To determine the prevalence of enuresis, urinary, and bowel symptoms and associated factors in children aged 7 years in a birth cohort.
MethodsA pre-coded questionnaire was applied to 3,602 children who belonged to a birth cohort initiated in 2004 in Pelotas, Brazil. During home visits at 12, 24, and 48 months and at age 7 years, mothers answered a questionnaire with demographic questions and characteristics of bladder and bowel habits of children using a urinary symptom score. Poisson regression was used for the hierarchical multivariable analysis, with robust variance.
ResultsThe prevalence of enuresis was 10.6%;11.7% in males and 9.3% in females; enuresis was monosymptomatic in 9.8% of the children (10.8% of males and 8.3% of females); 37.4% had symptoms up to once a week; 32.9%, two to four times a week; and 26.2%, every day, with no difference between genders. The most common urinary symptoms were urinary urgency (22.7%) and urinary retention maneuvers (38.2%). In the multivariate analysis, it was observed that the number of urinary symptoms and the number of children at home showed a direct association with the presence of enuresis, whereas maternal education was inversely associated.
ConclusionsEnuresis is a prevalent condition and should be investigated in clinical practice, especially in children of lower socioeconomic status. A detailed history of urinary habits detects associated urinary symptoms, which is important for adequate classification of enuresis and subsequent management.
Determinar a prevalência de enurese, sintomas urinários e intestinais e fatores associados em crianças de sete anos, em uma coorte de nascimentos.
MétodosFoi aplicado um questionário pré-codificado em 3.602 crianças pertencentes à coorte de nascimentos iniciada em 2004, em Pelotas, RS. Em visitas domiciliares realizadas aos 12, 24 e 48 meses e aos sete anos, as mães responderam um questionário com questões sociodemográficas e sobre as características e hábitos miccionais e intestinais das crianças, utilizando um escore de sintomas miccionais. Para a análise multivariável hierarquizada, utilizou-se regressão de Poisson com variância robusta.
ResultadosA prevalência de enurese de foi 10,6%, sendo 11,7% nos meninos e 9,3% nas meninas; a enurese foi monossintomática em 9,8% das crianças (10,8% dos meninos e 8,3% das meninas); 37,4% apresentavam o sintoma até uma vez por semana; 32,9%, duas a quetro vezes por semana; e 26,2% todos os dias, sem diferença entre os sexos. Os sintomas urinários mais frequentes foram urgência miccional (22,7%) e manobras de contenção urinária (38,2%). Na análise multivariável, observou-se que o número de sintomas miccionais e o número de crianças em casa mostraram relação direta com presença de enurese, enquanto que a escolaridade materna apresentou relação inversa.
ConclusõesA enurese é uma patologia prevalente e deve ser investigada em consultas de rotina, especialmente em crianças com menor nível socioeconômico. Uma história detalhada sobre hábitos urinários pode detectar sintomas miccionais associados, importantes para uma adequada classificação da enurese e posterior manejo.
Enuresis is the involuntary loss of urine at night, in the absence of organic disease, at an age when it would be expected for the child to control urination (usually after 5 years).1 Its natural history suggests symptom regression up to adolescence and adulthood, with annual remission rates around 15%. Still, enuresis affects many families, as it can cause social and emotional stigma, stress, and inconvenience for children and parents.
The prevalence of enuresis varies with age. Studies conducted with 7-year-old children have reported prevalence rates of 7% to 10%, considering both children that wet the bed once a month and those who do it every night.2–4 Enuresis is classified as primary (symptoms were always present) or secondary (at least six months without bedwetting and return of symptoms).5 Primary enuresis appears to result from nocturnal polyuria or decreased bladder capacity, together with the incapacity of child to wake up in response to bladder fullness.2,3,5
Regarding the presence of other urinary symptoms, it is classified as monosymptomatic enuresis (ME), when the only symptom is enuresis, and non-monosymptomatic enuresis (NME), with the presence of other urinary symptoms (urinary urgency, urinary incontinence, urinary retention maneuvers, and increased number of daily micturitions).6 The prevalence of NME enuresis is not well known in population-based samples, with estimates ranging from 20% to 80% of children with enuresis.6 A careful history is required to detect these symptoms. The classification of enuresis modifies the therapeutic approach and, consequently, its prognosis.
The studies generally investigate samples of schoolchildren and users of outpatient services, with scarce population-based and cohort researches, especially with Brazilian children.
The aim of this study was to determine the prevalence of enuresis, urinary and bowel symptoms, and associated factors in children aged 7 years belonging to the Pelotas birth cohort of 2004.
MethodsThis study followed a birth cohort initiated in 2004 in the city of Pelotas, state of Rio Grande do Sul, Brazil. Mothers living in the city were interviewed during hospitalization for childbirth, and their babies were measured (length and weight) and examined. The children were reassessed at 3, 12, 24, 48, and 72 months of age, when interviews were conducted with the mothers and anthropometric assessment of children was performed. At each visit, the mothers completed a questionnaire about the child's health, including morbidities, nutrition, sleep patterns, immunizations, urinary and bowel habits, as well as data on maternal health. Details on the methods of the Pelotas Birth Cohort 2004 are available in other publications.7,8 This article excluded children with neurological malformations, cerebral palsy, and the result of twin pregnancies.
The International Classification of Diseases (ICD) version 10 defines enuresis as bedwetting at least once a month for three months, in children aged five years or older.9 The American Psychiatric Association defines enuresis as bedwetting at least twice a month, for three months.10 For this analysis, enuresis was defined as bedwetting at night, at least once a month, in the last three months.
To evaluate other urinary symptoms, the criteria defined by the International Continence Society11 were used: urinary incontinence (involuntary loss of small amounts of urine during the day, at least once every two weeks, in children with sphincter control or, after 3 years of age); increased urinary frequency (urinating more than eight times a day); decreased urinary frequency (urinating less than three times a day); urinary retention maneuvers (child's efforts to suppress the urgency associated with urination, such as crossing the legs, sit on the heels, squeeze the penis); urinary urgency (urgent need to urinate); and dysuria (pain during urination).
Constipation was defined as the report of difficulty in evacuating, interval between bowel movements greater than 72hours, pain on defecation, or hard or lumpy stools.12 Encopresis was defined as the report of fecal escape in the last three months. Both urinary and intestinal symptoms were evaluated regarding frequency: never, sometimes (1-14 days in the month), almost always (15 to 29 days in the month), and always (every day).
The history of urinary tract infection was assessed through family report at each visit made to the cohort: urinary tract infection before 1 year; between 1 and 2 years; between 2 and 4 years; between 4 and 6 years; and at any age up to 6 years.
A score of elimination dysfunction was created, consisting of the number of urinary symptoms, except enuresis, presented by the child at 7 years of age: urinary incontinence, urinary maneuvers, urinary urgency, increased or decreased urination, and encopresis and interval between evacuations > 72hours. The score could range from 0 to 6 (sum of symptoms).
The other variables included in the analysis were: gender of the child, low birth weight (< 2,500g), prematurity (gestational age <37 weeks), number of children in the household in addition to the index child (information collected at the visit of 48 months); maternal characteristics: schooling and age (in years), ethnicity (white, black or mixed-race), parity, maternal paid work, and family socioeconomic level according to the National Economic Indicator (Indicador Econômico Nacional - IEN), in reference quintiles for Pelotas,13 based on information collected during the 48 months.
The interviewers were specially trained to perform the interviews. Quality control, in order to prevent and detect fraud in the interviews, included the repetition of 10% of the interviews at home (using a reduced questionnaire), as well as telephone contact with mothers who had a fixed or mobile telephone (for confirmation of performance and satisfaction with the interview).
The analysis was performed using the Stata 11 (Stata Corp., College Station, TX, United States) software. Chi-squared tests were used to compare prevalence, according to categorical exposures, and linear trend tests were used for ordinal exposures. For the hierarchical multivariable analysis, Poisson regression with robust variance was used, as the prevalence of the outcome was high. The first level included the variables maternal schooling, age, ethnicity, and socioeconomic status; the second level included prematurity, low birth weight, and number of children in the household; the third level included urinary and bowel symptoms and history of previous urinary tract infection. Variables with p<0.20 in the bivariate analysis were used in the multivariate analysis and those with p<0.05 were maintained after adjusting. Males and females were analyzed separately for the differences found in the literature on the prevalence of enuresis between genders.
The study protocol was approved by the Ethics Committee of the School of Medicine of the Universidade Federal de Pelotas. Written consent to participate in the study was requested from all mothers, after they were informed about the study objectives, and confidentiality of information was guaranteed.
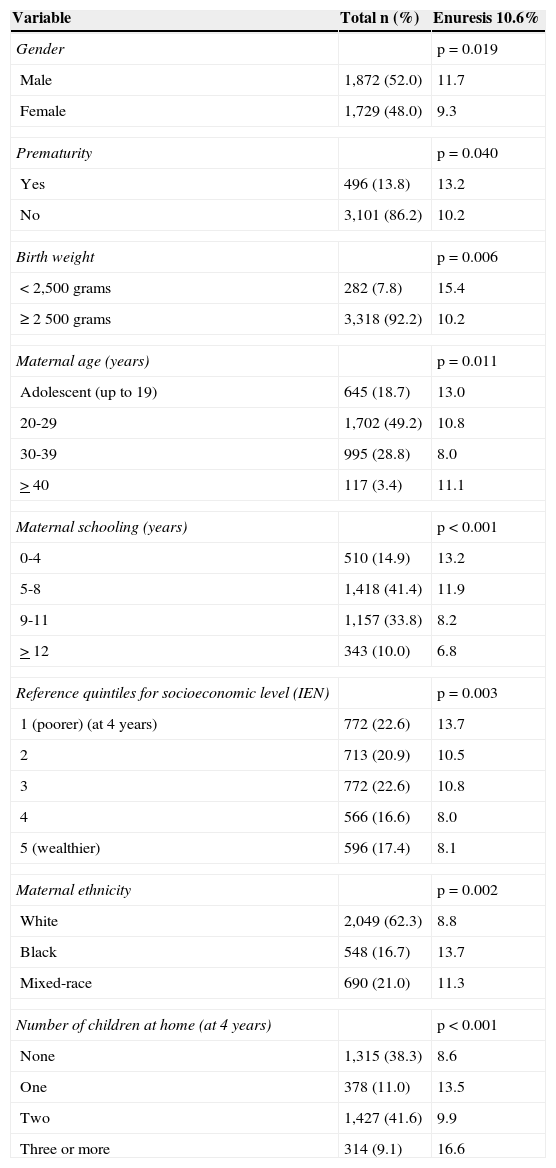
ResultsData on 3,602 children aged between 6 and 7 years were used for this analysis. Table 1 describes the overall sample and the prevalence of enuresis according to maternal, socioeconomic, and demographic variables. 52% of the children were males. The mean age was 6.8 years and 43.5% of families were classified in the two lower income quintiles. The prevalence of enuresis was 10.6%, with a predominance of males (p=0.019). The prevalence of enuresis was inversely associated with socioeconomic status (p=0.003). Enuresis was more common among children with low birth weight, premature children, children of adolescent mothers, lower degree of maternal schooling, black ethnicity, and living in households with three or more children.
Description of the general sample and of children with enuresis.
| Variable | Total n (%) | Enuresis 10.6% |
|---|---|---|
| Gender | p=0.019 | |
| Male | 1,872 (52.0) | 11.7 |
| Female | 1,729 (48.0) | 9.3 |
| Prematurity | p=0.040 | |
| Yes | 496 (13.8) | 13.2 |
| No | 3,101 (86.2) | 10.2 |
| Birth weight | p=0.006 | |
| < 2,500 grams | 282 (7.8) | 15.4 |
| ≥ 2 500 grams | 3,318 (92.2) | 10.2 |
| Maternal age (years) | p=0.011 | |
| Adolescent (up to 19) | 645 (18.7) | 13.0 |
| 20-29 | 1,702 (49.2) | 10.8 |
| 30-39 | 995 (28.8) | 8.0 |
| > 40 | 117 (3.4) | 11.1 |
| Maternal schooling (years) | p<0.001 | |
| 0-4 | 510 (14.9) | 13.2 |
| 5-8 | 1,418 (41.4) | 11.9 |
| 9-11 | 1,157 (33.8) | 8.2 |
| > 12 | 343 (10.0) | 6.8 |
| Reference quintiles for socioeconomic level (IEN) | p=0.003 | |
| 1 (poorer) (at 4 years) | 772 (22.6) | 13.7 |
| 2 | 713 (20.9) | 10.5 |
| 3 | 772 (22.6) | 10.8 |
| 4 | 566 (16.6) | 8.0 |
| 5 (wealthier) | 596 (17.4) | 8.1 |
| Maternal ethnicity | p=0.002 | |
| White | 2,049 (62.3) | 8.8 |
| Black | 548 (16.7) | 13.7 |
| Mixed-race | 690 (21.0) | 11.3 |
| Number of children at home (at 4 years) | p<0.001 | |
| None | 1,315 (38.3) | 8.6 |
| One | 378 (11.0) | 13.5 |
| Two | 1,427 (41.6) | 9.9 |
| Three or more | 314 (9.1) | 16.6 |
IEN, Indicador Econômico Nacional.
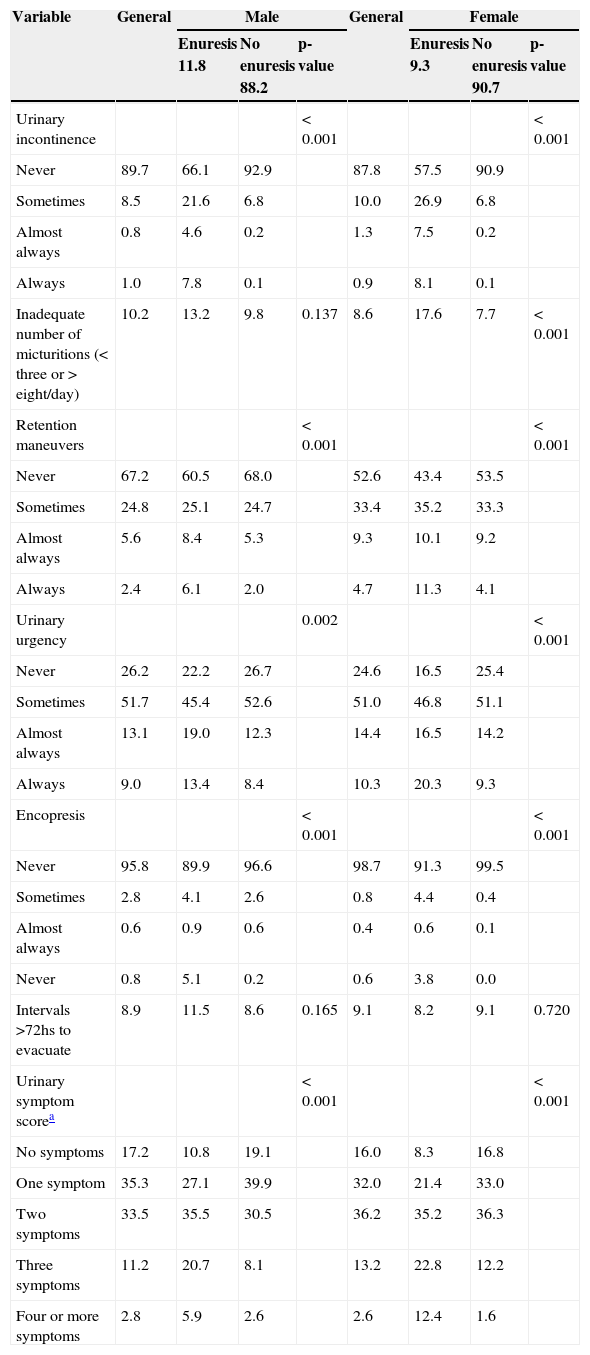
Table 2 shows the prevalence of urinary and bowel symptoms among children in the overall sample and stratified by gender. The most prevalent symptoms were urinary urgency (22.7% of the children had symptoms almost always or always) and urinary retention maneuvers (occurring in 38.2% of the children). Females had more elimination dysfunction symptoms when compared to males (p<0.001).
Prevalence of urinary and bowel symptoms in children with and without enuresis from the 2004 cohort at 7 years of age stratified by gender.
| Variable | General | Male | General | Female | ||||
|---|---|---|---|---|---|---|---|---|
| Enuresis 11.8 | No enuresis 88.2 | p-value | Enuresis 9.3 | No enuresis 90.7 | p-value | |||
| Urinary incontinence | < 0.001 | < 0.001 | ||||||
| Never | 89.7 | 66.1 | 92.9 | 87.8 | 57.5 | 90.9 | ||
| Sometimes | 8.5 | 21.6 | 6.8 | 10.0 | 26.9 | 6.8 | ||
| Almost always | 0.8 | 4.6 | 0.2 | 1.3 | 7.5 | 0.2 | ||
| Always | 1.0 | 7.8 | 0.1 | 0.9 | 8.1 | 0.1 | ||
| Inadequate number of micturitions (< three or > eight/day) | 10.2 | 13.2 | 9.8 | 0.137 | 8.6 | 17.6 | 7.7 | < 0.001 |
| Retention maneuvers | < 0.001 | < 0.001 | ||||||
| Never | 67.2 | 60.5 | 68.0 | 52.6 | 43.4 | 53.5 | ||
| Sometimes | 24.8 | 25.1 | 24.7 | 33.4 | 35.2 | 33.3 | ||
| Almost always | 5.6 | 8.4 | 5.3 | 9.3 | 10.1 | 9.2 | ||
| Always | 2.4 | 6.1 | 2.0 | 4.7 | 11.3 | 4.1 | ||
| Urinary urgency | 0.002 | < 0.001 | ||||||
| Never | 26.2 | 22.2 | 26.7 | 24.6 | 16.5 | 25.4 | ||
| Sometimes | 51.7 | 45.4 | 52.6 | 51.0 | 46.8 | 51.1 | ||
| Almost always | 13.1 | 19.0 | 12.3 | 14.4 | 16.5 | 14.2 | ||
| Always | 9.0 | 13.4 | 8.4 | 10.3 | 20.3 | 9.3 | ||
| Encopresis | < 0.001 | < 0.001 | ||||||
| Never | 95.8 | 89.9 | 96.6 | 98.7 | 91.3 | 99.5 | ||
| Sometimes | 2.8 | 4.1 | 2.6 | 0.8 | 4.4 | 0.4 | ||
| Almost always | 0.6 | 0.9 | 0.6 | 0.4 | 0.6 | 0.1 | ||
| Never | 0.8 | 5.1 | 0.2 | 0.6 | 3.8 | 0.0 | ||
| Intervals >72hs to evacuate | 8.9 | 11.5 | 8.6 | 0.165 | 9.1 | 8.2 | 9.1 | 0.720 |
| Urinary symptom scorea | < 0.001 | < 0.001 | ||||||
| No symptoms | 17.2 | 10.8 | 19.1 | 16.0 | 8.3 | 16.8 | ||
| One symptom | 35.3 | 27.1 | 39.9 | 32.0 | 21.4 | 33.0 | ||
| Two symptoms | 33.5 | 35.5 | 30.5 | 36.2 | 35.2 | 36.3 | ||
| Three symptoms | 11.2 | 20.7 | 8.1 | 13.2 | 22.8 | 12.2 | ||
| Four or more symptoms | 2.8 | 5.9 | 2.6 | 2.6 | 12.4 | 1.6 | ||
Sometimes, up to 14 days during the month; Almost always, 15 to 29 days per month; Always, everyday.
Enuresis was ME in only 9.8% of children (10.8% males and 8.3% of females) (Table 2). Among the enuretic children, 37.4% had symptoms up to once a week; 32.9%, two to four times a week; and 26.2%, every day, with no difference between genders (p=0.134).
When comparing children with and without enuresis, urinary and intestinal symptoms were more frequent in children with enuresis, in both genders (Table 2). The frequency of daytime urinary incontinence was 4.8 times higher among enuretic males and 6 times higher among enuretic females when compared with their peers (Table 2). The daily frequency of urinary urgency or on most days of the month was also higher among enuretic children when compared to non-enuretic ones. Among males, there was no association between enuresis and urinary frequency or intervals greater than 72hours to evacuate. All urinary symptoms were more common in enuretic females when compared to non-enuretic.
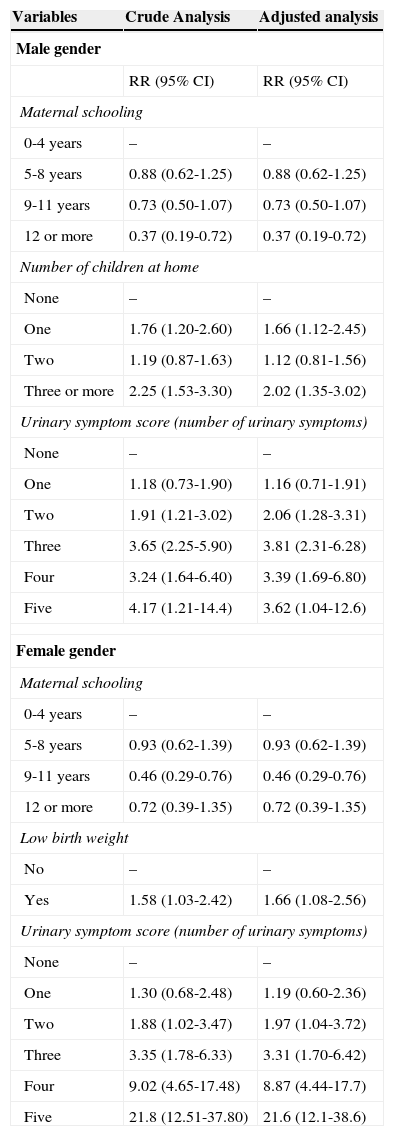
The multivariate analysis demonstrated that, in males (Table 3), the number of urinary symptoms and the number of children at home showed a direct association with the presence of enuresis, whereas maternal education was inversely related. In males, higher maternal education decreased the risk of enuresis and the higher number of urinary symptoms increased this risk; in females, the presence of urinary symptoms increased the chance of having more enuresis. Low birth weight was associated with more frequent bedwetting episodes only in females. Analyses with isolated symptoms present at 4 and 6 years showed an association of enuresis with urinary incontinence and urinary retention maneuvers, in both genders (data not shown).
Risk factors for enuresis using multivariate analysis (Poisson regression) and hierarchical model stratified by gender.
| Variables | Crude Analysis | Adjusted analysis |
|---|---|---|
| Male gender | ||
| RR (95% CI) | RR (95% CI) | |
| Maternal schooling | ||
| 0-4 years | – | – |
| 5-8 years | 0.88 (0.62-1.25) | 0.88 (0.62-1.25) |
| 9-11 years | 0.73 (0.50-1.07) | 0.73 (0.50-1.07) |
| 12 or more | 0.37 (0.19-0.72) | 0.37 (0.19-0.72) |
| Number of children at home | ||
| None | – | – |
| One | 1.76 (1.20-2.60) | 1.66 (1.12-2.45) |
| Two | 1.19 (0.87-1.63) | 1.12 (0.81-1.56) |
| Three or more | 2.25 (1.53-3.30) | 2.02 (1.35-3.02) |
| Urinary symptom score (number of urinary symptoms) | ||
| None | – | – |
| One | 1.18 (0.73-1.90) | 1.16 (0.71-1.91) |
| Two | 1.91 (1.21-3.02) | 2.06 (1.28-3.31) |
| Three | 3.65 (2.25-5.90) | 3.81 (2.31-6.28) |
| Four | 3.24 (1.64-6.40) | 3.39 (1.69-6.80) |
| Five | 4.17 (1.21-14.4) | 3.62 (1.04-12.6) |
| Female gender | ||
| Maternal schooling | ||
| 0-4 years | – | – |
| 5-8 years | 0.93 (0.62-1.39) | 0.93 (0.62-1.39) |
| 9-11 years | 0.46 (0.29-0.76) | 0.46 (0.29-0.76) |
| 12 or more | 0.72 (0.39-1.35) | 0.72 (0.39-1.35) |
| Low birth weight | ||
| No | – | – |
| Yes | 1.58 (1.03-2.42) | 1.66 (1.08-2.56) |
| Urinary symptom score (number of urinary symptoms) | ||
| None | – | – |
| One | 1.30 (0.68-2.48) | 1.19 (0.60-2.36) |
| Two | 1.88 (1.02-3.47) | 1.97 (1.04-3.72) |
| Three | 3.35 (1.78-6.33) | 3.31 (1.70-6.42) |
| Four | 9.02 (4.65-17.48) | 8.87 (4.44-17.7) |
| Five | 21.8 (12.51-37.80) | 21.6 (12.1-38.6) |
Poisson regression: In the first level, the variables education, age, ethnicity and maternal socioeconomic status; second level, prematurity, low birth weight, and number of children at home; third level, the scores of urinary symptoms and previous history of urinary tract infection. Variables with p<0.05 did not remain in the model.
CI, confidence interval.
Nocturnal enuresis is a type of morbidity that involves several physiopathologic mechanisms.5 This study sought to describe its occurrence, classification, and associated factors, without describing its physiopathology.5 The present study did not assess the familial occurrence of enuresis, which is an important factor for its occurrence,14,15 and whether these children had already sought treatment. The feelings of the children and their parents regarding symptoms were also not considered, which did not interfere with the present results, as they are important for the treatment, which was not the approach of this study.
One advantage of the present study is the fact that it was population-based and used a questionnaire with symptom definitions according to the International Children Continence Society (ICCS),15 providing information that can be compared to other studies.
The prevalence of enuresis is variable in the literature, especially due to the definitions used, in addition to cultural variations among the studied sites. Population-based studies conducted in Brazil and other countries are scarce, as most samples consist of ambulatory patients or schoolchildren. All analyzed studies demonstrated that the prevalence of enuresis decreased with age. The prevalence of enuresis in this study was 10.6%, which was higher among males, of whom 25% had urinary leakage every night. Mota, in a population-based study of Brazilian children aged 3 to 9 years, conducted in the same city, aiming to evaluate urinary symptoms, found a prevalence of enuresis in children older than 5 years of 20.1% in males and 15.1% in females.16
The prevalence of enuresis among the 8,242 children from the Avon Longitudinal Study of Parents and Children (ALSPAC) in England, assessed at age 7.5, was 2.6%, considering bedwetting two or more times a week, and 15.5% bedwetting less than twice a week, with a predominance of the male gender.17 In Turkey, three studies in schoolchildren, in different years, showed similar results.18–20
In 2007, Cuneyt assessed 1,500 schoolchildren and found a prevalence of enuresis of 22.2% in males and 18% in females aged 7 years, and 25.3% and 19.2% aged 8 years, respectively; among all children studied, 33.3% had symptoms every night.18 Gumus, in 1999, found a prevalence of 16.9% in males and 10.6% in females between 7 and 11 years,19 and, in 2004, Emel Gur observed a prevalence of 19.8% in children aged 6 to 10 years.20 In 7,012 Italian schoolchildren, the occurrence of enuresis was lower, 3.9%, with a predominance of males.21
In a study of schoolchildren from the Democratic Republic of the Congo, Central Africa, the prevalence was 34.5% at 7 years and 30% at 8 years, higher than that observed in European and American countries.22 In a sample of schoolchildren from Iran, the prevalence of enuresis between 5 and 7 years was 9% and between 8 and 10 years, of 6.9%. The frequency of over five nights a week was 3%, with no differences between the genders.23 In another study in Iranian schoolchildren aged 7 to 11 years, there was a prevalence of 18.7% with a predominance of males (20.9% vs. 16.5%); symptoms decreased as age increased.24
The concomitant occurrence of other lower urinary tract dysfunction symptoms is of utmost importance, as the physiopathological characteristics and therapeutic strategies differ from the management of ME enuresis. Most children had NME enuresis (85%), which has been also observed in current studies.16,18,19 The most frequently reported urinary symptoms were retention maneuvers and urinary urgency. These symptoms may be associated with dysfunctions of the lower urinary tract, especially hyperactive bladder,2 which needs to be managed before the treatment of enuresis.
Enuresis is a common pathology in children from families with low educational and socioeconomic status. It may cause secondary psychological disorders and problems of social and familial adaptation. The highest prevalence of enuresis was observed in children of mothers with lower education levels, of lower socioeconomic status, and in families with more children, demonstrating a significant variation between different social levels. The studies by Cuneyt, Gumus, Emel Gur, and Chiozza had similar findings, with a direct association between enuresis and more numerous families with lower level of schooling.18–21
The initial evaluation of enuretic children can be conducted through a detailed history and physical examination, without the need for laboratory or invasive tests.25 The evaluation of other urinary and intestinal symptoms forms this detailed history and is necessary for the classification of enuresis, as well as for therapeutic guidance. The urinary symptom score16,26 was shown to be a good tool for adequate evaluation of the urinary pattern and has been used in other studies.16,26–28
Child health monitoring is a unique opportunity for the pediatrician to prevent, diagnose, and treat childhood morbidities. Enuresis and its associated symptoms are prevalent and should be investigated in clinical practice, especially in children of lower socioeconomic status.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Mota DM, Barros AJ, Matijasevich A, Santos IS. Prevalence of enuresis and urinary symptoms at age 7 years in the 2004 birth cohort from Pelotas, Brazil. J Pediatr (Rio J). 2015;91:52–8.