to identify possible risk factors associated with wheezing in infants (12-15 months-old) in the state of Mato Grosso, Brazil.
Methodsthis was a cross-sectional study performed by applying a standardized written questionnaire from the international study on wheezing in infants (Estudio Internacional de Sibilancia en Lactantes - EISL), phase 3. Parents and/or guardians of infants were interviewed at primary health care clinics or at home from August of 2009 to November of 2010. Factors associated to wheezing were studied using bivariate and multivariate analysis (using the Statistical Package for Social Sciences [SPSS] v.18.0), and expressed as odds ratios (OR) and 95% confidence intervals (95% CI).
Resultsthe written questionnaire was answered by 1,060 parents and/or guardians. The risk factors for wheezing were: history of asthma in the family [mother (OR = 1.62; 95% CI = 1.07-2.43); father (OR = 1.98; 95% CI = 1.22-3.23); siblings (OR = 2.13; 95% CI = 1.18-3.87)]; history of previous pneumonia (OR = 10.80; 95% CI = 4.52-25.77); having had more than six upper respiratory tract infections (URTIs) (OR = 2.95; 95% CI = 2.11-4.14); having had first URTI before the third month of life (OR = 1.50; 95% CI = 1.04-2.17); living in a moderately polluted area (OR = 1.59; 95% CI = 1.08-2.33); paracetamol use for URTI (OR = 2.13; 95% CI = 1.54-2.95); and antibiotic use for skin infection (OR = 2.29; 95% CI = 1.18-4.46).
Conclusionsthe study of risk factors for wheezing in the first year of life is important to help physicians identify young children at high risk of developing asthma and to improve public health prevention strategies in order to reduce the morbidity of wheezing in childhood.
identificar possíveis fatores de risco associados à sibilância em lactentes (12 a 15 meses) no estado de Mato Grosso, Brasil.
Métodosestudo transversal, utilizando o questionário escrito padronizado do Estudio Internacional de Sibilancia en Lactantes (EISL) – fase 3. Pais e/ou responsáveis pela criança foram entrevistados em Unidades Básicas de Saúde quando as procuravam para imunização de rotina ou durante visitas nos domicílios de crianças matriculadas nos programas de saúde da família, no período de agosto de 2009 a novembro de 2010. Fatores associados à sibilância foram avaliados utilizando análise bivariada e multivariada e expressos como odds ratio (OR) e intervalo de confiança 95% (IC95%).
Resultadosao todo, um mil e sessenta (n = 1.060) pais e/ou responsáveis responderam o questionário escrito. Os fatores de risco para sibilância foram: história familiar de asma [mãe (OR = 1,62; IC95%= 1,07-2,43); pai (OR = 1,98; IC95% = 1,22-3,23); irmãos (OR = 2,13; IC95% = 1,18-3,87)]; história prévia de pneumonia (OR = 10,8; IC 95% = 4,52-25,77); ter mais de seis infecções de vias aéreas superiores (IVAS) (OR = 2,95; IC95% = 2,11-4,14) e a primeira IVAS antes dos três meses de idade (OR = 1,50; IC95% = 1,04-2,17); residir em local com moderada poluição (OR = 1,59; IC95% = 1,08-2,33); uso de paracetamol por IVAS (OR = 2,13; IC95% = 1,54-2,95); e uso de antibiótico por infecção na pele (OR = 2,29; IC 95% = 1,18-4,46).
ConclusõesO estudo dos fatores de risco para sibilância no primeiro ano de vida é importante para auxiliar na identificação, entre os lactentes sibilantes, aqueles de alto risco para desenvolver asma, e para o desenvolvimento de estratégias de prevenção por políticas pública de saúde visando minimizar a morbidade da sibilância na infância.
Wheezing in infants is an important cause of morbidity worldwide, both in developed and developing countries.1 Some wheezing phenotypes have been described as associated with different risk factors.2 In infants and preschool children, the asthma diagnosis is based on clinical symptoms, presence of risk factors, and therapeutic response; therefore, the identification, among wheezing infants, of those at high risk for developing asthma is crucial to define which children will benefit from preventive or therapeutic interventions.3
Prospective studies suggest several risk factors for early wheezing in children and its association with the subsequent development of asthma, such as family history of allergy,4 personal history of rhinitis or eczema,5,6 maternal smoking during pregnancy or passive exposure after birth,7 male gender,2,5 viral respiratory infections by respiratory syncytial virus (RSV) or rhinovirus,8,9 and attending daycare.10 Epidemiological studies have observed an association between the development of asthma and regular use of medications such as paracetamol and antibiotics during infancy.11,12
Therefore, risk factors for wheezing in infants have been identified, but their analysis is complex, due to the genetic-environmental interactions. The development of methods to identify and quantify these factors is essential for better understanding the natural history of asthma in childhood. The epidemiology of asthma is known worldwide in school-age children, adolescents, and adults; however, the prevalence and risk factors associated with symptoms of recurrent wheezing in infants and preschool children are still under investigation.13
To assess the impact of recurrent wheezing in infants and determine its prevalence and associated risk factors, the International Study of Wheezing in Infants in the first year of life (Estudio Internacional de Sibilancias en Lactantes - EISL) was developed. This is an international multicenter study with the participation of Latin American countries, Spain, and the Netherlands, whose tool was a standardized questionnaire validated in all participating centers. Phase 1 of EISL used a standardized questionnaire with 45 questions on demographic characteristics, respiratory symptoms, use of medications, and possible risk factors associated with wheezing.1 Phase 2 was designed to verify the onset and persistence of wheezing in preschoolers among the children who participated in Phase 1, and the centers that participated have not yet published their results. Phase 3 was designed to be conducted five years after Phase 1 in the same region, to compare the trend in prevalence in relation to Phase 1 data, and it used the same questionnaire as in Phase 1, including five questions on the use of antibiotics and paracetamol in first months of life, totaling 50 questions.
This study aimed to evaluate risk factors associated with wheezing in infants in Midwestern Brazil, using the standardized protocol of EISL - Phase 3.
Patients and methodsParents or guardians of healthy infants aged 12 to 15 months who answered the standard written questionnaire of EISL (QE-EISL) - Phase 3 participated in the study.
Among the 60 basic health units (BHUs) distributed in four regions - North, South, East and West - of the city, 28 were randomly selected for the study. Parents and/or guardians were invited to participate when they came for consultation and routine immunization of their children, or during visits to households of all children aged 12 to 15 months enrolled in the Family Health Program of the BHUs. All parents and/or guardians agreed to participate, signed an informed consent, and were then interviewed by the main investigator or a previously trained medical student. Visits to the BHUs or homes occurred between August of 2009 and November of 2010; during the two immunization campaigns against polio performed during this period, all children who belonged to the target age group that came on the day of the campaign participated in the study.
The QE-EISL - phase 3 is a tool consisting of 50 questions regarding demographic characteristics, wheezing, and risk factors, translated into Portuguese and validated for the Brazilian population.14
To perform the study, the coordinators of the EISL stipulated that the sample should include at least 1,000 infants. The sample size was based on the International Study of Asthma and Allergies in Childhood (ISAAC), considering a prevalence of wheezing of 30% and 25% in two different centers, with a study power of 95% and a significance level of 1% for this sample, to ensure adequate power for comparisons between centers and countries, even for questions with a low prevalence of positive answers.1,15
Infants who had three or more episodes of wheezing were deemed recurrent wheezers and those with less than three episodes of wheezing were termed occasional wheezers. Those who never had a wheezing episode were classified as non-wheezers.
Data were coded in a standard way, transferred to a database developed in Microsoft Excel® 2007, and statistically analyzed using the Statistical Package for Social Sciences (SPSS) for Windows - release 18.0.
Non-parametric tests were used (chi-squared and Fisher's exact test), as well as logistic regression model. Estimates of prevalence ratio with a 95% confidence interval (95% CI) were calculated in the bivariate analysis. The Poisson model was used for the logistic regression to evaluate the factors associated with the presence or absence of wheezing. In the initial model, the variables that resulted in a p < 0.20 in the bivariate analysis were identified. For multivariate analysis, the backward technique was used and the test for variable input and output was the likelihood ratio, with p < 0.05, thus determining the final model. All significance probabilities were bilateral, with a significance level of 0.05 in all tests.
This study was approved by the Ethics Committee of the Universidade Federal de São Paulo/Escola Paulista de Medicina (UNIFESP/EPM) and the Research Ethics Committee of the Hospital Universitário Júlio Müller.
ResultsA total of 1,060 parents and/or guardians of infants aged between 12 and 15 months were interviewed. No questionnaires were excluded from the sample due to incorrect completion. Most responders were mothers (87.9%), followed by other relatives (6.4%), and fathers (5.7%). Five hundred and forty-six (51.5%) were females and 514 (48.5%) were males. Two hundred and ninety-four (27.7%) infants had at least one episode of wheezing in the first year of life (“wheezers”), with wheezing onset at 5.8±3.0 months. Among the wheezing infants, 159 (54.1%) had less than three episodes (occasional wheezing) and 135 (45.9%) had three or more episodes (recurrent wheezing).
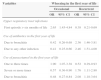
Table 1 shows the factors that were associated with wheezing in the first 12 months of life in the bivariate analysis, which were: male gender, history of pneumonia and hospitalization for pneumonia, exposure to maternal smoking during pregnancy and passive exposure after birth, family history of asthma, daily consumption of industrialized foods, breastfeeding duration between two and four months, more than six upper respiratory tract infections (URTIs), having the first URTI before three months of life, living in a moderately polluted environment, presence of at least one sibling in the household, household income less than R$ 800.00, use of antibiotics for pneumonia and skin infections, and use of paracetamol for URTI.
Factors associated with the presence of at least one episode of wheezing in the first 12 months of life (n = 294) in the bivariate analysis.
| Factors | n | PR | 95% CI | p |
|---|---|---|---|---|
| Male gender | 159 | 1.36 | 1.04-1.79 | 0.029 |
| Pneumonia | 80 | 3.90 | 2.72-5.58 | 0.000 |
| Hospitalization due to pneumonia | 33 | 3.91 | 2.27-6.73 | 0.000 |
| Passive smoking | 94 | 1.58 | 1.17-2.12 | 0.003 |
| Maternal smoking during pregnancy | 16 | 2.15 | 1.10-4.20 | 0.023 |
| Asthma in the family | ||||
| Father | 37 | 1.79 | 1.16-2.77 | 0.012 |
| Mother | 57 | 1.58 | 1.11-2.26 | 0.015 |
| Sibling | 26 | 2.15 | 1.26-3.67 | 0.006 |
| Daily intake of industrialized food | 139 | 1.42 | 1.09-1.87 | 0.013 |
| URTIs | ||||
| ≥ six episodes a year | 125 | 3.90 | 2.89-5.28 | 0.000 |
| First episode before three months of life | 86 | 2.06 | 1.50-2.82 | 0.000 |
| First episode after six months of life | 64 | 0.53 | 0.39-0.72 | 0.000 |
| C-section delivery | 212 | 0.44 | 0.30-0.57 | 0.000 |
| Mother's level of schooling: complete high school or college/university | 94 | 0.66 | 0.50-0.88 | 0.005 |
| Air conditioning at home | 135 | 0.46 | 0.35-0.60 | 0.000 |
| Indoor bathroom | 262 | 0.26 | 0.15-0.46 | 0.000 |
| Live in a moderately polluted environment | 68 | 1.79 | 1.28-2.52 | 0.001 |
| Have at least one sibling | 180 | 1.50 | 1.14-1.97 | 0.005 |
| Mother has a job | 138 | 0.63 | 0.48-0.83 | 0.001 |
| Family income < R$ 800.00 | 71 | 2.25 | 1.60-3.17 | 0.000 |
| Family income of R$ 3,500.00 to R$ 5,000.00 | 43 | 0.60 | 0.42-0.87 | 0.008 |
| Updated immunizations | 266 | 0.47 | 0.28-0.78 | 0.005 |
| Antibiotic use | ||||
| Due to pneumonia | 53 | 2.63 | 1.77-3.93 | 0.000 |
| Due to otitis | 49 | 1.76 | 1.20-2.56 | 0.004 |
| Due to skin infection | 22 | 2.40 | 1.33-4.32 | 0.004 |
| Paracetamol use | ||||
| Due to URTIs | 211 | 2.62 | 1.96-3.51 | 0.000 |
| Due to pneumonia | 22 | 4.68 | 2.33-9.43 | 0.000 |
| Number of times that paracetamol was used | ||||
| One to three times | 65 | 0.64 | 0.47-0.88 | 0.006 |
| Seven or more times | 141 | 1.75 | 1.33-2.30 | 0.000 |
CI, confidence interval; PR, prevalence ratio; URTIs, upper respiratory tract infections.
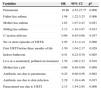
Factors associated with recurrent wheezing in the bivariate analysis were: antibiotics for bronchitis, antibiotics for any infection, use of paracetamol for bronchitis, and paracetamol use more than seven times in the first year of life (Table 2).
Factors associated with occasional (less than three episodes of wheezing, n=159) and recurrent wheezing (three or more episodes of wheezing, n=135) in the first year of life in the bivariate analysis.
| Variables | Wheezing in the first year of life | |||
|---|---|---|---|---|
| Occasional | Recurrent | |||
| OR | 95% CI | OR | 95% CI | |
| Upper respiratory tract infections | ||||
| First episode > six months of life | 2.65 | 1.45-4.84 | 0.38 | 0.21-0.69 |
| Use of antibiotics in the first year of life | ||||
| Due to bronchitis | 0.42 | 0.26-0.68 | 2.36 | 1.46-3.81 |
| Due to any other infection | 0.41 | 0.25-0.66 | 2.46 | 1.51-4.00 |
| Use of paracetamol in the first year of life | ||||
| One to three times | 1.90 | 1.07-3.38 | 0.52 | 0.29-0.93 |
| Seven or more times | 0.57 | 0.36-0.90 | 1.76 | 1.11-2.80 |
| Due to bronchitis | 0.48 | 0.27-0.84 | 2.08 | 1.18-3.64 |
CI, confidence interval; OR, odds ratio.
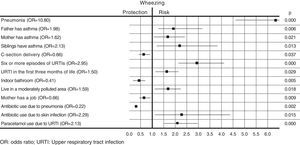
Table 3 and Fig. 1 show the results of the multivariate analysis. Odds ratios (OR) and corresponding 95% confidence intervals (95%CI) were calculated. Independent risk factors associated with the presence of at least one episode of wheezing in the first year of life were: history of pneumonia, family history of asthma in the mother, father and siblings, more than six URTIs, first URTI before three months of life, living in a moderately polluted environment, antibiotic use for skin infections, and paracetamol use for URTIs. The protective factors for wheezing in the first year of life were: C-section delivery, indoor bathroom, mother having paid work, and taking antibiotics for pneumonia.
Factors associated with wheezing in the first year of life in the multivariate analysis (n=294).
| Variables | OR | 95% CI | pa |
|---|---|---|---|
| Pneumonia | 10.80 | 4.52-27.77 | 0.000 |
| Father has asthma | 1.98 | 1.22-3.23 | 0.006 |
| Mother has asthma | 1.62 | 1.07-2.43 | 0.021 |
| Sibling has asthma | 2.13 | 1.18-3.87 | 0.013 |
| C-section delivery | 0.66 | 0.45-0.98 | 0.037 |
| Six or more episodes of URTIs | 2.95 | 2.11-4.14 | 0.000 |
| First URTI before three months of life | 1.50 | 1.04-2.17 | 0.029 |
| Indoor bathroom | 0.41 | 0.22-0.76 | 0.005 |
| Live in a moderately polluted environment | 1.59 | 1.08-2.33 | 0.018 |
| Mother has a job | 0.66 | 0.48-0.90 | 0.009 |
| Antibiotic use due to pneumonia | 0.22 | 0.08-0.56 | 0.002 |
| Antibiotic use due to skin infection | 2.29 | 1.18-4.46 | 0.015 |
| Paracetamol use due to URTI | 2.13 | 1.54-2.95 | 0.000 |
CI, confidence interval; OR, odds ratio; URTIs, upper respiratory tract infections.
Genetic and environmental factors have been suggested as risk factors for wheezing in the first years of life. As wheezing is the main symptom of asthma, identifying these factors in this age group is crucial for a better understanding of the different wheezing phenotypes and the progression to asthma development. The results of this study point to several genetic, demographic, and environmental factors associated with wheezing in the first year of life.
Among the sociodemographic factors, male gender was a risk factor for the occurrence of at least one episode of wheezing in infants evaluated in the bivariate analysis (Table 1). Other Brazilian studies also found this association.16,17 This factor, however, did not remain a risk factor in the multivariate analysis; a similar finding was observed in another Brazilian study.18
In this study, the presence of asthma in the infants’ relatives (mother, father, and siblings) was associated with risk of wheezing in the first year of life in both the bivariate and multivariate analyses. In a Brazilian cohort study, family history of asthma assessed at four years of age was significantly associated with the pattern of transient and persistent wheezing.5 Other studies have found this association16–18, in agreement with the Asthma Predictive Index (API), which has parental history of asthma as a major criterion for the diagnosis of asthma in children with recurrent wheezing.19
The presence of six or more episodes of upper respiratory tract infections in the first year of life, with early onset (before three months of age), was a factor associated with wheezing in this study (Tables 1 and 3). The presence of at least one sibling in the house, which was also associated with wheezing in the bivariate analysis, may partly explain the early occurrence of these infections, as only 31 (10.5%) of the infants who had at least one episode of wheezing attended daycare (data not shown).
Upper and lower airway infections, particularly those caused by RSV and rhinoviruses, are common triggers of wheezing in childhood, but the role of early infection in the subsequent development of asthma is less clear.20 The EISL - Phase 1, which involved 28,687 infants from countries in Latin America and Europe, observed the presence of URTI in the first three months of life among the risk factors for occasional and recurrent wheezing.1 A cohort study that evaluated 2,319 infants up to two years of age found that children who had common colds in the first three months of life had high risk for experiencing wheezing in the second year of life.21 Another study found that the number of respiratory infections, particularly in the first two years of life, showed an almost linear association with the risk of subsequent asthma, and that the group of children who had nine to ten infections had an almost eight-fold higher risk for development of asthma.22
The reporting of pneumonia was associated with wheezing in both the bivariate and multivariate analyses (Tables 1 and 3). As this was a cross-sectional study, wheezing could not be characterized as a triggering or consequent factor of pulmonary infections, but pneumonia was an important risk factor in this study. In a cohort of newborns of low socioeconomic class in Santiago (Chile), followed during the first year of life, a prevalence of pneumonia of 13.3%, was observed, and the presence of recurrent wheezing during the first three months of life was strongly associated with the diagnosis of pneumonia.23 EISL publications in Brazil also found the presence of pneumonia in the first year of life as a risk factor associated with wheezing.17,18,24
In the present study, exposure to maternal smoking during pregnancy and passive exposure after birth was associated with wheezing only in the bivariate analysis (Table 1). The multivariate analysis did not confirm this association, which can be explained by the low frequency of mothers of wheezing infants who smoked during pregnancy (5.4%) or after birth (7.5%). There is a tendency towards undernotification of the frequency of smoking by parents and caregivers of children with respiratory diseases, as they know the harmful effects of smoking on the respiratory system.
Obtaining objective measures of this exposure could minimize this bias. Exposure to cigarette smoke, both in the prenatal period and after birth, was associated with the risk of wheezing in infants and preschool children in several studies.1,17,25 A meta-analysis observed that prenatal or postnatal exposure increased the risk of incidence of wheezing by 30% to 70%, mainly in children younger than two years, stressing that parental smoking prevention is crucial for asthma prevention.7
The present study demonstrated that living in a moderately polluted environment was a risk factor for wheezing in the first year of life, similar to that observed in other studies.18,26 Exposure to pollutants may be associated with respiratory symptoms such as wheezing, not only as a triggering factor, but also as a risk factor for the development of asthma, according to the results of a cohort study of 4,089 Swedish children, which demonstrated that exposure to air pollution from traffic during the first year of life was associated with risk of persistent wheezing and low lung function at the age of 4 years.27 In a Chilean cohort study, the prevalence of wheezing in the first year of life was high (80.3%), and it was observed that 82.2% of the children were exposed to pollutants resulting from the fuel used for heating or cooking (kerosene, gas), and that 38.5% of the homes were located on unpaved roads.23 As the pollution exposure was known only through parental report, this result must be analyzed with caution, as it lacks objective measures to assess the degree of intra- and extra-domiciliary environment pollution.
In this study, the use of drugs such as paracetamol and antibiotics was associated with the risk of recurrent wheezing (Table 2) and of wheezing in the first year of life (Table 3).
A prospective study that followed children with a family history of atopy, from birth to 7 years of age, found an association between frequency of paracetamol use and asthma development, which was not maintained after adjustment for the frequency of respiratory infections, suggesting a confounding factor i.e., it is likely that the viral infections in early childhood, more than the use of paracetamol, may lead to the development of asthma.28 However, in another study, the association between asthma and paracetamol use persisted even after adjusting for respiratory infections.29 A cohort study that evaluated the use of paracetamol during pregnancy observed that the use of this drug was associated with the presence of asthma at age five and the risk was higher in those who had a greater number of days of consumption, suggesting a possible dose-dependent association.30
Therefore, the association between paracetamol and wheezing/asthma may simply reflect a reverse causality, i.e. children with a genetic predisposition to asthma or other allergies are more prone to febrile comorbidities, particularly URTI and therefore use more antipyretic medications such as acetaminophen.11 Thus, the association between paracetamol and wheezing/asthma requires further studies, using more appropriate designs that can attenuate or eliminate potential confounding biases.
The use of antibiotics was a risk factor for wheezing, and this can be explained in part by the “hygiene hypothesis”, which suggests that children who grow up in an environment with less microbial exposure tend to be more atopic and therefore have a greater chance of developing asthma.31 A meta-analysis study observed that exposure to at least one course of antibiotics in the first year of life was a risk factor for the development of asthma in childhood.32 A cohort study of 251,817 Canadian children followed from birth, evaluated for exposure to antibiotics in the first year of life, observed a lower risk for developing asthma, but this risk increased greatly when the child received more than four courses of antibiotics in the study period.33 Another recent meta-analysis evaluating antibiotic exposure in the prenatal period and the first year of life found an association with asthma from ages 3 to 18 years.34
In fact, several studies show a significant association between the use of antibiotics in early childhood and subsequent development of wheezing/asthma; conversely, the use of antibiotics may be a consequence of the increased frequency of respiratory infections in children with allergic predisposition, which is postulated as reverse causality, and this may complicate the interpretation of several epidemiological studies; therefore, further studies are needed to elucidate this association.
The present study had some limitations that should be considered when interpreting the results. As this was a cross-sectional study, the associations observed cannot be considered as causalities, and prospective studies are necessary to better clarify the correlation between risk factors for wheezing and/or asthma. A strong aspect of the study was that the information regarding the wheezing that occurred in the first 12 months of life was obtained when the infants were 12 to 15 months, thereby decreasing the likelihood of recall bias. Other important aspects of this study were the sample size and the use of a standardized questionnaire that allowed for the comparison between the different centers which performed the study.
In conclusion, this study demonstrated that some factors were associated with risk of wheezing in the first year of life, such as family history of asthma, pneumonia, more than six episodes of upper respiratory infections in early life, living in a polluted environment, and use of paracetamol and antibiotics. These factors varied when compared with other Brazilian studies that used the same protocol, which reinforces the need for further studies in other cities of Brazil due to the environmental particularities of each region. Prospective follow-ups of wheezing infants are needed to analyze the impact of these risk factors over the long-term in Brazil. The identification of risk factors for wheezing in the first years of life is crucial not only for the diagnosis of asthma, but also for the development of prevention strategies through public health policies aiming to minimize wheezing morbidity in childhood.
FundingFundação de Amparo à Pesquisa do Estado de Mato Grosso (FAPEMAT), Process No. 004/2009- 447941/2009.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Fundação de Amparo à Pesquisa do Estado de Mato Grosso (FAPEMAT) for the financial support (Process No. 447941/2009) and the Municipal Health Secretariat of Cuiabá (MT) for the authorization for the use of the public health services for the performance of this study.
Please cite this article as: Moraes LS, Takano OA, Mallol J, Solé D. Risk factors associated with wheezing in infants. J Pediatr (Rio J). 2013;89:559–566.