To analyze the prevalence and impact of asthma in schoolchildren from the city of Caxias do Sul, RS, Brazil.
MethodsCross-sectional observational and case-control study with children and adolescents between 7 and 15 years old, from public schools in Caxias do Sul, RS. The study is composed of two phases: Phase I analyzed the prevalence of asthma in the delimited population, investigating 1915 schoolchildren; Phase II quality of life questionnaires, asthma control and classification (for the asthmatic group), physical activity, school performance, pulmonary function tests and anthropometric measures were applied to 266 asthmatics and 288 controls.
ResultsThe estimated prevalence of asthma was 16.1%. In the comparison between asthmatics and nonasthmatics premature birth (p<0.001) and diagnosis of another chronic disease at birth (p<0.001) were found. Regarding pulmonary function, significant differences were found in the values between groups in FEV1, FEV1/FVC and forced expiratory flow in the 25 and 75% (FEF25–75%), being that asthmatics presented lower values. Among asthmatics, 133 (50.8%) did not have the disease controlled. In the anthropometric variables, significant differences were observed, with higher values in controls, in the the waist-to-height ratio (p=0.009) and in the perception of health (p<0.001). Quality of life is lower in asthmatics in the physical well-being domain (p=0.001) and in the total score (p=0.016). The total school performance score did not present a statistically significant difference between the groups.
ConclusionThe prevalence of asthma is similar to that of other industrialized urban centers and may negatively affect some areas of the development of schoolchildren.
Analisar a prevalência e o impacto da asma em escolares do município de Caxias do Sul-RS.
MétodosEstudo analítico observacional transversal e caso-controle, com crianças e adolescentes entre sete e 15 anos, de escolas da rede pública de Caxias do Sul-RS. O estudo é composto por duas fases: Fase I analisou a prevalência da asma na população delimitada e investigou 1.915 escolares; Fase II foram aplicados a 266 asmáticos e 288 controles, questionários de qualidade de vida, classificação e controle da asma (para o grupo asmático), atividade física, desempenho escolar, espirometria e antropometria.
ResultadosA prevalência de asma estimada foi de 16,1%. Na comparação entre asmáticos e não asmáticos foram encontradas diferenças na prematuridade (p<0,001) e ter diagnóstico de outra doença crônica ao nascer (p<0,001). Na espirometria foram encontradas diferenças significativas entre os grupos nos valores de VEF1, VEF1/CVF e fluxo expiratório forçado nos momentos 25 e 75% (FEF25-75%); os asmáticos apresentaram valores inferiores. Entre os asmáticos, 133 (50,8%) não tem a doença controlada. Nas variáveis antropométricas foram observadas diferenças significativas, com valores superiores entre os controles, na classificação razão cintura/estatura (p=0,009) e na percepção da própria saúde (p<0,001). A qualidade de vida é menor nos asmáticos no domínio bem estar físico (p=0,001) e no escore total (p=0,016). O escore total do desempenho escolar não apresentou diferença estatisticamente significativa entre os grupos de estudo.
ConclusãoA prevalência de asma se assemelha à de outros centros urbanos industrializados e pode impactar negativamente alguns domínios do desenvolvimento dos escolares.
Asthma is a severe global health problem that affects all age groups. Its prevalence is increasing in many countries, especially among children.1 It is considered the main chronic respiratory disease in childhood, resulting in significant quality-of-life impairment for patients and their families, with high direct and indirect costs to society. According to a Brazilian study, the asthma prevalence in children and adolescents was 24.3% and 19%, respectively.2 In the same study, the highest prevalence rates of asthma and allergic diseases were observed in the urban centers of the North and Northeast, except for asthma, which was also observed in the South.
Asthma is characterized by a history of respiratory symptoms such as wheezing, shortness of breath, tightness in the chest, and coughing, which vary in time and intensity, together with variable limitation of expiratory airflow. Children with asthmatic respiratory symptoms have impaired lung function and, therefore, may be more susceptible to environmental factors, as well as being at increased risk of declining lung function in adulthood.3 According to the Global Initiative for Asthma (GINA), asthma should be classified as well controlled, partially controlled, or uncontrolled, based on symptom assessment. Thus, a patient with controlled asthma should be free of diurnal symptoms, nocturnal awakenings, need for rescue medication, and the limitations in daily activities and the practice of physical activities.1 Chronic diseases often significantly interfere with quality of life. However, individual characteristics and different lifestyles make the disease impact diverse; it often does not correlate with the severity or prognosis of the disease itself.4
Comparative studies of physical activity levels between young asthmatic and non-asthmatic individuals do not show similar results. However, higher levels of activity are associated with a higher rate of asthma reports or associated symptoms.5 The practice of physical activity by asthmatic individuals, when performed with adequate intensity and duration, improves the physical capacity and decreases dyspnea. Moreover, it may result in improved medication administration and use, reducing the severity of exercise-induced bronchospasm, with a consequent improvement in the quality of life.6
Another factor related to asthma is school performance, whereupon many children with asthma miss school due to the asthma crises, impairing their educational achievement.6 Similarly, activities that involve social interaction with peers, such as games that require physical effort, also tend to be avoided by children with asthma, and depending on how teachers address the limitations of asthmatics, they may feel socially excluded.7 In this context, the present study investigated the prevalence and impact of asthma in schoolchildren from the municipality of Caxias do Sul/RS.
MethodsThe present study comprised two phases: the first was an observational descriptive (cross-sectional) study and the second one was an observational analytical (case-control) study.
This study included children and adolescents regularly enrolled in elementary schools of the Municipal Education Network of Caxias do Sul-RS. The inclusion criteria were defined as follows: schoolchildren aged 7–16 years of both genders, with an asthma diagnosis (cases), and without an asthma diagnosis and previously healthy (controls).
Schoolchildren with cognitive or motor limitations, or with other chronic diseases that could impair the assessment of asthma or quality of life, were excluded.
In study Phase I, in which the objective was to investigate the prevalence of asthma and to characterize the sample economically, parents or guardians answered the standard written questionnaire (WQ), which corresponds to the first part of the written questionnaire of the International Study of Asthma and Allergies in Childhood (ISAAC)8 and the economic classification questionnaire, which used the Brazilian Economic Classification Criteria (Critério de Classificação Econômica do Brasil [CCEB]).9
In study Phase II, in which the objective was to investigate the impact of asthma, the following tools were used: to evaluate health-related quality of life, the KINDL (Kinder Lebensqualität Fragebogen) QL-Generic Questionnaire was applied.10 The questionnaire consists of 24 questions covering six quality of life dimensions: physical well-being, emotional well-being, self-esteem, family, friends, and school routine. Complementing the measurement of the quality of life data, children/adolescents diagnosed with asthma answered a specific questionnaire about asthma-related quality of life. The KINDL QL-Specific Questionnaire, validated in Brazil,11 consists of 15 questions regarding the disease, directed towards the patients’ quality of life in the week preceding the interview. The Asthma Control Test (ACT) questionnaires were used to investigate asthma control.12
In the evaluation of pulmonary function, the technical procedures and the acceptability and reproducibility criteria for performing pulmonary function tests followed the guidelines of the American Thoracic Society/European Respiratory Society (ATS/ERS).13 A KoKo® spirometer (nSpire Health, Inc; KoKo®, CO, USA) was used with its own software. The assessments were carried out in the field by two researchers trained and capable of carrying out the measurements. The values found in the Brazilian Consensus of Spirometry were used as references for the percentage of the predicted values in liters.14
The children answered the Physical Activity Questionnaire for Children (PAQ-C) and the adolescents, the Physical Activity Questionnaire for Adolescents (PAQ-A), which identify the level of physical activity. The tool investigates moderate and intense physical activities in the seven days prior to completing it. This questionnaire consists of nine questions about the practice of sports and games, physical activities at school, and leisure. Each question has a score ranging from 1 (did not practice activity) to 5 (practiced every day of the week) and the final score is the mean of the questions.15
As for the anthropometric measures, the procedures were as follows: body mass was obtained using a digital scale (G-Tech, Glass 1 FW – Rio de Janeiro, Brazil), with an accuracy of 100g; height was measured using a portable stadiometer (AlturaExata, TBW – São Paulo, Brazil), with a precision of 1mm; for waist circumference, a measurement tape was utilized, measuring the mid-point between the lower rib and the iliac crest. Based on these measurements, the body mass index (BMI) was calculated by dividing body mass (kg) by height2 (m), and the classification was made according to the percentile for age, considering the reference distribution of the Centers for Disease Control and Prevention (CDC).16 The waist-to-height ratio was obtained by dividing waist circumference (cm) by height measurement (cm). A waist/height ratio value ≤0.50 was used as a cutoff point for low coronary risk, whereas values ≥0.51 were used for high risk.17
When evaluating school performance, the School Performance Test (Teste de Desempenho Escolar [TDE])18 was used, which is a tool that aims to provide an objective assessment of the essential abilities for school performance, specifically regarding writing, arithmetic, and reading. It indicates, in a comprehensive way, which areas of school learning are preserved or impaired in the patient.
In the descriptive analysis, the categorical data were shown as absolute and relative frequencies, and the continuous variables as means and standard deviations. The Shapiro-Wilk test was applied to test for normality. In the inferential analysis, the continuous variables were analyzed by the Mann–Whitney test and the categorical variables by the chi-squared test. All analyses were performed using the SPSS program (SPSS Statistics for Windows, Version 20.0. NY, USA). The differences were considered significant for p≤0.05.
The study was approved by the research ethics committee of the Universidade de Caxias do Sul (UCS), under opinion No. 1,453,525. The parents/guardians signed the informed consent the children and adolescents signed the informed assent.
ResultsPhase I of the study involved 1915 schoolchildren and Phase II, 554 (266 asthmatics and 288 controls). The adherence rate was 83% (1915/2307), with an asthma prevalence rate estimated at 16.1% (309/1915), according to the criteria established by the ISAAC protocol, in which 920 (48%) schoolchildren had a wheezing episode, 700 (36.6%) had a confirmed medical diagnosis of asthma sometime during their lifetime, and 372 had a wheezing episode in the previous 12 months (19.4%). Moreover, 444 (23.2%) schoolchildren reported having used medication for the disease at least once in the previous twelve months.
Of the 1915 schoolchildren evaluated at this stage, 953 (49.8%) were males, with a mean age of 10.77±2.55 years. For the purpose of economic classification and level of schooling of the parents/guardians, 1833 (95.7%) belonged to classes B and C, and 852 (44.5%) had finished high school.
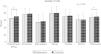
When comparing the groups (asthmatics and controls), the results showed significantly higher results among the asthmatics for the variables age (p=0.041), rates of preterm birth (p<0.001), and diagnosis of another chronic disease at birth (p<0.001), as shown in Table 1.
Evaluation of the classification between the group of asthmatics (n=309) and controls (n=1606) in Phase I of the study.
| Asthmatics n (%) | Controls n (%) | p | |
|---|---|---|---|
| Classification of schoolchildren | |||
| Male gender (%) | 145 (46.9) | 808 (50.3) | 0.29 |
| Age, years (M±SD) | 10.5±2.5 | 10.8±2.6 | 0.04 |
| Preterm birth | 50 (16.2) | 134 (8.3) | <0.001 |
| Another chronic disease (rhinitis, atopy, ADHD) | 66 (21.4) | 109 (6.8) | <0.001 |
| Classification of parents/guardians | |||
| Parents’/guardians’ level of schooling | |||
| Elementary school – first 4 years | 28 (9.0) | 204 (12.8) | 0.38 |
| Elementary school – 8 years | 113 (36.6) | 533 (33.2) | |
| High school | 138 (44.7) | 714 (44.5) | |
| College/university | 30 (9.7) | 155 (9.7) | |
| Economic classification | |||
| Class A | 2 (0.6) | 18 (1.1) | 0.93 |
| Class B | 147 (47.6) | 773 (48.1) | |
| Class C | 149 (48.2) | 764 (47.6) | |
| Class D | 10 (3.2) | 48 (3.0) | |
| Class E | 1 (0.3) | 3 (0.2) | |
M±SD, mean and standard deviation; ADHD, attention deficit hyperactivity disorder. Tests applied: chi-squared and Mann–Whitney.
In study Phase II, 554 (28.9%) of the eligible students were included in the study, of whom 266 (48%) were asthmatics and 283 (51.1%) were males, with a mean age of 10.8±2.4 years (10.7±2.3 for asthmatics and 10.9±2.4 for controls, p=0.264). Of the 262 asthmatics who answered the disease control questionnaire, 129 (49.2%) reported having controlled disease and 133 (50.8%), uncontrolled disease.
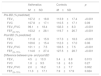
Regarding pulmonary function (Table 2), there were significant differences between the groups regarding forced expiratory volume in the first second (FEV1), forced vital capacity (FEV1/FVC), and forced expiratory flow between the moments of 25% and 75% (FEF25–75%), showing that asthmatic patients had lower pulmonary function when compared to controls. Furthermore, asthmatics have bronchodilator response rates above that of controls.
Comparison between lung volume and capacity in asthmatic students (n=266) and controls (n=288).
| Asthmatics | Controls | p | |
|---|---|---|---|
| M±SD | M±SD | ||
| Pre-BD (% predicted) | |||
| FEV1 | 107.2±18.8 | 113.9±17.4 | <0.001 |
| FVC | 107.8±17.1 | 110.5±17.1 | 0.09 |
| FEV1/FVC | 99.1±18.4 | 102.3±8.3 | <0.001 |
| FEF25-75% | 103.2±28.1 | 119.7±26.7 | <0.001 |
| Post-BD (% predicted) | |||
| FEV1 | 111.8±15.9 | 117.3±18.3 | <0.001 |
| FVC | 109.6±15.4 | 112.3±17.0 | 0.06 |
| FEV1/FVC | 101.1±7.5 | 103.5±7.5 | <0.001 |
| FEF25–75% | 114.6±27.4 | 127.5±28.7 | <0.001 |
| Difference between pre- and post-BD | |||
| FEV1 | 4.5±13.3 | 3.4±8.8 | 0.013 |
| FVC | 1.8±9.5 | 1.8±6.3 | 0.27 |
| FEV1/FVC | 2.0±16.2 | 1.3±7.7 | 0.002 |
| FEF25–75% | 11.3±17.1 | 7.9±17.9 | 0.024 |
BD, bronchodilator; FEV1, forced expiratory volume in the first second; FVC, forced vital capacity; FEF25–75%, forced expiratory flow between 25% and 75%; M±SD, mean and standard deviation.
Test applied: Mann–Whitney.
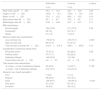
When analyzing the anthropometric profile data (Table 3), 25.9% of the 266 asthmatics, and 23.6% of the 288 controls were overweight/obese, based on the body mass index (BMI). As for the waist/height ratio, 31.6% and 21.2%, respectively, had high coronary risk. Significant differences related to the disease were found only in the variable waist-to-height ratio (p=0.009). Regarding physical activity, the average weekly screen time among the 266 asthmatics comprised 32.2h in front of the television, video game and/or computer. Among the 288 controls, the total weekly screen time was 29.4h. Therefore, 79.7% and 74.3% of the assessed individuals, respectively, showed a sedentary lifestyle risk. This information was confirmed, in part, since more than half of the asthmatic, 146 (54.9%) and 49% (141) of non-asthmatic individuals were classified as sedentary, based on the number of minutes of weekly physical activity. Even so, the vast majority perceives their health as good or very good (63.5% of asthmatics and 65.6% of controls), with statistical differences between the groups regarding their health perception (p<0.001).
Anthropometric evaluation and physical activity levels of asthmatics (n=266) and controls (n=288).
| Asthmatics | Controls | p-value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Body mass, kg (M±SD) | 43.3±14.9 | 42.5±14.8 | 0.43 |
| Height, cm (M±SD) | 145.0±14.7 | 145.6±14.0 | 0.57 |
| Waist, cm (M±SD) | 70.0±12.2 | 68.6±12.2 | 0.19 |
| Body mass index (M±SD) | 20.1±4.5 | 19.5±4.0 | 0.11 |
| Waist/height ratio (M±SD) | 0.48±0.08 | 0.47±0.07 | 0.11 |
| BMI classification | |||
| Normal weight | 194 (72.9) | 211 (73.3) | 0.49 |
| Overweight | 48 (18) | 55 (19.1) | |
| Obese | 21 (7.9) | 13 (4.5) | |
| Waist-to-height ratio classification | |||
| Low coronary risk | 179 (67.3) | 218 (75.7) | 0.009 |
| High coronary risk | 84 (31.6) | 61 (21.2) | |
| Total minutes of activity (M±SD) | 212.6±274.5 | 236.0±309.6 | 0.10 |
| Classification of physical activity level | |||
| Physically active | 73 (27.4) | 82 (28.5) | 0.29 |
| Partially active | 47 (17.7) | 65 (22.6) | |
| Sedentary lifestyle | 146 (54.9) | 141 (49) | |
| Total screen time (M±SD) | 4.6±3.2 | 4.2±3.2 | 0.129 |
| Total screen time classification | |||
| <2–h/day – no risk of sedentary lifestyle | 54 (20.3) | 74 (25.7) | 0.158 |
| >2 h/day – risk of sedentary lifestyle | 212 (79.7) | 214 (74.3) | |
| Students’ own health perception | |||
| Poor | 7 (2.6) | 3 (1.0) | |
| Regular | 68 (25.6) | 45 (15.6) | |
| Good | 128 (48.1) | 134 (46.5) | <0.001 |
| Very good | 41 (15.4) | 55 (19.1) | |
| Excellent | 18 (6.8) | 38 (13.2) | |
M±SD, mean and standard deviation.
Tests applied: chi-squared and Mann–Whitney.
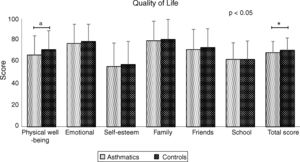
Fig. 1 shows the average scores in the assessed domains for health-related quality of life (HRQoL) among the studied groups. The asthmatic group had a statistically significant difference in the physical well-being domain (p=0.001) and in the total quality of life score (p=0.016) when compared to the control group.
Regarding the quality of life related to the disease, the total score of the asthma module was 78.5±15.5 points, demonstrating that asthma does not interfere in the quality of life of asthmatic children, as they show values that are clinically within acceptable standards (>70% of the total score).
When evaluating school performance, no significant differences were observed between the groups (p=0.64). However, asthmatics scored lower on all tests. The asthmatics obtained an average of 107.2±27.0 points in the total score (maximum possible score of 143 points) and the controls obtained 109.5±23.0 points. Specifically in the subtests, the observed values were 25.6±8.6 and 26.4±7.6 in writing (maximum possible score of 35 points); 18.0±8.0 and 18.4±7.5 in arithmetic (maximum possible score of 38 points) and 63.5±14.0 and 64.2±11.3 in reading (maximum possible score of 70 points), for asthmatics and controls, respectively.
DiscussionThis study aimed to evaluate the prevalence of asthma in children/adolescents of an industrial urban center in Serra Gaúcha, state of Rio Grande do Sul, Brazil. As a main result, 16.1% of the assessed students were identified as asthmatics, with more than half of them having uncontrolled disease. Regarding the impact of asthma on schoolchildren's development, there was a significant impact on lung function, waist/height ratio, quality of life and one's perception of their own health.
In the present study, the prevalence of asthma was slightly lower (16.1%) than in other studies carried out with schoolchildren from all over Brazil19 and with students from Porto Alegre/RS.20 In a cross-sectional study carried out in 2012, with a sample involving the five regions of Brazil, 26 state capitals and the Federal District (n=109,104), the prevalence of asthma symptoms was 23.2%.19 In another study with schoolchildren from Porto Alegre, the city capital of the state of Rio Grande do Sul (n=2500), the prevalence was 28.2%.20 It is important to note that all these studies used the same diagnostic criteria of the disease. Environmental factors are the key to explain the variations and changes in the prevalence of asthma.21 Regarding disease control, the prevalence of 50.9% of asthmatics with uncontrolled asthma in this study is similar to that found in Porto Alegre/RS.20
The development of pulmonary function in children with persistent asthma are less favorable than that observed in the non-asthmatic population. However, studies indicate that more severe asthma may be associated with an increased decline in pulmonary function, while milder asthma may be associated with near-normal rates of decline in pulmonary function.22 Another factor related to the prevalence of asthma and decreased pulmonary function is preterm birth. In this study, the prevalence of preterm birth was practically twice as high among asthmatics when compared with non-asthmatics. A meta-analysis with 24,938 children showed that children born with lower gestational age had reduced values of FEV1, FEV1/FVC, and forced expiratory flow at the 75% moment (FEF75%).23
In relation to the level of physical activity, the prevalence of a sedentary lifestyle and number of hours of screen time was high in both assessed groups. A similar outcome was found in a study that compared the level of physical activity of 155 asthmatic children and 158 controls in Portugal.24 The study concluded that although parents of asthmatic children state that their children's disease is an impediment to physical activity, it seems there are no differences between the level of physical activity of the controlled asthmatic children and their peers. Moreover, the asthmatic students’ total number of hours of screen time was comparable to that of the students without the disease. A prevalence of excessive screen time of 79.5% was found among 2874 adolescents in a study carried out in the city of João Pessoa-PA; however, the study found no association between excessive screen time and physical activity level and nutritional status.25
The prevalence of overweight and obesity in childhood has increased substantially worldwide in less than a generation. In Brazil, this figure increased from 15% in 2002 to 25% in 2010.26 In this study, similar percentages of overweight/obesity were observed among asthmatics and controls (25.9% and 23.6%, respectively). Among the schoolchildren from Porto Alegre, no significant differences were found between the study groups; however, the percentages were higher than in this study (34.8% and 32.7%, respectively).20 However, significant differences were observed between the groups regarding abdominal fat, evaluated by waist/height ratio (p=0.009). A study carried out with schoolchildren aged 6–12 years in the state of Bahia suggests that an increase in fat deposits, whether in the abdominal region or elsewhere in the body, increases the risk of wheezing episodes.27
It has been shown that asthma affects the health-related quality of life of asthmatics, specifically in the physical well-being domain and also in the total score. These findings are similar to those found in a sample of 480 schoolchildren from a city in the state of Rio Grande do Sul, where the asthma group showed a worse score in the physical well-being domain (p<0.001) and in the total quality of life score (p=0.025) when compared to the control group.28 In a sample from the capital city of Rio Grande do Sul, 290 asthmatics showed lower scores than the 315 controls in the physical well-being domain (p<0.001), in addition to significant differences in emotional well-being and self-esteem.20
The school performance of asthmatics was lower than that of the control group, but the differences were not significant. One study with children and adolescents from the city of Maceió-AL compared the school performance of 188 asthmatics and 213 controls and concluded that asthma did not interfere with school performance, which was evaluated by the average of all first semester grades.29 Another study, corroborating the present result, showed that there were no significant differences in performance between asthmatics and non-asthmatics in 3812 schoolchildren from the United States aged 8–17 years. However, schoolchildren with persistent asthma showed lower values of academic achievement when compared to asthmatics with mild asthma. The same study found a significant inverse correlation between absenteeism and school performance (p<0.001). This led the authors to conclude that the severity of asthma, which is one of the main determinants of absenteeism, may be an important factor in decreasing school performance.30
Even if the results do not prove the negative impact of asthma on all studied variables, it is important to carry out further studies on this subject, aiming to identify other associations between them. Finally, characteristics of the level of physical activity, hours of screen time, anthropometric profile, and school performance need to be observed by school and health professionals and family, aiming to develop a collective plan that will favor a better quality of life for non-asthmatic students, but especially those with asthma.
Some study limitations are associated with the fact that the investigation of the impact of asthma was limited to obtaining information from the children and adolescents. Thus, this study did not obtain more precise data regarding disease control, medical consultations, hospitalizations, school absenteeism, treatment, and quality of life, where parents or guardians could provide more accurate information.
FundingCoordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Zacaron D, Roncada C, Molin RS, Jones MH, Pitrez PC. Prevalence and impact of asthma in schoolchildren in the city of Caxias do Sul-RS. J Pediatr (Rio J). 2020;96:479–86.