ultrasound (US) has been an important diagnostic tool to identify several causes of gastrointestinal bleeding. Infants with cow's milk allergy (CMA) may present hematochezia and the confirmation of the diagnosis can be difficult. The aim of this study is to describe grayscale and color Doppler ultrasound findings in patients with CMA.
Methodswe retrospectively studied 13 infants with CMA. All infants presented severe hematochezia and abdominal pain. All underwent an US study with the diagnosis of allergic colitis. This diagnosis was based on clinical findings, recovery after infant or mother exclusion diets in the case of exclusive breastfeeding and positive oral challenge test.
Resultsthe mean age ranged from 1 to 6 months (mean=3.53). Seven out of 13 infants (53.8%) had grayscale and color Doppler sonographic repeated after exclusion diet. Twelve out of 13 (92,3%) showed abnormalities at US and CDUS at beginning. The positive findings suggesting colitis were thickened bowel walls and increased vascularity, especially in the descending and sigmoid colon. Colonoscopy and histopathological findings were compatible with allergic colitis. After a diet change the 13 infants recovered and their oral challenge tests were positive.
ConclusionDoppler US may be very useful in diagnosing secondary colitis, such as CMA, and to exclude several other abdominal diseases that can emulate this disease.
O ultrassom (US) tem sido uma importante ferramenta de diagnóstico para identificar várias causas de hemorragia gastrointestinal. Neonatos com alergia ao leite de vaca (ALV) podem apresentar hematoquezia, e a confirmação do diagnóstico pode ser difícil. O objetivo deste estudo é descrever achados com ultrassom em escala de cinza e com Doppler colorido em pacientes com ALV.
MétodosEstudamos, retrospectivamente, 13 neonatos com ALV. Todos eles apresentaram hematoquezia severa e dor abdominal e foram submetidos a um estudo com US, com o diagnóstico de colite alérgica. O diagnóstico teve como base os achados clínicos, a recuperação após a dieta de exclusão do neonato ou da mãe, no caso de amamentação exclusiva, e o teste de provocação oral positivo.
ResultadosA idade média variou de um a seis meses (média=3,53). Sete dos 13 neonatos (53,8%) passaram novamente por ultrassonografia em escala de cinza e com Doppler colorido após a dieta de exclusão. Dentre eles, 12 dos 13 (92,3%) mostraram anormalidades no US e no ultrassom com Doppler colorido (USDC) no início. Os achados positivos que sugeriram colite foram paredes intestinais espessas e aumento na vascularização, principalmente no cólon descendente e sigmoide. Os resultados da colonoscopia e histopatológicos foram compatíveis com colite alérgica. Após uma mudança na dieta, os 13 neonatos se recuperaram e seus testes de provocação oral foram positivos.
ConclusãoO US com Doppler pode ser muito útil para diagnosticar a colite secundária, como a ALV, e para excluir várias outras doenças abdominais que podem imitar essa doença.
Allergic proctocolitis is the main cause of rectal bleeding in infants during the first six months of life. Generally it occurs due to early exposure to heterologous proteins, especially from cow's milk intake or cow's milk proteins derived from maternal breastfeeding. This allergy is usually cell mediated and is due to an immunological immaturity of the infant gut. Generally, allergic proctocolitis is a transient process, which ceases during the first year of life in more than half of cases.1,2
The clinical presentation of allergic proctocolitis is variable but often includes hematochezia (bright red blood in the stool), diarrhea, vomiting, irritability, cramps, abdominal distention, and growth impairment.3,4 Regardless of the clinical presentation, the cow's milk allergy (CMA) diagnosis is made through response to exclusion diet and subsequent oral challenge.5–7
Food allergy colitis is frequently overlooked due to the wide range of symptoms and its insidious nature, which makes it difficult to establish a definitive diagnosis.6 Grayscale ultrasound (US) and color Doppler ultrasound (CDUS) have been important diagnostic tools to identify different causes of gastrointestinal bleeding, such as complications caused by Meckel's diverticulum, midgut volvulus, infectious colitis, intussusception, vascular malformations, and inflammation.8,9 US and CDUS have also been employed to detect inflammatory bowel disease in children.10–12 and less frequently in allergic colitis.13
Recently, using CDUS, we assessed the mesenteric circulation of infants below the age of 6 months with suspected CMA.12 The group of children involved in this study were heterogeneous, including infants with different clinical manifestations besides allergic proctocolitis, as colic, vomiting. Controls were asymptomatic infants <6 months.12 When comparing both groups there was a significant increase of the mesenteric vessel density in infants with confirmed CMA diagnoses (by the exclusion diet for four weeks and challenge test) when compared to controls and patients with non-confirmed CMA. Those results suggest that CDUS could be used as a screening tool to diagnose CMA.
The aim of this study is to describe grayscale and color Doppler ultrasound findings in infants with hematochezia due to allergic proctocolitis.
MethodsUS and CDUS were ordered to evaluate the cause of hematochezia in 13 infants of less than 6 months old. All infants presented with blood stools and the suspicion of allergic colitis. The diagnostic standard used was the response to exclusion diet, confirmed by challenge test after four weeks of clinical improvement. These patients were from the pediatric gastroenterology clinic of our institution and examination before starting the elimination diet. All were evaluated and investigated by pediatric gastroenterologists, who requested US and CDUS scans and follow-up colonoscopies when indicated. The time lapse between the first clinical examination and US was one week, at most. Colonoscopy and mucosal biopsies were performed to rule out other pathologies when the hematochezia had not improved after exclusion diet. Thirteen infants underwent US and CDUS, exclusion diet and challenge test. Only four patients underwent colonoscopy (infants who were breastfed and had not improved after exclusion diet for their mothers). The findings of US and CDUS were compared to clinical response and colonoscopic findings. Besides hematochezia, infants presented other symptoms: diarrhea, vomiting, refusing breastfeeding, and colic. The Ethics Committee approved the performance of the study without informed consent.
The diagnosis of proctocolitis secondary to CMA was based on 1) clinical findings (bloody stool with or without diarrhea) and 2) clinical recovery after infant or mother exclusion diet (when breastfeeding). Extensively hydrolyzed or aminoacid formula was used for the exclusion diet when the infant was formula fed. When the child was partially or exclusively breastfed, breastfeeding was maintained and the mother was oriented to exclude cow's milk and its derivatives from her diet.6
Suggestive US and CDUS colitis findings were considered when: 1) increased Doppler vascularity in the intestinal wall (five or more vessels in the bowel wall in a segment of approximately 2cm2); and 2) wall thickening ≥ to 3mm.14 US and CDUS were performed at beginning, when child had hematochezia and CMA was suspected, and repeated after four weeks of exclusion diet.
US and CDUS techniqueUS and CDUS were performed using a XP10 (Acuson, Mountain View, CA, USA) system using a 7.5MHz linear transducer or a HD11 (Phillips Medical Systems, Bothell, WA, USA) system using a 12-15MHz linear transducer. Our US and CDUS routine consisted of scanning all four abdominal quadrants. Study times ranged from 10 to 15min. Grayscale ultrasound was used to evaluate the bowel wall thickness. All colon segments were examined using cross-sectional and longitudinal views with continuous imaging starting from the caecum to the most distal segment of the sigmoid flexure. Finally, the rectum was examined with full bladder. Bowel wall thickness was measured from the serosa to the intestinal mucosa and all colonic segments were recorded. A bowel wall thickness ≥ 3mm in the transversal or longitudinal section was classified as abnormal. The thickest bowel wall was chosen from five subsequent measurements of each bowel segment. Measurements were taken in regions without haustral folds in the colon. CDUS was used to evaluate bowel wall vascularity according to the number of vessels in a 2cm2 area. For color Doppler studies, parameters were adjusted to detect low-velocity flows, and the adopted gain adjustment criterion was the appearance of color artifacts. Pulsatile pixels were classified as vessels. All ultrasound studies were performed and reported by the same experienced pediatric radiologist.
ResultsThirteen infants (between one and six months of age) with hematochezia were studied. Nine (69%) were female. Nine infants were exclusively breastfed and two partially (one was complemented with cow's milk formula and one with soy formula); two were receiving exclusively cow milk infant formula.
Seven of the 13 infants (53.8%) had grayscale and color Doppler sonographic repeated after exclusion diet. Twelve of thirteen (92,3%) showed abnormalities at US and CDUS at beginning. One patient had a normal US e CDUS performed four days after the exclusion diet had started. The positive findings suggesting colitis were thickened bowel walls and increased vascularity, especially in the descending and sigmoid colon.
The bowel wall layers were not well defined. The greatest thickening was found in the mucosa and the highest number of vessels was found in the submucosa. All patients had both findings at US and CDUS.
Cow's milk protein allergy was confirmed by the clinical response to exclusion diet and reappearance of symptoms after challenge test with cow's milk. Colonoscopy was only performed on four exclusively breastfed infants with persistent rectal bleeding after mothers exclusion diet. In all infants colitis was confirmed and pathological anatomy study suggested a histological diagnosis of allergic colitis (cryptitis, crypt abscesses and eosinophilic infiltrate). All of them had breastfeeding substituted by amino acid formula, improving the hematochezia.
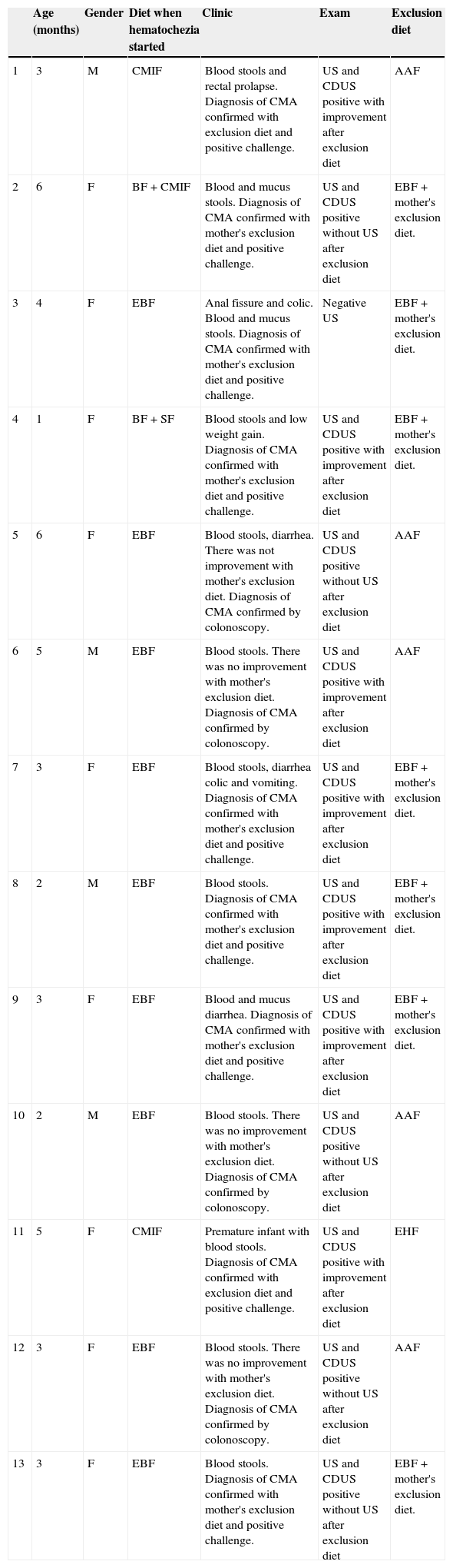
After one month of follow-up with exclusion diet and clinical improvement, the US and CDUS was repeated in 7 infants. All studies were normal, with normalization of intestinal wall thickness and vascularity (Table 1).
Patients’ characterization.
| Age (months) | Gender | Diet when hematochezia started | Clinic | Exam | Exclusion diet | |
|---|---|---|---|---|---|---|
| 1 | 3 | M | CMIF | Blood stools and rectal prolapse. Diagnosis of CMA confirmed with exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | AAF |
| 2 | 6 | F | BF + CMIF | Blood and mucus stools. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive without US after exclusion diet | EBF + mother's exclusion diet. |
| 3 | 4 | F | EBF | Anal fissure and colic. Blood and mucus stools. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | Negative US | EBF + mother's exclusion diet. |
| 4 | 1 | F | BF + SF | Blood stools and low weight gain. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | EBF + mother's exclusion diet. |
| 5 | 6 | F | EBF | Blood stools, diarrhea. There was not improvement with mother's exclusion diet. Diagnosis of CMA confirmed by colonoscopy. | US and CDUS positive without US after exclusion diet | AAF |
| 6 | 5 | M | EBF | Blood stools. There was no improvement with mother's exclusion diet. Diagnosis of CMA confirmed by colonoscopy. | US and CDUS positive with improvement after exclusion diet | AAF |
| 7 | 3 | F | EBF | Blood stools, diarrhea colic and vomiting. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | EBF + mother's exclusion diet. |
| 8 | 2 | M | EBF | Blood stools. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | EBF + mother's exclusion diet. |
| 9 | 3 | F | EBF | Blood and mucus diarrhea. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | EBF + mother's exclusion diet. |
| 10 | 2 | M | EBF | Blood stools. There was no improvement with mother's exclusion diet. Diagnosis of CMA confirmed by colonoscopy. | US and CDUS positive without US after exclusion diet | AAF |
| 11 | 5 | F | CMIF | Premature infant with blood stools. Diagnosis of CMA confirmed with exclusion diet and positive challenge. | US and CDUS positive with improvement after exclusion diet | EHF |
| 12 | 3 | F | EBF | Blood stools. There was no improvement with mother's exclusion diet. Diagnosis of CMA confirmed by colonoscopy. | US and CDUS positive without US after exclusion diet | AAF |
| 13 | 3 | F | EBF | Blood stools. Diagnosis of CMA confirmed with mother's exclusion diet and positive challenge. | US and CDUS positive without US after exclusion diet | EBF + mother's exclusion diet. |
AAF, amino acid formula; CDUS, color Doppler ultrasound; CMA, cow's milk allergy; CMIF, cow's milk infant formula; EBF, exclusively breastfeeding; EHF, extensively hydrolyzed formula; F, female; M, male; SF, soy formula; US, ultrasound.
In pediatrics, US and CDUS have been increasingly used to evaluate acute and chronic abdominal vascular disorders and intestinal inflammation.10 Inflammatory and infectious intestinal diseases cause thickening of the intestinal wall that can be detected using US.11 CDUS detects increases in vessel density in the intestinal wall when there is active inflammation. The physiopathology of CMA in infants is usually associated with intestinal inflammation, and ultrasound may, therefore, detect these changes. When associated with clinical parameters, ultrasound may be useful to suggest the diagnostic hypothesis of CMA.11–14 In the present study, the role of Doppler US was to evaluate vascular changes in the intestinal wall of infants with rectal bleeding and abdominal pain. Doppler US features help to confirm the presence of findings indicating the diagnosis of colitis, complementing the clinical findings suggestive of CMA. Doppler US was also an important diagnostic tool to rule out other abdominal diseases, such as intestinal intussusception.
These US and CDUS findings are unspecific, as they can also be found in some infectious colitis, however correlating these US findings with color Doppler, clinical data, and laboratory tests enables us to order another test that will lead to a final diagnosis. Doppler ultrasound was employed as a tool for the differential diagnosis of allergic colitis and to reveal vascular changes on Doppler confirmed by medical assessment or colonoscopy.
We showed abnormalities in 12/13 infants at the diagnosis. One study was negative. We suppose that the delay in perform the US and CDUS could explain this negative result. Based in a previous study of our group, the best part of the colon to identify inflammation at US and CDUS is the right colon. So, inflammation predominantly at rectum and sigmoid could not be visualized at US and CDUS.11
Unfortunately only seven infants performed the second ultrasonographic study to confirm the disappearance of abnormalities visualized at beginning.
The response to exclusion diet and oral challenge test may yield false positive or false negative results in children since tolerance may develop early, resulting in negative tests. Moreover, an early oral challenge may not be advantageous in some cases because it can lead to potential harmful clinical manifestations.15–17
To the best of our knowledge, only 3 studies described US findings in allergic colitis associated to cow's milk protein; two have shown grayscale US findings in allergic colitis.11–13 and one was an extensive retrospective study about Doppler ultrasound in pediatric inflammatory bowel diseases illustrating a CMA case.11
Some cases of allergic colitis have been a diagnostic challenge and require invasive tests, such as colonoscopy, for confirmation. This diagnostic challenge has raised the need to develop another accurate and non-invasive test for early detection and follow-up. As the present report depicted 12/13 infants with positive imaging findings of colitis on Doppler US, our results have shown the significant contribution of US at the symptomatic period when there is suspicion of the diagnosis of cow's milk allergy. Unfortunately we could not document how accurate this method could be with improving of ultrasonographic findings when the infant had responded to the exclusion diet as well as after challenge diet. In other study of our group we could show the improving after exclusion diet, however as the US was performed just after reappearance of symptoms, the US findings were less intensive compared to the first US.
The experience and expertise of the ultrasonographist is very important to obtain these results. Reproducibility is the main limitation of this method, as it is operator dependent. Cut points for the CDUS findings should be established in large sample of patients for an effective use of this technique.
One limitation of this study was that it was a retrospective assessment of patients with a diagnosis of allergic colitis. To solve these possible limitations, future prospective studies should be carried out with infants with suspected allergic proctocolitis to determine the accuracy of the US diagnostic method. Another limitation was the use of two different US equipments: XP10 and HD11. The use of different technologies did not interfere in our results, as only 1 of the 13 studied subjects was assessed by the older (XP10) equipment that revealed colitis changes. Another limitation of this study is that we did not use a Power Doppler, which could have detected low flow vessels.
In conclusion, Doppler US has been used in the diagnostic evaluation of infants with abdominal pain and intestinal bleeding, and could be a tool for the cow's milk protein allergy diagnosis, especially with colitis. The presence of increased colonic wall thickness and vascularity at Doppler is indicative of intestinal inflammation, adding an important element in the correct clinical setting.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Epifanio M, Spolidoro JV, Missima NG, Soder RB, Garcia PC, Baldisserotto M. Cow's milk allergy: color Doppler ultrasound findings in infants with hematochezia. J Pediatr (Rio J). 2013;89:554–558.