To analyze economic inequality (absolute and relative) due to family income in relation to the occurrence of preterm births in Southern Brazil.
MethodsFour birth cohort studies were conducted in the years 1982, 1993, 2004, and 2011. The main exposure was monthly family income and the primary outcome was preterm birth. The inequalities were calculated using the slope index of inequality and the relative index of inequality, adjusted for maternal skin color, education, age, and marital status.
ResultsThe prevalence of preterm births increased from 5.8% to approximately 14% (p-trend<0.001). Late preterm births comprised the highest proportion among the preterm births in all studies, although their rates decreased over the years. The analysis on the slope index of inequality demonstrated that income inequality arose in the 1993, 2004, and 2011 studies. After adjustment, only the 2004 study maintained the difference between the poorest and the richest subjects, which was 6.3 percentage points. The relative index of inequality showed that, in all studies, the poorest mothers were more likely to have preterm newborns than the richest. After adjustment for confounding factors, it was observed that the poorest mothers only had a greater chance of this outcome in 2004.
ConclusionIn a final model, economic inequalities resulting from income were found in relation to preterm births only in 2004, although a higher prevalence of prematurity continued to be observed in the poorest population, in all the studies.
Analisar a iniquidade econômica (absoluta e relativa) decorrente da renda familiar na ocorrência de prematuros no Sul do Brasil.
MétodosForam realizados quatro estudos do tipo coorte de nascimentos nos anos de 1982, 1993, 2004 e 2011. A exposição principal foi a renda familiar mensal e o desfecho foi nascer prematuro. Foram calculadas as iniquidades através do slope index of inequality e o relative index of inequality, ajustados por cor da pele, escolaridade, idade e estado civil maternos.
ResultadosHouve aumento da prevalência de prematuros de 5,8 para cerca de 14% (p de tendência <0,001). O prematuro tardio foi a maior proporção encontrada dentre os que nasceram prematuros em todos os estudos, embora reduzindo suas taxas ao longo dos anos. A análise do slope index of inequality demonstrou iniquidade decorrente de renda nos estudos de 1993, 2004 e 2011. Após ajuste, apenas o estudo de 2004 manteve a diferença entre os mais pobres e os mais ricos, que foi de 6.3 pontos percentuais. Através do relative index of inequality, observou-se que, em todos os estudos, as mães mais pobres tiveram maior chance de ter prematuros, em comparação com as mais ricas. O ajuste para fatores de confusão demonstrou a manutenção dos mais pobres com maior chance do desfecho apenas em 2004.
ConclusãoNo modelo final, iniquidades econômicas decorrentes da renda foram encontradas no nascimento de prematuros apenas em 2004, apesar da manutenção de maior ocorrência da prematuridade na população mais pobre, em todos os estudos.
Global occurrence of preterm birth (PT) ranges from 3.8% to 17.5% of live births, being lower in high-income countries than in low/medium-income countries.1 Brazil is among the ten countries with the largest numbers of PT.1,2
Maternal risk factors for spontaneous PT may or may not be prior to conception and include underprivileged socioeconomic position, black ethnicity, low education, low height, age below 20 or over 35, being single, exhausting work, or presence of maternal diseases such as high blood pressure and diabetes.2–5
The relationship of poverty with prematurity and higher neonatal mortality rates has been well-recognized.2,3 Low-income families may share other risk factors that can influence inequity, such as black ethnicity, lower levels of education, and unemployment.2,5,6
Socioeconomic inequalities remain a major challenge to healthcare policies or strategies in low/medium-income countries. The slope index of inequality (SII) and the relative index of inequality (RII) can be used to assess inequalities, showing the magnitudes of absolute and relative differences, respectively, of indicators of socioeconomic position, in comparison with temporal trends of neonatal outcomes in epidemiological studies.7,8
The present study aimed to analyze inequalities of family income (absolute and relative) in relation to occurrence of PT in four birth cohorts conducted in Pelotas, RS, a city located in the southern region of Brazil, in the years 1982, 1993, 2004, and 2011.
MethodsOver the course of 1982, 1993, and 2004, all births in hospitals were identified and those whose mothers lived in the urban area of Pelotas were included in the cohorts. Soon after birth, the mothers were interviewed using a previously tested structured questionnaire and the newborns were examined and measured. Methodological details of each cohort (1982, 1993, and 2004) were described in previous publications.9–11
The 2011 data from the multicenter study International Fetal and Newborn Growth Consortium for the 21st Century (Intergrowth 21st) was made available. The inclusion criteria, sampling, and logistics were similar to those of the other cohort studies.12
The outcome variable was PT, i.e. birth at a gestational age (GA)<37 weeks.4 GA in completed weeks can be determined from: (i) the time elapsed since the first day of the last menstrual period (LMP); (ii) the estimated birth date according to early obstetric ultrasound (US); and/or (iii) newborn physical examination using the Dubowitz score.13 In all of the cohort studies, LMP was the method used to calculate GA. In 20% of the neonates in 1982, GA was determined by the Dubowitz score.10 In 1993, 2004, and 2011, GA was calculated by LMP complemented by physical examination and US for the last two cohorts.9,11,12 Based on GA, PT can be subdivided as follows: extremely preterm (<28 completed weeks of gestation), very preterm (28≥ to <32 weeks), or moderately preterm (32≥ to <37 weeks). Moderately PT can be further divided to concentrate on the early end of full-term births (34–37 weeks), denominated late preterm birth (LPT), and on those with or without low birth weight (LBW), i.e., situations in which the birthweight was lower than 2500g.2
The main exposure was monthly family income (generally from one or both parents), calculated from the sum of the individual incomes collected as a continuous variable and later categorized into income quintiles. Potential confounding variables included mother's ethnicity, categorized as white, black, or others by the interviewer, and self-reported in 2011; mother's education in full years, expressed as four categories: <4 years, 5–8 years, 9–11 years, or ≥12 years; mother's age in full years, categorized as <20 years, 20–34 years, or ≥35 years; and mother's marital status, expressed as whether she was living with a partner or not, regardless of the legal status of the relationship.
The absolute and relative income inequalities were calculated using the SII and the RII, respectively. SII is obtained from logistic regression analysis on the outcome of PT, as the mean of the relative income rank, with values ranging from 0 to 1, calculated by ordering the groups from the lowest to the highest income quintiles to calculate the midpoint of the distribution in this ranking. Each mean point of each quintile was sited almost at 0.1, 0.3, 0.5, 0.7, and 0.9. SII resulted from regression on each result from the midpoint position and was interpreted as the absolute difference in outcome between the group of individuals at the lowest point of the distribution or the first quintile (Q1, the poorest) and the group of individuals at the highest point of the income distribution (Q5, the richest). When the slope of the regression line is flat, SII is 0. Positive values result from prematurity, and are more prevalent among richer subjects; in turn, negative values mean that this indicator is more prevalent among poorer subjects. RII was expressed by odds ratio (OR) with 95% confidence interval. The results were interpreted through comparison of income extremes; the difference between Q1 and Q5 and SII referred to absolute inequality, expressed as percentage points (PP), while the ratio of Q1–Q5 to RII indicated relative inequality based on the chance that the group of individuals might have the outcome. SII and RII determined a direct relationship with the level of inequality in the socioeconomic hierarchy.8,14
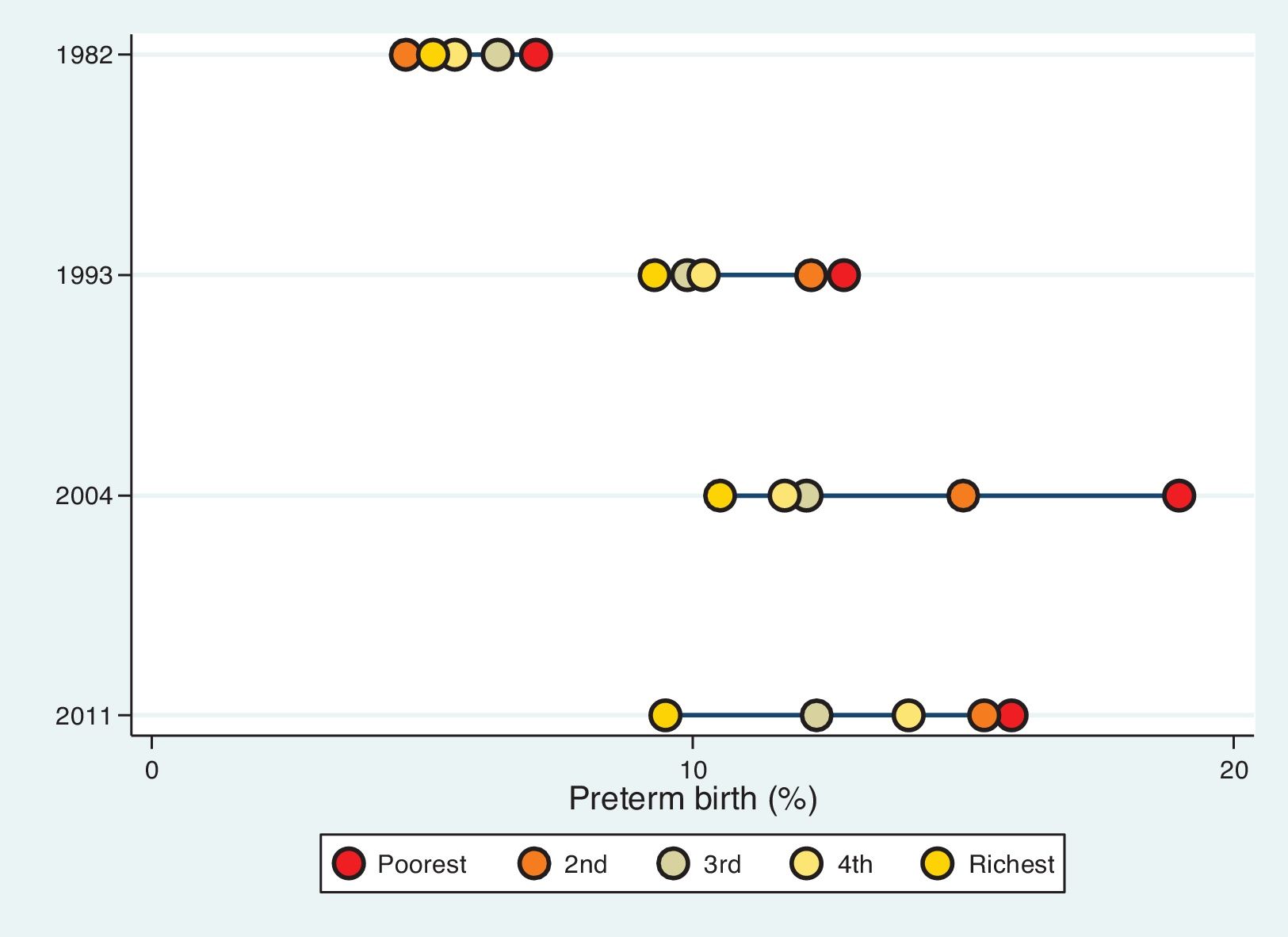
The inequality between income and the incidence of PT in the four studies was observed through the distance between income quintiles on an inequality graph (five-dot plots). It can be classified as a bottom pattern (the poorest very far from the others), top pattern (the richest very far from the others), or linear pattern (similar distances among the groups analyzed).7
The analyses were restricted to live births, as the definition of PT did not include stillbirths,2 and to single deliveries, avoiding repeated data from the same family (in case of twins). Newborns with malformations and/or congenital diseases were excluded, as soon as those were detected during the interviews or newborn physical examinations in the maternities.
The chi-squared test (X2) was used to compare the distribution of maternal characteristics in the four cohorts and, when possible, X2 for trend was calculated.
Adjusted analysis included the variables maternal ethnicity, education, age, and marital status in the final model, to determine the independent contributions of family income to the outcome.
All analyses were performed using the Stata 13.1 software (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX, USA).
Ethical approval for studies was not necessary in Brazil until 1996. However, all follow-ups conducted on the 1982 and 1993 cohorts after 1996 were approved. The Ethics Committee of the School of Medicine, Universidade Federal de Pelotas (UFPel) approved the 2004 study (021/2003) and the Intergrowth-21st (051/09).
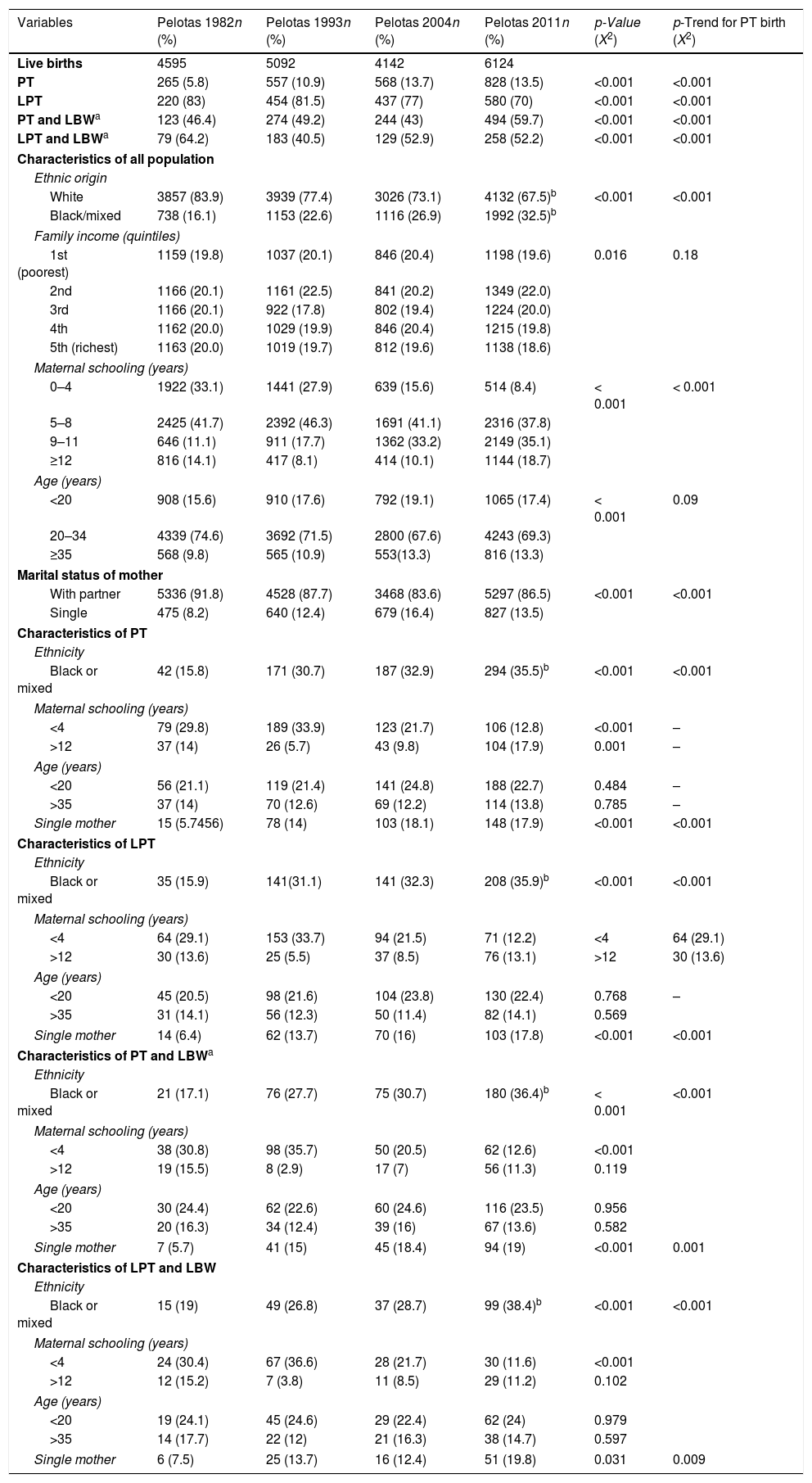
ResultsTable 1 summarizes the main frequencies of the variables evaluated in each cohort of newborns. There was an increase in the prevalence of PT from 5.8% to about 14% (p for trend <0.001) up to the year 2004 and stabilization in 2011. LPT showed the highest occurrence (approximately 80% of PT), with drops in the 2004 and 2011 studies. Higher numbers of PT associated with low birth weight were observed in 1993, with a reduction in 2004 and a new increase in 2011, accounting for almost 60% of PT. LPT with LBW was more prevalent in the 1982 study, was reduced in 1993, increased again in 2004, and remained stable in 2011 (Table 1).
Maternal and child characteristics of all births and of preterm (PT) birth and late preterm (LPT) with or without low birthweight in four birth cohort studies.
| Variables | Pelotas 1982n (%) | Pelotas 1993n (%) | Pelotas 2004n (%) | Pelotas 2011n (%) | p-Value (X2) | p-Trend for PT birth (X2) |
|---|---|---|---|---|---|---|
| Live births | 4595 | 5092 | 4142 | 6124 | ||
| PT | 265 (5.8) | 557 (10.9) | 568 (13.7) | 828 (13.5) | <0.001 | <0.001 |
| LPT | 220 (83) | 454 (81.5) | 437 (77) | 580 (70) | <0.001 | <0.001 |
| PT and LBWa | 123 (46.4) | 274 (49.2) | 244 (43) | 494 (59.7) | <0.001 | <0.001 |
| LPT and LBWa | 79 (64.2) | 183 (40.5) | 129 (52.9) | 258 (52.2) | <0.001 | <0.001 |
| Characteristics of all population | ||||||
| Ethnic origin | ||||||
| White | 3857 (83.9) | 3939 (77.4) | 3026 (73.1) | 4132 (67.5)b | <0.001 | <0.001 |
| Black/mixed | 738 (16.1) | 1153 (22.6) | 1116 (26.9) | 1992 (32.5)b | ||
| Family income (quintiles) | ||||||
| 1st (poorest) | 1159 (19.8) | 1037 (20.1) | 846 (20.4) | 1198 (19.6) | 0.016 | 0.18 |
| 2nd | 1166 (20.1) | 1161 (22.5) | 841 (20.2) | 1349 (22.0) | ||
| 3rd | 1166 (20.1) | 922 (17.8) | 802 (19.4) | 1224 (20.0) | ||
| 4th | 1162 (20.0) | 1029 (19.9) | 846 (20.4) | 1215 (19.8) | ||
| 5th (richest) | 1163 (20.0) | 1019 (19.7) | 812 (19.6) | 1138 (18.6) | ||
| Maternal schooling (years) | ||||||
| 0–4 | 1922 (33.1) | 1441 (27.9) | 639 (15.6) | 514 (8.4) | < 0.001 | < 0.001 |
| 5–8 | 2425 (41.7) | 2392 (46.3) | 1691 (41.1) | 2316 (37.8) | ||
| 9–11 | 646 (11.1) | 911 (17.7) | 1362 (33.2) | 2149 (35.1) | ||
| ≥12 | 816 (14.1) | 417 (8.1) | 414 (10.1) | 1144 (18.7) | ||
| Age (years) | ||||||
| <20 | 908 (15.6) | 910 (17.6) | 792 (19.1) | 1065 (17.4) | < 0.001 | 0.09 |
| 20–34 | 4339 (74.6) | 3692 (71.5) | 2800 (67.6) | 4243 (69.3) | ||
| ≥35 | 568 (9.8) | 565 (10.9) | 553(13.3) | 816 (13.3) | ||
| Marital status of mother | ||||||
| With partner | 5336 (91.8) | 4528 (87.7) | 3468 (83.6) | 5297 (86.5) | <0.001 | <0.001 |
| Single | 475 (8.2) | 640 (12.4) | 679 (16.4) | 827 (13.5) | ||
| Characteristics of PT | ||||||
| Ethnicity | ||||||
| Black or mixed | 42 (15.8) | 171 (30.7) | 187 (32.9) | 294 (35.5)b | <0.001 | <0.001 |
| Maternal schooling (years) | ||||||
| <4 | 79 (29.8) | 189 (33.9) | 123 (21.7) | 106 (12.8) | <0.001 | – |
| >12 | 37 (14) | 26 (5.7) | 43 (9.8) | 104 (17.9) | 0.001 | – |
| Age (years) | ||||||
| <20 | 56 (21.1) | 119 (21.4) | 141 (24.8) | 188 (22.7) | 0.484 | – |
| >35 | 37 (14) | 70 (12.6) | 69 (12.2) | 114 (13.8) | 0.785 | – |
| Single mother | 15 (5.7456) | 78 (14) | 103 (18.1) | 148 (17.9) | <0.001 | <0.001 |
| Characteristics of LPT | ||||||
| Ethnicity | ||||||
| Black or mixed | 35 (15.9) | 141(31.1) | 141 (32.3) | 208 (35.9)b | <0.001 | <0.001 |
| Maternal schooling (years) | ||||||
| <4 | 64 (29.1) | 153 (33.7) | 94 (21.5) | 71 (12.2) | <4 | 64 (29.1) |
| >12 | 30 (13.6) | 25 (5.5) | 37 (8.5) | 76 (13.1) | >12 | 30 (13.6) |
| Age (years) | ||||||
| <20 | 45 (20.5) | 98 (21.6) | 104 (23.8) | 130 (22.4) | 0.768 | – |
| >35 | 31 (14.1) | 56 (12.3) | 50 (11.4) | 82 (14.1) | 0.569 | |
| Single mother | 14 (6.4) | 62 (13.7) | 70 (16) | 103 (17.8) | <0.001 | <0.001 |
| Characteristics of PT and LBWa | ||||||
| Ethnicity | ||||||
| Black or mixed | 21 (17.1) | 76 (27.7) | 75 (30.7) | 180 (36.4)b | < 0.001 | <0.001 |
| Maternal schooling (years) | ||||||
| <4 | 38 (30.8) | 98 (35.7) | 50 (20.5) | 62 (12.6) | <0.001 | |
| >12 | 19 (15.5) | 8 (2.9) | 17 (7) | 56 (11.3) | 0.119 | |
| Age (years) | ||||||
| <20 | 30 (24.4) | 62 (22.6) | 60 (24.6) | 116 (23.5) | 0.956 | |
| >35 | 20 (16.3) | 34 (12.4) | 39 (16) | 67 (13.6) | 0.582 | |
| Single mother | 7 (5.7) | 41 (15) | 45 (18.4) | 94 (19) | <0.001 | 0.001 |
| Characteristics of LPT and LBW | ||||||
| Ethnicity | ||||||
| Black or mixed | 15 (19) | 49 (26.8) | 37 (28.7) | 99 (38.4)b | <0.001 | <0.001 |
| Maternal schooling (years) | ||||||
| <4 | 24 (30.4) | 67 (36.6) | 28 (21.7) | 30 (11.6) | <0.001 | |
| >12 | 12 (15.2) | 7 (3.8) | 11 (8.5) | 29 (11.2) | 0.102 | |
| Age (years) | ||||||
| <20 | 19 (24.1) | 45 (24.6) | 29 (22.4) | 62 (24) | 0.979 | |
| >35 | 14 (17.7) | 22 (12) | 21 (16.3) | 38 (14.7) | 0.597 | |
| Single mother | 6 (7.5) | 25 (13.7) | 16 (12.4) | 51 (19.8) | 0.031 | 0.009 |
PT, preterm birth; LPT, late preterm birth; X2=chi-squared.
The predominant maternal ethnicity was white in all the studies, with increased proportions of black and other ethnicities in more recent studies. The proportion of maternal black ethnicity among PT (including LPT) was lower in 1982, but greater in 1993, 2004, and 2011; however, when PT was associated with LBW, it was similar or higher in all four cohorts. In relation to maternal education, an increase in the number of years of schooling occurred. Those less educated had a higher prevalence of PT and LPT with or without LBW, except in 1982. The prevalence of teenage mothers ranged from 15.6% to 19.1%, with the highest percentage in the 2004 cohort and a fall in 2011, while the proportion of mothers older than 35 years ranged from 9.8% to 13.3%, remaining stable in the last two studies. The presence of PT and LPT in teenage mothers, associated or not with LBW, was higher in all studied cohorts, especially in 2004 and 2011. Older mothers had comparable findings with teenagers, particularly for PT and LPT with LBW in 1982, and for PT in 2004 and 2011. The number of women who did not have a steady relationship increased from 8.2% to 16.4%, up to 2004, with a subsequent reduction to 13.5% in 2011. Single mothers had lower indices of PT and LPT with LBW in 1982 when compared with the other cohorts, except for LPT with LBP in 2004. In 2011, single mothers had higher rates of PT and LPT alone or with LBW (Table 1).
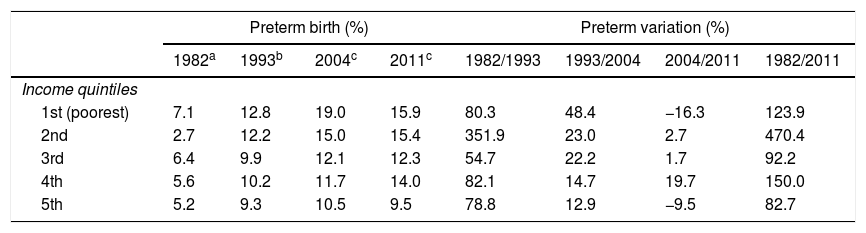
The highest prevalence of PT was observed among the poorest families (first quintile), in all four studies analyzed. The largest increase in prematurity occurred between 1982 and 1993 cohorts, especially among poor mothers (income quintile 2) (351.9%) and rich mothers (income quintile 4; 82.1%). The largest reduction occurred between 2004 and 2011 among the poorest mothers (Q1; – 16.3%), followed by the richest mothers (Q5; – 9.5%; Table 2).
Prevalence of preterm birth and the preterm percentage variation according to family income quintiles among four birth cohort studies.
| Preterm birth (%) | Preterm variation (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| 1982a | 1993b | 2004c | 2011c | 1982/1993 | 1993/2004 | 2004/2011 | 1982/2011 | |
| Income quintiles | ||||||||
| 1st (poorest) | 7.1 | 12.8 | 19.0 | 15.9 | 80.3 | 48.4 | −16.3 | 123.9 |
| 2nd | 2.7 | 12.2 | 15.0 | 15.4 | 351.9 | 23.0 | 2.7 | 470.4 |
| 3rd | 6.4 | 9.9 | 12.1 | 12.3 | 54.7 | 22.2 | 1.7 | 92.2 |
| 4th | 5.6 | 10.2 | 11.7 | 14.0 | 82.1 | 14.7 | 19.7 | 150.0 |
| 5th | 5.2 | 9.3 | 10.5 | 9.5 | 78.8 | 12.9 | −9.5 | 82.7 |
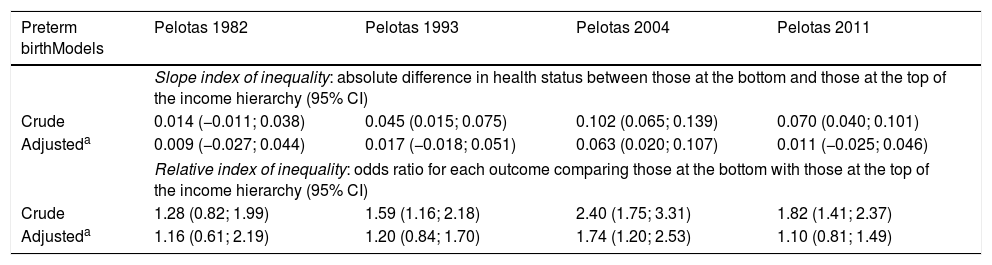
Inequalities in PT were observed through crude and adjusted SII analysis. The largest SII income inequality relating to PT was observed in 2004, with the difference between the poorest (Q1) and the richest (Q5) of 6.3 PP. Those differences were not observed in 1982, 1993, or 2011 as confidential intervals (CI) that included zero (Table 3).
Crude and adjusted analysis on the association of family income with preterm birth among four birth cohort studies.
| Preterm birthModels | Pelotas 1982 | Pelotas 1993 | Pelotas 2004 | Pelotas 2011 |
|---|---|---|---|---|
| Slope index of inequality: absolute difference in health status between those at the bottom and those at the top of the income hierarchy (95% CI) | ||||
| Crude | 0.014 (−0.011; 0.038) | 0.045 (0.015; 0.075) | 0.102 (0.065; 0.139) | 0.070 (0.040; 0.101) |
| Adjusteda | 0.009 (−0.027; 0.044) | 0.017 (−0.018; 0.051) | 0.063 (0.020; 0.107) | 0.011 (−0.025; 0.046) |
| Relative index of inequality: odds ratio for each outcome comparing those at the bottom with those at the top of the income hierarchy (95% CI) | ||||
| Crude | 1.28 (0.82; 1.99) | 1.59 (1.16; 2.18) | 2.40 (1.75; 3.31) | 1.82 (1.41; 2.37) |
| Adjusteda | 1.16 (0.61; 2.19) | 1.20 (0.84; 1.70) | 1.74 (1.20; 2.53) | 1.10 (0.81; 1.49) |
For RII, it was observed that in the 1993, 2004, and 2011 cohorts, the poorest mothers had a higher chance of having PT when compared with the richest. The adjustment for confounding factors reduced the odds ratio (OR), and in 2004, only the poorest mothers had a greater chance of PT (Table 3).
There was a bottom pattern of inequality in 2004 and a top pattern in 2011, unlike the linear pattern shown in 1982 and 1993. There was an increase in occurrence of PT up to 2004 and a slight reduction in 2011, mainly in the poorest population (Fig. 1).
DiscussionThese four studies with great volume of information, gathered from birth cohorts from the same Brazilian city, allowed the comparison of socioeconomic aspects in order to assess PT inequalities. Socioeconomic inequality according to income was demonstrated in all studies, but after adjustment, a significant OR was shown only for the 2004 cohort. An increased prevalence of PT was observed, especially among poorer mothers.
Health inequality occurred by differences between the most privileged groups in a chosen category of social determinants of health.15 The most important determinant factors related to inequality are ethnicity, religion, socioeconomic position (wealth, income, schooling, or occupation), marital status, and age.8,15 Worldwide, mothers and fetuses are exposed to many factors of iniquity, leading to undesirable neonatal outcomes.4,16
Greater differences related to major occurrence of PT were seen in mothers of black ethnicity, low education, singles, aged <20 or ≥35 in the 1993, 2004, and 2011 studies; in 1993 and 2004, it more evident in black mothers and in those with <4 years of schooling. These differences were also found in other countries, associated to ethnicity,5,17,18 education,19–21 income,22 or all.23
Income is one of the risk factors that determine the individual's social position; low income may be a related to social exclusion of individuals in their communities, being therefore related to marked health inequalities.16 Additionally, it may determine changes in maternal and child health, affecting neonatal and childhood morbidities, with a reflex in the child's future development. The influence of income on maternal and child health may be due to difficulties prior to pregnancy, such as access to good quality/quantity of food, provision of appropriate prenatal care, and early identification of morbidities.3
Analysis on the different income statements showed that the 2004 cohort presented almost twice the occurrence of PT among the poorest mothers. This result was observed, to a lesser degree, in the 2011 cohort, but without effect in RII or SII. The higher levels of PT that occurred among the poorest mothers in the 1982, 1993, and 2004 studies were also observed among the richest mothers (although less intensely). A significant decrease was observed in 2011 among the poorest mothers and lower among the richest. Despite the stabilization of the proportion of PT in 2011, the rates were still higher among the poorest mothers.
It is important to note that LPT accounted for the largest proportion of PT, and it occurrences were inversely related to those of PT. As there was no confirmation of GA through the most accurate measurement (first-trimester ultrasound) until 2004, erroneous calculation of GA could have occurred, therefore explaining the LPT behavior.2,24 Small changes in the occurrence of PT with LBW were observed across the studies, very similar for prematurity alone, but including LPT associated with LBW just in the studies of 2004 and 2011.
PT is more prevalent in medium/low-income countries, but its survival rate is much higher in high-income countries.1,2 In 2011, the PT rate reported in Brazil ranged from 9.3% to 10.5% of total births.25 Silveira et al. pointed out that there were major differences in PT prevalence according to the Brazilian region studied. The highest rates were observed in the south and southeast regions (3.4–15.0%, from 1978 to 2004), whereas the lowest were in the northeast region (3.8–10.2%, from 1984 to 1998). In all regions, there is a tendency toward gradual increases. Reports from different Brazilian cities indicate that the total percentage of PT in Brazil may have been underestimated.26 A national multicenter study including 191 cities found a PT rate of 12.5% and discussed the importance of erroneous classifications of LPT as term births, and the large number of surgical interventions as possible avoidable causes of this outcome.27
Improvements in income, education, and type of work can influence health inequalities, with an impact on individual and community health.6 Previous publication using data from the same cohorts demonstrated a significant economic inequality related to family income for small to gestational age (SGA) and LBW newborns and suggest that improvements in Brazilian economy may have modified the prevalence of these outcomes in all cohorts.28
These socioeconomic changes could also have helped in the reduction of PT. However, others factors influenced PT rates, such as mode of delivery. The vast majority of PT happens spontaneously. Other cultural factors, early induction of labor, and inappropriate indication of C-sections may increase the prevalence of PT, regardless of the mother's socioeconomic position.3,4,16 Unfortunately, among people who are less favored economically, there is difficulty in accessing prenatal care, worsening the real prevalence of prematurity in this group. This difficulty is compounded by the low accuracy of using the LMP or Dubowitz methods13 instead of early obstetric US (gold standard for GA calculation).3
The increased prevalence of PT and, in the vast majority of LPT, can be explained (in part) to alarming and increasing rates of C-sections in Brazil, with a greater proportion among private healthcare users.25 An analysis on the indications for surgical intervention indicated that 35% of deliveries were elective. In addition, the socioeconomically privileged social classes may have improper conceptions of normal delivery as a cause of “pain and suffering.”29 Moreover, cultural factors and other questionable causes of C-section indication attributed by healthcare professionals are associated with indications of non-natural childbirth.29
Improvements in the survival of PT newborns, due to advances in neonatology and better access to specialized care, especially for very premature infants, have culminated in reductions of newborn and child mortality.3 However, the scale of the reductions of these indexes continues to be smaller than expected. There is a serious concern regarding LPT, which could lead to a greater likelihood not only of child morbidity and mortality, but also of higher mortality among young adults. Furthermore, the morbidities and sequelae of PT are serious consequences imposed on socioeconomically underprivileged families.2,3,30
One of possible limitations of the present study is the fact that it did not compare delivery modes or other data related to previous maternal health and/or pregnancies, such as BMI, previous history of prematurity, or maternal habits such as nutrition or consumption of illicit or licit drugs (alcohol and tobacco). These factors could have an influence in the inadequate neonatal outcomes, such as PT or even infant and child morbimortality. Furthermore, lack of exploration of other dimensions of inequality, such as schooling and ethnicity as the primary outcome, were one of the limitations of this study.
Other limitations may occur, as methods to determine GA have changed over time. The use of combined methods could increase accuracy to determine the real prevalence of PT, especially by using US in the first and second trimesters (≤23 weeks), as observed in the last cohorts (2004 and 2011). However, with exception of 1982, all studies presented PT prevalence with minor variation, and the statistics were performed using the same distribution of income quintiles, minimizing changes in the result of the inequality indices. These facts reinforce the result of this paper, despite a suspected discrepancy of GA.
PT was related with inequalities of income until 2004, with a reduction in 2011, although the rate remained higher among poorer mothers in all the studies. These results highlight the importance of public health policies, social inclusion, and promotion of improved income and education levels among families with socioeconomic vulnerability, as part of the efforts to promote healthy newborn outcomes and to reduce preterm birth.
Funding- -
Brazilian Government Agency for Qualification of Human Resources (CAPES);
- -
Brazilian Public Health Association (ABRASCO);
- -
Wellcome Trust;
- -
The International Development Research Center;
- -
World Health Organization;
- -
Overseas Development Administration;
- -
European Union;
- -
National Support Program for Centers of Excellence (PRONEX);
- -
Brazilian National Research Council (CNPq);
- -
Brazilian Ministry of Health;
- -
Children's Pastorate;
- -
Bill & Melinda Gates Foundation.
The authors declare no conflicts of interest.
Please cite this article as: Sadovsky AD, Matijasevich A, Santos IS, Barros FC, Miranda AE, Silveira MF. Socioeconomic inequality in preterm birth in four Brazilian birth cohort studies. J Pediatr (Rio J). 2018;94:15–22.