 | Reference | – | 156 | Reference | – | |
| Sleep durationc | No problem at all | 1371 | 1.27 (0.91, 1.77) | 0.159 | 1287 | 1.25 (0.87, 1.79) | 0.236 |
| Only a very slight problem | 384 | 1.08 (0.74, 1.57) | 0.700 | 368 | 1.15 (0.77, 1.72) | 0.654 | |
| Somewhat of a problem | 242 | 0.90 (0.60, 1.36) | 0.613 | 222 | 0.93 (0.60, 1.46) | 0.758 | |
| A very big problem | 165 | Reference | – | 154 | Reference | – | |
| Habitual sleep efficiencyc | No problem at all | 1523 | 1.39 (1.01, 1.91) | 0.044d | 1430 | 1.44 (1.02, 2.05) | 0.039d |
| Only a very slight problem | 273 | 1.32 (0.90, 1.95) | 0.155 | 255 | 1.47 (0.97, 2.24) | 0.071 | |
| Somewhat of a problem | 126 | 1.12 (0.70, 1.79) | 0.650 | 120 | 1.15 (0.69, 1.91) | 0.585 | |
| A very big problem | 184 | Reference | – | 172 | Reference | – | |
| Sleep disturbancesc | No problem at all | 145 | 1.69 (0.42, 6.82) | 0.458 | 138 | 1.51 (0.36, 6.35) | 0.575 |
| Only a very slight problem | 1643 | 1.69 (0.44, 6.65) | 0.449 | 1540 | 1.48 (0.37, 6.00) | 0.580 | |
| Somewhat of a problem | 334 | 1.34 (0.34, 5.29) | 0.673 | 315 | 1.13 (0.27, 4.61) | 0.870 | |
| A very big problem | 10 | Reference | – | 10 | Reference | – | |
| Use of sleeping medicationc | No problem at all | 1903 | 1.06 (0.57, 1.97) | 0.848 | 1787 | 1.23 (0.61, 2.48) | 0.566 |
| Only a very slight problem | 108 | 1.05 (0.51, 2.16) | 0.892 | 103 | 1.26 (0.56, 2.81) | 0.576 | |
| Somewhat of a problem | 51 | 0.91 (0.39, 2.09) | 0.821 | 49 | 0.92 (0.36, 2.34) | 0.850 | |
| A very big problem | 43 | Reference | – | 39 | Reference | – | |
| Daytime dysfunctionc | No problem at all | 635 | 2.15 (1.46, 3.19) | <0.001d | 597 | 2.19 (1.42, 3.39) | <0.001d |
| Only a very slight problem | 929 | 1.37 (0.94, 2.01) | 0.104 | 876 | 1.56 (1.02, 2.37) | 0.039d | |
| Somewhat of a problem | 416 | 1.16 (0.77, 1.74) | 0.491 | 390 | 1.22 (0.78, 1.91) | 0.384 | |
| A very big problem | 139 | Reference | – | 129 | Reference | – | |
OR, odds ratio; 95% CI, 95% confidence interval.
The main objective of this study was to assess the relationship of late-night cell phone use (after 9p.m.) with sleep parameters such as its duration and quality. The present findings showed that the use of cell phones after 9p.m. was associated with poorer sleep quality, later wake-up time, and higher sleep latency, but it was not directly associated with sleep duration.
Between 2003 and 2008, there were more than 900 million new cell phone subscribers worldwide.15 A study implied that the worldwide proportion of subscribing to cell phones has increased from 5% in 1995 to more than 70% current users in 2010.10 Nowadays, cell phones provide their users with various ways of communication, such as calling, texting, sending e-mails; they also allow users to interact with others on social networks, using the internet, sharing videos and pictures, and using different software applications. Considering the mobile nature of cell phones, they can be used anywhere and at anytime, unlike conventional computers.16,17
Surprisingly, a large portion of adolescents are not aware of the adverse effects of using electronic media such as cell phones in bed; they wrongly believe that these media might help them sleep.5 For many individuals, media use has become connected with their personal sleep routine. It is proposed that cell phone use might be associated with reduced sleep quantity and quality, as well as sleeping problems. Fobian et al.18 indicated that bedtime media use and being awaken by a cell phone is associated with lower sleep efficiency in adolescents. According to a study by Lemola et al., electronic media use at night is associated with sleep disturbance, which could also be a partial mediator for the development of depressive symptoms.19 A cross-sectional study among 3139 American adolescents indicated that bedtime use of communication technologies is associated with insomnia and daytime sleepiness.20 It should be noted that sleep displacements appear to be at a higher level among children and adolescents than in other age groups. The stressful and sometimes irritating content of media is suggested as the underlying factor regarding how cell phone use may affect sleep.21
Physical activity and BMI were also considered in the present as two important variables, and their association with sleep parameters was investigated. The authors found that cell phone use after 9p.m. was significantly associated with a number of sleep-related variables. Those who used cell phones after 9p.m. had higher levels of sleep latency and delayed wake-up time than non-users. No significant relationship was observed between late-night cell phone use and sleep duration. This finding is in line with a study among Taiwanese adolescents, which reported no significant relationship between cell phone use and sleep duration.22 Likewise, a study among Canadian children found no significant relationship between using cell phones for either chatting or texting at night with sleep duration.23 However, a study in United Kingdom showed that the use of cell phones reduced total sleep duration for as long as 21min.24 In another research in the United Kingdom, cell phone use was associated with 45min decrease in sleep duration.25 Another study reported that sending at least one text message late night was extremely prevalent and could affect the sleep duration.14
Using the data collected by the PSQI questionnaire, it was observed that those who used cell phones after 9p.m. had a poorer sleep quality. Moreover, those with a better quality sleep had shorter duration of cell phone use than those with poor sleep quality; moreover, the use of cell phones after 9p.m. had inverse association with sleep and its related variables. The present findings are consistent with some previous reports. Studies among adults demonstrated similar findings and showed that using cell phones after the lights out had negative impacts on sleep and its quality.21,26 The experience on such associations in the pediatric age group is limited. A study in Japanese adolescents showed that using cell phones after lights out was associated with sleep disturbances including short sleep duration, poor sleep quality, daytime sleepiness, and insomnia.5 A study among American high-school students showed that use or perceived need of using cell phones during normal sleeping hours may contribute to daytime sleepiness, which is in turn related to poor sleep quality.20
The present findings showed that physical activity was positively associated with both sleep quality and quality. Participants who were physically active had lower sleep latency than their sedentary peers. Moreover, total sleep duration and sleep quality were higher in physically active participants. A study among Swedish adolescents reported that higher levels of both subjective and objective physical activity resulted in more favorable subjective and objective sleep.27 In a study among Spanish adolescents, those with higher level of morning tiredness, an indicator of poor sleep quality, were less likely to take part in any kind of physical activity.28 A study on the relationship of physical activity and sleep parameters in American adolescents showed that physical activity was associated with remembering when tired.29
Study strengths and limitationsThe main limitation of the present study is its cross-sectional design. Some potential confounding factors were considered, but other variables not considered in the present study may be associated with both sleeping and late-night cell phone use in either a positive or negative way. Moreover, the cut-off for sufficient sleep time was 8h; given that the use of another cut-off to stratify the sleep into poor and sufficient would lead to different results, the authors consider this fact as a limitation of the present study. Assessing the correlation between sleep and academic performance was only possible in the adolescent age range; therefore, it is reasonable to think that the present findings may not be significant in other age groups. The main strength of this study is its large sample size and the fact that participants with various socio-demographic characteristics were recruited. Furthermore, to the best of the authors’ knowledge, this is the first large population based study of its kind in Iran.
In this study, late-night cell phone use was associated with poorer sleep quality in adolescents. It was associated with sleep latency and wake-up time, however it was not directly associated with sleep duration. Adolescents who were physically active had better sleep quality and quantity. Public awareness should be increased about the adverse health effects of late-night cell phone use by adolescents.
FundingThis study was funded by a grant of the Research Institute for Primordial Prevention of Non-Communicable Disease, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Amra B, Shahsavari A, Shayan-Moghadam R, Mirheli O, Moradi-Khaniabadi B, Bazukar M, et al. The association of sleep and late-night cell phone use among adolescents. J Pediatr (Rio J). 2017;93:560–7.