To evaluate and correlate, before and after the therapeutic intervention, the behavioral problem scores evaluated by the CBCL/6-18 questionnaire and the quality of life indexes evaluated by the PedsQL™ 4.0 in patients with monosymptomatic nocturnal enuresis.
MethodAfter the initial evaluation and completion of the CBCL/6-18 questionnaire, a multidisciplinary evaluation and completion of the PedsQL™ 4.0 questionnaire was performed. Of the initially evaluated 140 children and adolescents aged 6–16 years, 58 were excluded due to non-monosymptomatic enuresis or associated comorbidities. Of the initially included 82 patients, who were randomized to three treatment groups, 59 completed the CBCL/6-18 and PedsQL™ 4.0 questionnaires at the end of the treatment and were included in this study. The α error was set at 5% for ruling out the null hypothesis.
ResultsOf the total of 59 participants, 45.8% responded with total success, 23.7% were partially successful, 23.7% did not reach the improvement criteria, and 6.8% gave up the treatment. There was a significant increase in quality of life indexes and a reduction of post-intervention behavioral problem scores, in the three proposed modalities, in patients who had a total or partial response to treatment. There was no correlation between higher scores of pre-treatment behavior problems and therapeutic failure.
ConclusionsOnly the participants who successfully responded to interventions showed improvement in quality of life and behavioral problems, which indicates that enuresis is a primary problem that has a negative impact on these parameters. The authors suggest that it is possible to achieve success in the treatment of monosymptomatic enuresis, even in patients with high pre-intervention behavioral problem scores.
Avaliar e relacionar, pré e pós-intervenção terapêutica, em pacientes com enurese noturna monossintomática, os escores de problemas de comportamento, avaliados pelo questionário CBCL/6-18, e os índices de qualidade de vida, avaliados pelo PedsQL™ 4.0.
MétodoApós avaliação inicial e preenchimento CBCL6/18, procedeu-se avaliação multidisciplinar e preenchimento do PedsQL™ 4.0. Das 140 crianças e adolescentes de 6 a 16 anos inicialmente avaliados, 58 foram excluídos por enurese não monossintomática ou comorbidades associadas. Dos 82 pacientes inicialmente incluídos e randomizados em três grupos de tratamento, 59 preencheram o CBCL/6-18 e PedsQL™ 4.0 no fim do tratamento e puderam ser incluídos neste trabalho. O erro alfa foi estabelecido em 5% para descarte da hipótese de nulidade.
ResultadosDos 59 participantes 45,8% responderam com sucesso total, 23,7% tiveram sucesso parcial, 23,7% não atingiram critério de melhoria e 6,8% desistiram do tratamento. Verificou-se aumento significativo dos índices de qualidade de vida e redução dos escores de problemas de comportamento pós-intervenção, nas três modalidades propostas, nos pacientes que obtiveram resposta total ou parcial ao tratamento. Não se demonstrou correlação entre maiores escores de problemas de comportamento pré-tratamento e insucesso terapêutico.
ConclusõesApenas os participantes que responderam com sucesso às intervenções, melhoraram em sua qualidade de vida e problemas comportamentais, o que indica que a enurese é um problema primário que impacta negativamente esses parâmetros. Sugere-se que é viável obter sucesso no tratamento da enurese monossintomática, mesmo em pacientes com altos escores de problemas de comportamento pré-intervenção.
Nocturnal enuresis has been described as one of the most prevalent and chronic problems of childhood.1 The standardization proposal presented by the International Childhood's Continence Society (ICCS)2 defines that enuresis is characterized by episodes of involuntary urination during sleep, in clothing or in bed, in children over 5 years of age with no other clinical condition that can explain them. As for the frequency, episodes should occur at least once a month and may involve variable amounts of nocturnal urinary loss.
The current categorization of the International Childhood's Continence Society (ICCS)2 divides enuresis into monosymptomatic, when there are no other lower urinary tract symptoms, and non-monosymptomatic, when accompanied by daytime symptoms such as containment maneuvers, urinary urgency, altered urination frequency, or diurnal urinary incontinence.3
Overall, the prevalence is higher among males during the childhood years, with values at around 7 years of age ranging from 15% to 22% in boys and 7% to 15% in girls, with similar values for both genders in adolescence.4 In Brazil, this prevalence is 10.6%, being 11.7% in males and 8.3% in females.5
Currently, enuresis is understood as a disorder whose genetic basis is influenced by physiological and environmental aspects.6 It is suggested that enuresis is transmitted by high-penetrance, autosomal dominant inheritance, since according to some studies, the probability of developing enuresis increases from 43% when one parent has a history of enuresis, to 77% when this antecedent is common to both parents, decreasing to 15% in families with no history of the problem.7
The pathogenesis of this condition is understood through three mechanisms: high thresholds for arousal to full bladder signs, nocturnal polyuria, and nocturnal detrusor hyperactivity.2,3
There is no evidence that behavioral problems and poor quality of life lead to urinary control difficulty at night, but there are studies that demonstrate an improvement in behavioral problems after enuresis treatment, suggesting that these problems may be due to an initial picture of enuresis; however, there are still divergences in the literature about this statement.8
In any case, enuresis is a clinical condition with a multifactorial etiology that generates great impacts on social relationships, self-esteem, family relationships, and even the academic life of children and adolescents with nocturnal enuresis.9
The aim of this study was to evaluate the scores of behavioral problems and quality of life, pre- and post-treatment, as well as their association, in three different treatment modalities for monosymptomatic nocturnal enuresis.
MethodsAfter publicizing the study, carried out predominantly through the Internet, the interested parties contacted the team responsible for the project, through telephone contact or e-mail, and the parents/guardians were instructed to complete the Child Behavior Checklist (CBCL/6-18) at home and return it by post, together with the socioeconomic level assessment (evaluated by the Brazilian Economic Classification Criteria). After receiving this documentation, a medical screening interview (with parents and child) was scheduled, during which the Pediatric Quality of Life Questionnaire (PedsQL™ 4.0) was applied.
The study involved a partnership between the Pediatric Nephrology Unit of the ICr HCFMUSP Department of Pediatrics (Instituto da Criança, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo); the ICr HCFMUSP Clinical Neurophysiology Unit; the Physiotherapy Division of the Physiotherapy, Speech, and Occupational Therapy Care Unit of the HCFMUSP Central Institute; and the Behavioral Therapy Sector of the FMUSP Institute of Psychology, which were associated in order to carry out an initial multidisciplinary evaluation, in an outpatient setting at the HCFMUSP, which could provide a full and complete discussion of the patient's case in a single day.
The main objective of this multidisciplinary evaluation was the observation of monosymptomatic nocturnal enuresis. Inclusion criteria for the study were the following: patients aged 6–16 years, of both genders, diagnosed with monosymptomatic nocturnal enuresis according to the ICCS criteria,2 who had undergone a complete multidisciplinary evaluation, and whose parents/guardians had signed the Informed Consent. The exclusion criteria were: non-monosymptomatic nocturnal enuresis, urinary infection that occurred less than one year from the initial visit, enuresis associated with genetic syndromes, nocturnal enuresis secondary to underlying disease (hypercalciuria, diabetes mellitus, diabetes insipidus, sickle-cell anemia, sleep apnea, hypertension, chronic kidney disease, neuropathies), and attention deficit disorder with or without hyperactivity.
Of a total of 140 initially evaluated children and adolescents, 52/140 participants were excluded due to: Non-monosymptomatic nocturnal enuresis (NMNE) in 27/140 cases (19.3%), hypercalciuria in 4/140 cases (2.9%), renal tubular acidosis in 3/140 cases (2.1%), one case of attention deficit hyperactivity disorder (ADHD; 0.7%), and 17/140 cases (12.1%) because they did not complete the diagnostic investigation. Of the 88/140 (62.8%) remaining participants, one was spontaneously cured while waiting for polysomnography (PSG). The PSG was performed in 87 participants, and 6/87 (6.9%) of them had a diagnosis of apnea, being referred for specialized follow-up. Of the 82/140 (58.6%) patients diagnosed with monosymptomatic nocturnal enuresis (MNE), 62/82 were males (75.6%) and 20/82 were females (24.4%), with a mean age of 9.5 years (±2.66); 72/82 (85.2%) had primary type enuresis and were randomized to three treatment groups: alarm and desmopressin, or isolated use of alarm or desmopressin.
Categorical variables were described as percentages and their respective 95% confidence intervals. Continuous variables were described as means and standard deviation, or median and interquartile range, if they were non-parametric.
Subsequently, the analyses were performed using the paired Student's t-test and Wilcoxon's test, if they were non-parametric. For comparison between groups, the ANOVA single factor test was also used.
The alpha error was set at 5% for ruling out the null hypothesis. The evaluation of the treatment outcomes followed the criteria established by ICCS10:
- •
Total response: reduction of at least 90% of enuretic episodes.
- •
Partial response: reduction of 50–89% of enuretic episodes.
- •
No response: reduction of 0–49% of enuretic episodes.
The present study was approved by CAPPESQ – HCFMUSP and is included as a subproject of a larger project entitled: “Comparative evaluation of the efficacy of the isolated and combined use of nocturnal alarm and desmopressin in the treatment of monosymptomatic nocturnal enuresis,” CAPPESQ No. 0649/10 and FAPESP No. 2011/17589.
ResultsThe total number of patients described in this study is 59 children and adolescents aged 6 to 16 years, in whom pre-and post-treatment comparative analysis of CBCL/6-18 and PedsQL™ 4.0 instruments was performed. After randomization, 20 participants received the monotherapy treatment of alarm, 21 received the combined treatment with alarm and desmopressin, and 18 received treatment with desmopressin (1-desamino-8-d-arginine vasopressin), with an initial dose of 0.2mg, which could be increased to 0.4mg if the initial dose did not reduce the number of nocturnal enuresis episodes by 50%. A statistical power calculation was performed, and its index was (1−β)=0.967.
Of the total of 59 participants, 45.8% showed total response, 23.7% partial response, 23.7% did not reach the improvement criteria, and 6.8% gave up treatment.
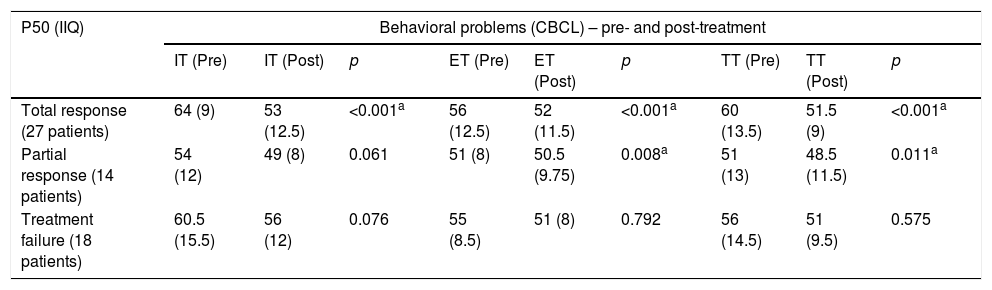
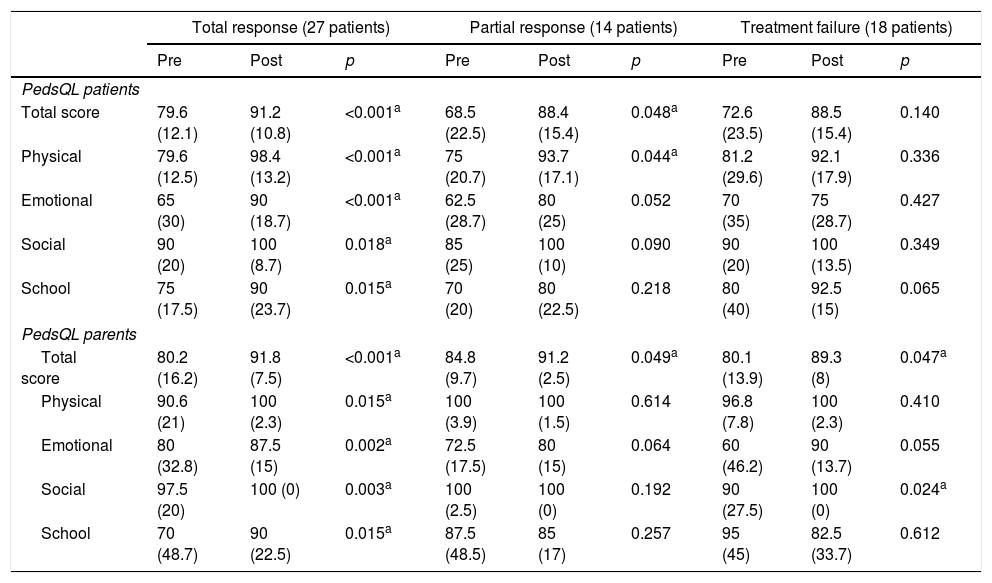
Tables 1 and 2 show, respectively, the comparison of behavioral problem indexes before and after the interventions, and the quality of life scores before and after treatment.
Comparison between pre- and post-treatment behavioral problem scores by treatment outcome category in 59 patients with monosymptomatic nocturnal enuresis.
| P50 (IIQ) | Behavioral problems (CBCL) – pre- and post-treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| IT (Pre) | IT (Post) | p | ET (Pre) | ET (Post) | p | TT (Pre) | TT (Post) | p | |
| Total response (27 patients) | 64 (9) | 53 (12.5) | <0.001a | 56 (12.5) | 52 (11.5) | <0.001a | 60 (13.5) | 51.5 (9) | <0.001a |
| Partial response (14 patients) | 54 (12) | 49 (8) | 0.061 | 51 (8) | 50.5 (9.75) | 0.008a | 51 (13) | 48.5 (11.5) | 0.011a |
| Treatment failure (18 patients) | 60.5 (15.5) | 56 (12) | 0.076 | 55 (8.5) | 51 (8) | 0.792 | 56 (14.5) | 51 (9.5) | 0.575 |
IT, internalizing problems; ET, externalizing problems; TT, total problems.
Comparison between quality of life scores (assessed by patients and parents) pre- and post-treatment by treatment outcome category in 59 patients with monosymptomatic nocturnal enuresis.
| Total response (27 patients) | Partial response (14 patients) | Treatment failure (18 patients) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | p | Pre | Post | p | Pre | Post | p | |
| PedsQL patients | |||||||||
| Total score | 79.6 (12.1) | 91.2 (10.8) | <0.001a | 68.5 (22.5) | 88.4 (15.4) | 0.048a | 72.6 (23.5) | 88.5 (15.4) | 0.140 |
| Physical | 79.6 (12.5) | 98.4 (13.2) | <0.001a | 75 (20.7) | 93.7 (17.1) | 0.044a | 81.2 (29.6) | 92.1 (17.9) | 0.336 |
| Emotional | 65 (30) | 90 (18.7) | <0.001a | 62.5 (28.7) | 80 (25) | 0.052 | 70 (35) | 75 (28.7) | 0.427 |
| Social | 90 (20) | 100 (8.7) | 0.018a | 85 (25) | 100 (10) | 0.090 | 90 (20) | 100 (13.5) | 0.349 |
| School | 75 (17.5) | 90 (23.7) | 0.015a | 70 (20) | 80 (22.5) | 0.218 | 80 (40) | 92.5 (15) | 0.065 |
| PedsQL parents | |||||||||
| Total score | 80.2 (16.2) | 91.8 (7.5) | <0.001a | 84.8 (9.7) | 91.2 (2.5) | 0.049a | 80.1 (13.9) | 89.3 (8) | 0.047a |
| Physical | 90.6 (21) | 100 (2.3) | 0.015a | 100 (3.9) | 100 (1.5) | 0.614 | 96.8 (7.8) | 100 (2.3) | 0.410 |
| Emotional | 80 (32.8) | 87.5 (15) | 0.002a | 72.5 (17.5) | 80 (15) | 0.064 | 60 (46.2) | 90 (13.7) | 0.055 |
| Social | 97.5 (20) | 100 (0) | 0.003a | 100 (2.5) | 100 (0) | 0.192 | 90 (27.5) | 100 (0) | 0.024a |
| School | 70 (48.7) | 90 (22.5) | 0.015a | 87.5 (48.5) | 85 (17) | 0.257 | 95 (45) | 82.5 (33.7) | 0.612 |
The pre-treatment behavioral problem scores and the intervention outcomes were compared using Wilcoxon's test, disclosing no significant differences between them in patients with total or partial response, no response, or those who gave up treatment (p=0.124).
DiscussionData from the present study confirm the higher prevalence of nocturnal enuresis in male patients, as shown by the greater number of male patients.1,5
The focus of the present study was to identify whether improving behavioral problems and quality of life scores depended on whether the patient had a total or partial response to treatment, or whether those indexes would improve regardless of treatment outcome, motivated by the inclusion and care offered by the multiprofessional team during the follow-up. These data are not clear in the literature, and there are disagreements on these points.8,11 For this purpose, the association between the change in behavioral problem scores and the therapeutic outcome was analyzed. However, it was verified that only those patients who achieved treatment success (total response and partial response) showed a decrease in behavioral problem scores, whereas patients who had treatment failure (no response and those who gave up treatment) did not show significant differences in pre- and post-treatment behavior problem scores.
This finding differs from the results of the study by Pereira et al.,12 in which the researchers analyzed, based on a database, the scores of behavioral problems pre- and post-treatment with alarm, evaluated by the CBCL/6-18. Patients in that study showed behavioral problem improvement after treatment of enuresis, regardless of the outcome success.
In the present study, regardless of the type of treatment, medication or alarm, the alarm used in two of the therapeutic subgroups, behavioral problem improvement in patients with total or partial response to treatment shows that enuresis is a primary problem, either generating or in parallel with the behavioral problems. This is also the conclusion of the study by Santos and Silvares,13 which points to enuresis as a possible risk factor for the onset of behavioral problems and not the opposite.
The present study also aimed to compare the scores of pre-treatment behavior problems with the intervention outcomes to evaluate if they could be a possible complicating factor for the successful treatment of monosymptomatic nocturnal enuresis. It was verified that there were no significant differences, both for the internalizing problems, as well as for the externalizing and total problems in the four types of outcomes observed, namely: total response, partial response, absence of response, and giving up the treatment. Higher rates of pre-treatment behavioral problems do not imply a failure of monosymptomatic nocturnal enuresis management. This finding confirms the studies of Sousa14 and Ferrari15 and contradicts the conclusions of Houts,16 and Arantes,17 who suggest that patients with higher scores of behavioral problems would have a significant impact, hindering successful enuresis therapeutic management.
Regarding the analysis of the association between quality of life assessed by PedsQL 4.0™ and the treatment outcome for monosymptomatic nocturnal enuresis, the present study confirms that both the patients’ own views and their parents’ views improved the quality of life indexes only for patients who were successful in their treatment, especially those who obtained total response. As well as with behavioral problems, enuresis negatively impacts the patient's quality of life as a primary problem. These data corroborate a study that evaluated 70 children with different types of enuresis (monosymptomatic nocturnal enuresis, non-monosymptomatic enuresis, diurnal enuresis) seeking to associate the treatment of these clinical conditions to the patients’ quality of life. The authors concluded that patients who responded successfully to enuresis treatment achieved a significant quality of life improvement.18
Several studies indicate that the clinical pictures of enuresis and other chronic diseases have a negative impact on quality of life and result in higher scores for behavioral problems when compared to control groups.19–24 These studies suggest that psychological support would be important for children with such clinical conditions, but they do not assess the association between therapeutic success, behavioral problems, and quality of life; or, in other words, the question remains whether the psychological condition leads to the physical illness, or vice versa. To the best of the authors’ knowledge, the present study is unique in approaching this topic in monosymptomatic nocturnal enuresis. It has been confirmed that, from both parents’ and patients’ viewpoints, post-treatment quality of life indexes increased only for patients with therapeutic success and consequent improvement of enuresis, and it is postulated that enuresis is a primary problem, which generates low quality of life and behavioral problems, and that its successful treatment is crucial for a healthier life.25,26
The finding that adult individuals with a previous history of nocturnal enuresis in childhood may have an abnormal neuronal response to emotional stimuli suggests that nocturnal enuresis may affect the individual both psychologically and neurologically.27 These findings emphasize the importance of the present study's findings and indicate the need to promote effective treatment of enuresis.
In conclusion, only participants who successfully responded to interventions improved their scores regarding behavioral problems and quality of life, which indicates that enuresis is a primary problem that negatively affects these parameters. These results suggest that enuresis treatment is feasible, and that treatment can be successful regardless of high pre-intervention scores for behavioral problems.
FundingFAPESP process No. 2011/17589-1.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Sousa e Silva GJ, Sammour SN, Ferraro AA, Koch VH. Study of the profile of behavioral problems and quality of life indexes in a pediatric cohort of monosymptomatic enuresis. J Pediatr (Rio J). 2019;95:188–93.
Article associated with the Postgraduate Program of the Pediatrics Department of Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil.