To analyze the performance of three different diagnostic criteria of overweight and obesity (WHO, IOTF and Conde and Monteiro) using body mass index (BMI) as predictors of metabolic syndrome (MetS) in a representative sample of adolescents.
MethodsA sample of 1035 adolescents aged 12–20 years (565 girls and 470 boys) was used in the study. BMI was calculated through the quotient of weight (kg)/height squared (m)2, and MetS was defined according to the criteria of the International Diabetes Federation. Sensitivity, specificity, and overall accuracy (area under the curve) were estimated using the receiver operating characteristic (ROC) curves method and used to describe the predictive performance.
ResultsThe three diagnostic criteria showed higher absolute values of sensitivity and specificity for predicting MetS in boys and older adolescents. The highest sensitivity to identify MetS was found using the IOTF criterion (60–85%), while specificity values ≥ 90% were found for the three criteria. The Conde and Monteiro diagnostic criterion pointed to a significantly lower overall accuracy (0.52–0.64) than that of the WHO (0.70–0.84) and IOTF (0.75–0.89) diagnostic criterion.
ConclusionsOverweight and obesity using BMI showed a moderate association with MetS, regardless of the diagnostic criteria used. However, the IOTF criterion showed better predictive capacity for the presence of MetS than the WHO and the Conde and Monteiro criteria.
Analisar o desempenho de três diferentes critérios diagnósticos de sobrepeso e obesidade (WHO, IOTF e Conde & Monteiro) a partir do índice de massa corporal (IMC) como preditores da síndrome metabólica (SMet) em amostra representativa de adolescentes.
MétodosA amostra foi constituída por 1035 adolescentes (565 moças e 470 rapazes) com idades entre 12 e 20 anos. O IMC foi calculado mediante quociente entre peso (kg)/altura (m)2 e SMet foi definida através dos critérios da International Diabetes Federation. Desempenho preditivo foi descrito a partir das estimativas de sensibilidade, especificidade e acurácia global (área sob a curva) utilizando-se do método de curvas Receiver Operating Characteristic.
ResultadosOs três critérios diagnóstico apresentaram maiores valores absolutos de sensibilidade e especificidade para predição da SMet nos rapazes e nos adolescentes com mais idade. Maior sensibilidade para identificar SMet foi observada utilizando o critério IOTF (60% a 85%), enquanto especificidade ≥ 90% foi observada mediante o uso dos três critérios diagnósticos. O critério diagnóstico Conde & Monteiro apontou acurácia global (0,52 a 0,64) significativamente menor que os critérios diagnósticos WHO (0,70 a 0,84) e IOTF (0,75 a 0,89).
ConclusõesSobrepeso e obesidade a partir do IMC mostrou uma moderada associação com SMet, independentemente do critério diagnóstico empregado. Contudo, o critério IOTF demonstrou melhor capacidade preditiva para presença de SMet que os critérios WHO e Conde & Monteiro.
Currently, regardless of gender, age, socioeconomic stratum, and geographical region, overweight and obesity have become a global epidemic,1 which definitively contributes to the onset of cardiovascular risk biomarkers.2 In recent years, there have been significant changes in the understanding of biomarkers implicated in the pathogenesis of cardiovascular diseases, including the identification of proinflammatory and anti-inflammatory cytokines, adipokines, chemokines, inflammatory indicators derived from hepatocytes, and some specific enzymes.3 However, at young ages, the use of the so-called traditional risk biomarkers still prevails, with emphasis on metabolic syndrome (MetS).4–6
Nonetheless, the complexity of the procedures necessary to identify MetS makes it difficult to include them in routines for health status monitoring in young individuals, which require alternatives that are more practical and of immediate use. In this sense, previous studies presented evidence that overweight and obesity, identified through the body mass index (BMI), are defined as possible predictors of MetS.7–9 Therefore, adequate classification of overweight and obesity may constitute an important complementary screening tool for the presence of MetS in children and adolescents.
The use of a diagnostic criterion of overweight and obesity based on BMI to screen MetS in adolescents is justified, as it is an accessible and easy-to-use alternative, which has immediate interpretation and good cost-effectiveness. However, it does not seek to replace medical intervention at any time, since it does not exclude the need to monitor the individual components to confirm the MetS diagnosis. A screening process, when performed in environments with high concentrations of young individuals, such as schools, reaches a high number of adolescents, especially those who have difficulty access to or do not seek the health system. Therefore, once the adolescents most likely to have MetS have been identified, they can be referred for specialized medical follow-up.
There is a consensus regarding the diagnostic criteria to classify overweight and obesity in adults based on BMI; however, this is not the case for children and adolescents. Considering the implications related to the processes of physical growth and biological maturation that start at this stage of development, the significance of BMI for the health of young individuals calls for more complex differentiations than those attributed to adults. In this case, different diagnostic criteria based on BMI have been proposed and have been used to identify excess body weight in young individuals. In the international context, the criteria set forth by=the World Health Organization (WHO)10,11 and the International Obesity Task Force (IOTF)12,13 stand out, whereas the proposal of Conde and Monteiro14 has received special attention for the specific use in the young Brazilian population. However, there is no consensus on the proposal to be used and, therefore, there are discussions about the validity of each diagnostic criterion when used in specific populations.
Therefore, the aim of the present study was to analyze the performance of the three different diagnostic criteria for overweight and obesity based on BMI (WHO, IOTF, Conde and Monteiro) as predictors of MetS in a representative sample of adolescents.
MethodsThe study is linked to a larger project, which aimed to estimate the prevalence of MetS and associated factors in adolescents. For that purpose, a population-based cross-sectional study was carried out in students from the city of Jacarezinho, state of Paraná, Brazil. Data collection was carried out from August to November 2014. The intervention protocols used in the study were approved by the Research Ethics Committee of Universidade do Paraná – UNOPAR (Opinion n. 1,302,963).
Sample and subject selectionThe reference population included adolescents of both genders, aged 12 to 20 years, enrolled in public and private elementary schools (6th to 9th grade) and high school (1st to 3rd year). Initially, the sample size was established to meet the objective of estimating the prevalence of MetS and associated factors, assuming a 95% confidence interval, a sampling error of 3 percentage points, an increase of 10% for possible losses and, as the sample planning involved conglomerates (school structure, gender, school shift and school year), a design effect (deff) equal to 1.5 was added.
According to the procedures used to calculate sample size in studies involving diagnostic tests,15 it was verified that this sample, which included 1035 adolescents, allowed the adequate identification of sensitivity and specificity. The sample's statistical power, stratified by gender (565 girls and 470 boys), was calculated a posteriori and allows to consider, with 80% power and 5% significance, areas under the receiver operating characteristic (ROC) curve of at least 0.53 and 0.56 for girls and boys, respectively.
Data collectionChronological age was established in years and months, based on the comparison between the data collection date and birth date. However, for the analysis of data, two age groups were established: 12–15 years and 16–20 years.
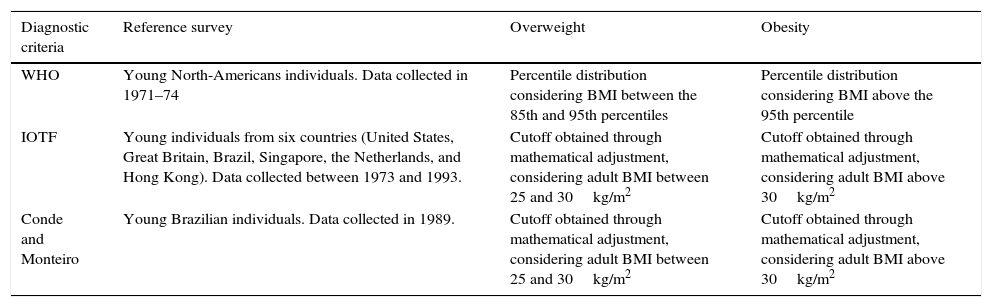
BMI was calculated using the ratio between body weight in kilograms and height expressed in meters squared (kg/m2), based on the procedures of the World Health Organization.16 Overweight and obesity were identified using the three specific diagnostic criteria for gender and age: WHO,11 IOTF,13 and Conde and Monteiro,14 as explained in Table 1.
Diagnostic criteria for identifying excess body weight in young individuals based on body mass index (BMI) according to the World Health Organization (WHO), International Obesity Task Force (IOTF) and Conde and Monteiro.
| Diagnostic criteria | Reference survey | Overweight | Obesity |
|---|---|---|---|
| WHO | Young North-Americans individuals. Data collected in 1971–74 | Percentile distribution considering BMI between the 85th and 95th percentiles | Percentile distribution considering BMI above the 95th percentile |
| IOTF | Young individuals from six countries (United States, Great Britain, Brazil, Singapore, the Netherlands, and Hong Kong). Data collected between 1973 and 1993. | Cutoff obtained through mathematical adjustment, considering adult BMI between 25 and 30kg/m2 | Cutoff obtained through mathematical adjustment, considering adult BMI above 30kg/m2 |
| Conde and Monteiro | Young Brazilian individuals. Data collected in 1989. | Cutoff obtained through mathematical adjustment, considering adult BMI between 25 and 30kg/m2 | Cutoff obtained through mathematical adjustment, considering adult BMI above 30kg/m2 |
MetS was identified by analyzing the blood content of plasma lipids (triglycerides and high-density lipoproteins – HDL-cholesterol) and blood glucose, resting blood pressure (systolic and diastolic), and abdominal fat accumulation (waist circumference), according to the criteria proposed by the International Diabetes Federation (IDF).17 In this case, MetS was defined as the mandatory presence of elevated waist circumference (<16 years: both genders ≥ 90th percentile; ≥ 16 years: boys ≥ 90cm and girls ≥ 80cm) and at least two other altered components: increased triglycerides (≥150mg/dL), decreased HDL-cholesterol (<16 years: both genders<40mg/dL; ≥16 years: boys<40mg/dL and girls<50mg/dL), elevated fasting blood glucose (≥100mg/dL), and altered blood pressure (systolic ≥ 130mmHg or diastolic ≥ 85mmHg).
The measurements of plasma lipids and glycemia were carried out in blood samples collected by venipuncture after 12h of fasting, according to conventional laboratory techniques. Systolic and diastolic blood pressure levels were measured through the auscultatory method using a mercury sphygmomanometer, with the adolescent in the sitting position, after a minimum of 5min of rest. Two measurements were performed, considering the mean value of both measures for calculation purposes. Waist circumference measurements were made at the midpoint between the last rib and the iliac crest, using an inextensible anthropometric tape.
Statistical analysisThe statistical analysis was performed using SPSS software, version 22 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, NY, USA). Point proportions and their respective 95% confidence intervals were calculated for the outcomes of interest (overweight, obesity, and MetS), and were stratified for gender and age. Statistical differences between the strata investigated were analyzed with the chi-squared test (χ2) for linear trends. The performance of the three diagnostic criteria for overweight and obesity (WHO, IOTF, and Conde and Monteiro) as predictors of MetS was analyzed using sensitivity, specificity, and global accuracy properties, identified by the ROC curve method together with their 95% confidence intervals.18 Possible significant differences related to the sensitivity, specificity, and overall accuracy properties were identified using McNemar (χ2) statistics.19
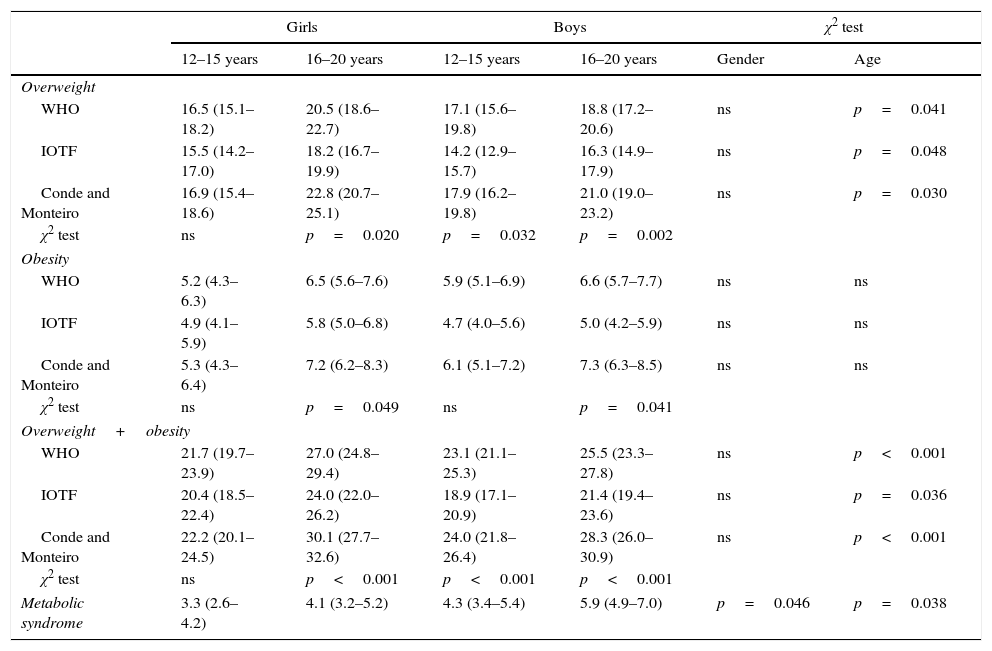
ResultsTable 2 shows the prevalence rates of overweight, obesity, and MetS in the adolescent population analyzed in the study. The highest prevalence rates were observed using the diagnostic criterion by Conde and Monteiro, mainly in adolescents aged between 16 and 20 years. Conversely, the IOTF diagnostic criterion indicated significantly lower prevalence rates, especially in boys. MetS was identified in 4.5% (95%CI: 3.8–5.4) of the sample, being significantly higher in boys and older adolescents.
Prevalence rates (95% confidence interval) of overweight and obesity estimated by the three diagnostic criteria and metabolic syndrome in the population of adolescent students analyzed in the study.
| Girls | Boys | χ2 test | ||||
|---|---|---|---|---|---|---|
| 12–15 years | 16–20 years | 12–15 years | 16–20 years | Gender | Age | |
| Overweight | ||||||
| WHO | 16.5 (15.1–18.2) | 20.5 (18.6–22.7) | 17.1 (15.6–19.8) | 18.8 (17.2–20.6) | ns | p=0.041 |
| IOTF | 15.5 (14.2–17.0) | 18.2 (16.7–19.9) | 14.2 (12.9–15.7) | 16.3 (14.9–17.9) | ns | p=0.048 |
| Conde and Monteiro | 16.9 (15.4–18.6) | 22.8 (20.7–25.1) | 17.9 (16.2–19.8) | 21.0 (19.0–23.2) | ns | p=0.030 |
| χ2 test | ns | p=0.020 | p=0.032 | p=0.002 | ||
| Obesity | ||||||
| WHO | 5.2 (4.3–6.3) | 6.5 (5.6–7.6) | 5.9 (5.1–6.9) | 6.6 (5.7–7.7) | ns | ns |
| IOTF | 4.9 (4.1–5.9) | 5.8 (5.0–6.8) | 4.7 (4.0–5.6) | 5.0 (4.2–5.9) | ns | ns |
| Conde and Monteiro | 5.3 (4.3–6.4) | 7.2 (6.2–8.3) | 6.1 (5.1–7.2) | 7.3 (6.3–8.5) | ns | ns |
| χ2 test | ns | p=0.049 | ns | p=0.041 | ||
| Overweight+obesity | ||||||
| WHO | 21.7 (19.7–23.9) | 27.0 (24.8–29.4) | 23.1 (21.1–25.3) | 25.5 (23.3–27.8) | ns | p<0.001 |
| IOTF | 20.4 (18.5–22.4) | 24.0 (22.0–26.2) | 18.9 (17.1–20.9) | 21.4 (19.4–23.6) | ns | p=0.036 |
| Conde and Monteiro | 22.2 (20.1–24.5) | 30.1 (27.7–32.6) | 24.0 (21.8–26.4) | 28.3 (26.0–30.9) | ns | p<0.001 |
| χ2 test | ns | p<0.001 | p<0.001 | p<0.001 | ||
| Metabolic syndrome | 3.3 (2.6–4.2) | 4.1 (3.2–5.2) | 4.3 (3.4–5.4) | 5.9 (4.9–7.0) | p=0.046 | p=0.038 |
WHO, World Health Organization; IOTF, International Obesity Task Force.
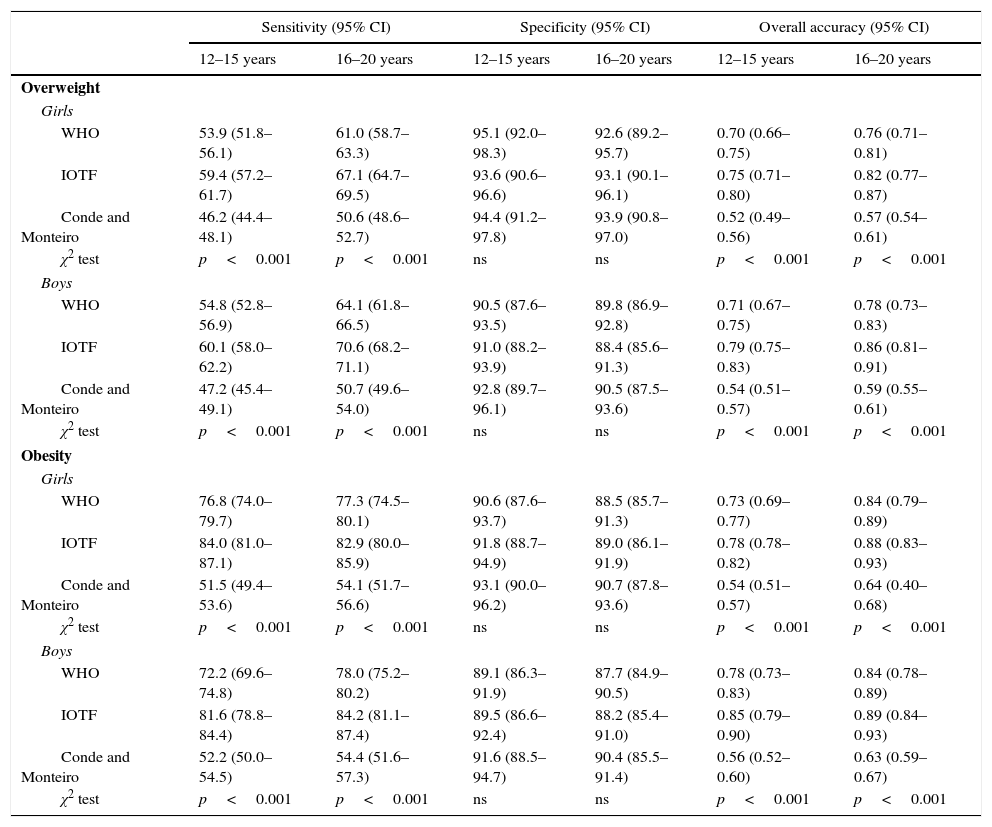
The performance of the three diagnostic criteria for overweight and obesity as predictors of MetS is shown in Table 3. Overall, both overweight and obesity showed similar sensitivity in both genders; however, higher values were observed in older adolescents. As for specificity, there was a tendency for the values observed in girls to stand out when compared with those observed in boys, with no important significant in relation to age.
Performance of WHO, IOTF, and Conde and Monteiro diagnostic criteria of overweight and obesity as metabolic syndrome predictors.
| Sensitivity (95% CI) | Specificity (95% CI) | Overall accuracy (95% CI) | ||||
|---|---|---|---|---|---|---|
| 12–15 years | 16–20 years | 12–15 years | 16–20 years | 12–15 years | 16–20 years | |
| Overweight | ||||||
| Girls | ||||||
| WHO | 53.9 (51.8–56.1) | 61.0 (58.7–63.3) | 95.1 (92.0–98.3) | 92.6 (89.2–95.7) | 0.70 (0.66–0.75) | 0.76 (0.71–0.81) |
| IOTF | 59.4 (57.2–61.7) | 67.1 (64.7–69.5) | 93.6 (90.6–96.6) | 93.1 (90.1–96.1) | 0.75 (0.71–0.80) | 0.82 (0.77–0.87) |
| Conde and Monteiro | 46.2 (44.4–48.1) | 50.6 (48.6–52.7) | 94.4 (91.2–97.8) | 93.9 (90.8–97.0) | 0.52 (0.49–0.56) | 0.57 (0.54–0.61) |
| χ2 test | p<0.001 | p<0.001 | ns | ns | p<0.001 | p<0.001 |
| Boys | ||||||
| WHO | 54.8 (52.8–56.9) | 64.1 (61.8–66.5) | 90.5 (87.6–93.5) | 89.8 (86.9–92.8) | 0.71 (0.67–0.75) | 0.78 (0.73–0.83) |
| IOTF | 60.1 (58.0–62.2) | 70.6 (68.2–71.1) | 91.0 (88.2–93.9) | 88.4 (85.6–91.3) | 0.79 (0.75–0.83) | 0.86 (0.81–0.91) |
| Conde and Monteiro | 47.2 (45.4–49.1) | 50.7 (49.6–54.0) | 92.8 (89.7–96.1) | 90.5 (87.5–93.6) | 0.54 (0.51–0.57) | 0.59 (0.55–0.61) |
| χ2 test | p<0.001 | p<0.001 | ns | ns | p<0.001 | p<0.001 |
| Obesity | ||||||
| Girls | ||||||
| WHO | 76.8 (74.0–79.7) | 77.3 (74.5–80.1) | 90.6 (87.6–93.7) | 88.5 (85.7–91.3) | 0.73 (0.69–0.77) | 0.84 (0.79–0.89) |
| IOTF | 84.0 (81.0–87.1) | 82.9 (80.0–85.9) | 91.8 (88.7–94.9) | 89.0 (86.1–91.9) | 0.78 (0.78–0.82) | 0.88 (0.83–0.93) |
| Conde and Monteiro | 51.5 (49.4–53.6) | 54.1 (51.7–56.6) | 93.1 (90.0–96.2) | 90.7 (87.8–93.6) | 0.54 (0.51–0.57) | 0.64 (0.40–0.68) |
| χ2 test | p<0.001 | p<0.001 | ns | ns | p<0.001 | p<0.001 |
| Boys | ||||||
| WHO | 72.2 (69.6–74.8) | 78.0 (75.2–80.2) | 89.1 (86.3–91.9) | 87.7 (84.9–90.5) | 0.78 (0.73–0.83) | 0.84 (0.78–0.89) |
| IOTF | 81.6 (78.8–84.4) | 84.2 (81.1–87.4) | 89.5 (86.6–92.4) | 88.2 (85.4–91.0) | 0.85 (0.79–0.90) | 0.89 (0.84–0.93) |
| Conde and Monteiro | 52.2 (50.0–54.5) | 54.4 (51.6–57.3) | 91.6 (88.5–94.7) | 90.4 (85.5–91.4) | 0.56 (0.52–0.60) | 0.63 (0.59–0.67) |
| χ2 test | p<0.001 | p<0.001 | ns | ns | p<0.001 | p<0.001 |
WHO, World Health Organization; IOTF, International Obesity Task Force.
In both genders, regardless of age and the three diagnostic criteria, the sensitivity for obesity was higher, while greater specificity was observed for overweight. In all assessed strata, the IOTF diagnostic criterion showed the highest sensitivity. In turn, the lowest sensitivity was observed when using the Conde and Monteiro diagnostic criterion. As for specificity, the three diagnostic criteria showed similar values, close to 90%.
Regarding the overall accuracy property, which ranged between 0.52 and 0.89, differences between age ranges were more pronounced than between genders. Regarding the diagnostic criteria, the Conde and Monteiro proposal showed a significantly lower global accuracy than the WHO and IOTF proposals. The use of the diagnostic criterion by Conde and Monteiro showed values ≤ 0.69, which suggests low overall accuracy. In turn, the use of the WHO and IOTF diagnostic criteria showed values between 0.70 and 0.89, with a significant advantage for the IOTF criterion, thus showing moderate global accuracy.
DiscussionRegardless of the diagnostic criteria used, one in four adolescents analyzed in the study had excess body weight (≈25%). This proportion is similar to that found in a representative study of a group of medium-sized and large Brazilian municipalities20; however, slightly lower than that of developed countries and approximately twice as high as that observed in the young population of developing countries.1 Using the same diagnostic criteria (IDF), the proportion of adolescents with MetS is higher than that recently observed in the young Brazilian population (4.5% vs. 2.6%)21; however, it is lower than that described in North-American and European adolescents.22
O diagnostic criterion by Conde and Monteiro showed the lowest capacity to discriminate between adolescents who had MetS and those who did not. Global accuracy estimates showed that the chances of correctly identifying the presence of MetS when using this diagnostic criterion were close to 50–60% (area under the ROC curve between 0.52 and 0.64). In this context, if, on the one hand, the specificities obtained when using the Conde and Monteiro diagnostic criterion showed values ≥ 90%, on the other hand, the sensitivities did not exceed 55%. Therefore, when using this diagnostic criterion to identify MetS, there is a high probability that adolescents with normal weight will be identified as not having MetS; however, the chance of detecting MetS markedly decreases in adolescents who are overweight or obese.
The predictive capacities of the WHO and IOTF diagnostic criteria for the presence of MetS were shown to be higher and with lower differences between them; however, the IOTF diagnostic criterion showed significantly higher sensitivity than the WHO and the Conde and Monteiro criteria. In this sense, the use of the IOTF diagnostic criteria to correctly identify MetS resulted in 5–10% and 13–22% fewer false-negative cases than the WHO and the Conde and Monteiro diagnostic criteria, respectively. In probabilistic values, using the WHO and IOTF diagnostic criteria, out of ten adolescents with excess body weight, there were also indications that approximately seven to nine of them were correctly identified as having MetS (area under the ROC curve between 0.70 and 0.89).
In general, when considering the three diagnostic criteria as MetS predictors, a lower overall accuracy was observed for girls and adolescents aged 12–15 years. This fact may likely reflect the pubertal growth spurt that occurs at this age, especially among the girls. In this case, due to differences in the timing of puberty, there is a higher variability in the association between body fat accumulation, fat-free mass proportion, and changes in BMI values, which directly affects the identification of overweight and obesity.23
Although significant differences were found related to the sensitivity, specificity, and overall accuracy properties, the findings of the present study confirmed that the three diagnostic criteria are capable of predicting MetS, with more adequate validity indicators in obese adolescents. In this context, it is important to mention that the three diagnostic criteria have the use of arbitrary cutoffs in common, based mainly on statistical assumptions. Therefore, these differences may be explained in part by the different methodologies used in their propositions and, mainly, by the prevalence rates of overweight and obesity and the secular tendency of BMI of the reference population used for the sample data set.
The WHO proposal is based on data from young North-American individuals collected from 1971 to 1974; it was recently reprocessed to attenuate limitations detected in a previous proposal.11 While there may be evidence that the prevalence of overweight and obesity in the young population of the United States showed a stabilizing tendency in the last decade, this is not the case when comparing data from the 1970s and from more recent generations.24
In turn, the IOTF proposal originates from representative national surveys of young individuals from six countries (United States, Great Britain, Brazil, Singapore, the Netherlands, and Hong Kong). The surveys were carried out at different times between 1973 and 1993,12,13 which hinders the analysis of the secular trend of BMI when proposing this diagnostic criterion. The Conde and Monteiro proposal used data extracted from the National Health and Nutrition Survey, involving a nationally representative sample of young Brazilian individuals.14 Data were collected in 1989, when the prevalence of overweight and obesity in the young Brazilian population was significantly lower than in the present day.20
Furthermore, when selecting a specific diagnostic criterion, it is prudent to consider the influence of ethnic components. In this sense, for use in Brazilian adolescents, the Conde and Monteiro diagnostic criterion initially showed great advantage and, in contrast, even considering the multiethnic profile of the young American population, an important limitation should be accounted for when choosing the WHO diagnostic criteria. The IOTF diagnostic criterion appears to be more adequate to ensure a multiethnic application, as it is based on data from six countries, including Brazil.
Regarding the different methodologies used to identify cutoffs, the WHO proposal used probabilistic resources in which BMI values equivalent to the 85th and 95th percentiles were used to identify overweight and obese adolescents, respectively. Therefore, it was assumed that, in the reference population, regardless of any additional information, exactly 15% of the young individuals of each gender and age were overweight and 5% were obese. An important limitation of this methodology is that it considers that higher BMI values in the percentile distribution of the reference population may represent the presence of overweight and obesity, rather than just identifying individuals who are heavier in comparison to their peers.
In contrast, the IOTF and the Conde and Monteiro proposals were created independently from the BMI percentile distribution in the reference population. In these cases, the cutoffs were defined using epidemiological criteria, based on adjustments of specific mathematical models for gender and age, in which at age of 18 years there was an interception with BMI values representative of increased risk for the presence of health outcomes in early adulthood, as a consequence of overweight and obesity, i.e., 25kg/m2 and 30kg/m2, respectively. However, the methodological procedure used by the two proposals is not free of criticism. Although they do not depend on the percentile distribution, it was assumed that the proportion of young individuals in the reference population with overweight and obesity was the same in both genders and at all ages.
The present study results corroborate findings available in the literature that indicate high specificity accompanied by reasonable sensitivity to identify cardiometabolic risk in young individuals using diagnostic criteria based on the BMI.7–9 However, it partially disagrees with the results found in a study of Brazilian children that sought to identify the predictive capacity of diagnostic criteria, specifically for the presence of high blood pressure.25 The study showed indicators equivalent to overall accuracy that were similar to the diagnostic criteria by Conde and Monteiro and by the IOTF. Possibly, the isolated use of the high blood pressure component, rather than the conglomerate of components that defines MetS, and the younger age of the study subjects (children between 6 and 13 years of age) can explain possible divergences between both studies.
The present study has some limitations that should be considered. Even assuming the low rate of refusal to undergo the measurements (≈8%), the possibility of selection bias cannot be ruled out, since it was not possible to compare data from the adolescents that participated and those who did not participate in the study. It is also important to mention that, because there is no universal criterion to define MetS, the authors chose to use criteria proposed by the IDF and, in this sense, MetS prevalence estimates may vary according to the used criteria.26,27
In conclusion, evidence found in the study contribute to the knowledge of the area, showing that, of the three diagnostic criteria of overweight and obesity based on BMI (WHO, IOTF, and Conde and Monteiro), the IOTF diagnostic criterion showed a significantly higher predictive capacity for the presence of MetS. However, since BMI is an important predictor of the presence of MetS in adolescents, the major challenge remains to adjust cutoffs that can minimize the number of false-negative results (higher sensitivity indices) and maximize the amount of true-negative cases (higher specificity indices), as previously observed in the three diagnostic criteria considered in the study.
FundingDartagnan Pinto Guedes is a Research Productivity Fellow at CNPq.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Oliveira RG, Guedes DP. Performance of different diagnostic criteria of overweight and obesity as predictors of metabolic syndrome in adolescents. J Pediatr (Rio J). 2017;93:525–31.