To compare the use of analgesia versus neonatologists’ perception regarding analgesic use in painful procedures in the years 2001, 2006, and 2011.
MethodsThis was a prospective cohort study of all newborns admitted to four university neonatal intensive care units during one month in 2001, 2006, and 2011. The frequency of analgesic prescription for painful procedures was evaluated. Of the 202 neonatologists, 188 answered a questionnaire giving their opinion on the intensity of pain during lumbar puncture, tracheal intubation, mechanical ventilation, and postoperative period using a 10-cm visual analogic scale (VAS; pain >3cm).
ResultsFor lumbar puncture, 12% (2001), 43% (2006), and 36% (2011) were performed using analgesia. Among the neonatologists, 40–50% reported VAS >3 for lumbar puncture in all study periods. For intubation, 30% received analgesia in the study periods, and 35% (2001), 55% (2006), and 73% (2011) of the neonatologists reported VAS >3 and would prescribe analgesia for this procedure. As for mechanical ventilation, 45% (2001), 64% (2006), and 48% (2011) of patient-days were under analgesia; 56% (2001), 57% (2006), and 26% (2011) of neonatologists reported VAS >3 and said they would use analgesia during mechanical ventilation. For the first three post-operative days, 37% (2001), 78% (2006), and 89% (2011) of the patients received analgesia and more than 90% of neonatologists reported VAS >3 for major surgeries.
ConclusionsDespite an increase in the medical perception of neonatal pain and in analgesic use during painful procedures, the gap between clinical practice and neonatologist perception of analgesia need did not change during the ten-year period.
Confrontar o uso de analgesia versus a percepção de neonatologistas quanto ao emprego de analgésicos para procedimentos dolorosos nos anos de 2001, 2006 e 2011.
MétodosCoorte prospectiva de todos recém-nascidos internados em quatro unidades universitárias. Avaliou-se a frequência do emprego de analgésicos para procedimentos dolorosos por um mês dos anos de estudo. Dos 202 neonatologistas atuantes nas unidades nos três períodos, 188 assinalaram em escala analógica visual de 10cm (dor >3cm) a intensidade da dor sentida pelo recém-nascido na punção lombar, intubação traqueal, ventilação mecânica e pós-operatório.
ResultadosPara PL, 12%, 43% e 36% foram realizadas com analgesia em 2001, 2006 e 2011 e 40-50% dos neonatologistas referiam indicar analgésicos na punção lombar nos três períodos. Na intubação, 30% foram realizadas sob analgesia nos três períodos e 35% (2001), 55% (2006) e 73% (2011) dos médicos diziam indicar analgésicos. Quanto à ventilação mecânica, 45-64% dos ventilados-dia estavam sob analgesia nos três períodos e 56% (2001), 57% (2006) e 26% (2011) dos neonatologistas diziam usar analgésicos. Dos pacientes-dia nos três primeiros dias de pós-operatório, 37% (2001), 78% (2006) e 89% (2011) receberam alguma dose de analgésico, sendo que mais de 90% dos médicos referiam usar analgesia para essa situação.
ConclusõesEntre 2001 e 2011, ocorreu aumento no uso de analgésicos para procedimentos dolorosos nas unidades neonatais e uma percepção mais acentuada por parte dos médicos de que o recém-nascido sente dor, mas o lapso entre a prática clínica e a percepção médica quanto à presença de dor persistiu.
Painful events are common in newborns who require intensive care. Simons et al.1 observed 151 newborns in the first 14 days of admission to the intensive care unit (ICU) and each was submitted to an average of 14 painful procedures a day. Prestes et al.2 verified that three to five potentially painful procedures were performed per patient/day in university neonatal units in São Paulo. Carbajal et al.3 assessed 430 newborns in the Paris region in the first 14 days of life and observed, on average, ten painful procedures a day. Cignacco et al.4 studied 120 infants on mechanical ventilation during the first 14 days of life in two Swiss units and found 23 painful procedures/day per patient.
Despite this scenario, the use of measures to relieve the pain during potentially painful procedures is unusual, and it is estimated that only 3% of newborns receive specific analgesia for the procedure and that, in 30%, adjuvant techniques are applied to minimize pain.1–3 In Italy, five years after the publication of a national guide for pain control and prevention, Lake et al. analyzed 103 NICUs and observed that routine analgesic administration occurred in 34% of the units for tracheal intubation, 47% for mechanical ventilation, 33% for lumbar puncture, and 64% for postoperative pain.5
Therefore, a paradox is observed between the frequency of conditions that cause pain in critically ill neonates and the use of analgesia in neonatal units. The most often cited causes for this paradox are the several myths surrounding the painful experience in the neonatal population, particularly the perception that the newborn is too immature to feel pain.6–8 It is known that the knowledge about the presence of pain in newborns has greatly increased among health professionals responsible for neonatal care,9 but it is not known how each professional puts such knowledge into practice.
The aim of this study was to compare the perception of physicians working in university neonatal intensive care units (NICUs) regarding the painful procedures and the analgesia versus the use of analgesics for potentially painful procedures performed in critically ill newborns in these units, in three different times over a ten-year period.
MethodsThis was a multicenter observational study consisting of three prospective cohorts of all newborns admitted to four university NICUs and the neonatologists working in these units within the period of October 1st to 31st of the years 2001, 2006, and 2011. The choice of month and the year 2001 was for convenience, and the repetition every five years was considered because close to 100% of medical knowledge is renewed every ten years, with an obsolescence rate of medical journals of about 50% every five years.
The following neonatal units were assessed: Faculdade de Ciências Médicas da Santa Casa de São Paulo, Universidade Estadual de Campinas, Universidade Estadual Paulista Júlio de Mesquita Filho, and Universidade Federal de São Paulo–Escola Paulista de Medicina. The research protocol was approved by the Research Ethics Committee of each institution. The need for informed consent from newborns’ family members was waived. Each participating physician signed an informed consent form.
All neonates admitted to the four units were included, according to the criteria of the intensive care of each of them. In order to answer the pain perception questionnaire, the inclusion criterion was to be a physician at one of the participating units, with power to make clinical decisions. Residents from the pediatrics and neonatology units were not included.
The head of the neonatal intensive care unit of each institution filled out a questionnaire with information about the general characteristics of the unit, presence of routine assessment, treatment, and education on pain and analgesia in the neonatal period.
Data collection of the hospitalized newborns was carried out by a neonatologist of each institution. Information on the total number of patients and patient-days in each unit were obtained. The performed painful procedures were registered in a medical file at the bedside, filled by doctors and nurses who cared for the patients. For the present study, the following procedures were considered: lumbar puncture, tracheal intubation, time of mechanical ventilation, and postoperative period. The same team of researchers collected data in the three study periods.
To evaluate the use of analgesics in newborns in the three periods of the study, the following data were analyzed: patient-days on analgesia (sum of all patients who received at least one dose of analgesic for each day of the study); number of lumbar puncture and tracheal intubation procedures under analgesia for each day of the evaluated month and year; postoperative period under analgesia (it was verified, at each day of the study, which patients were receiving any dose of analgesia on the three first days after some surgical procedure), and ventilation-days (sum of patients undergoing mechanical ventilation in every day of the study, whether under analgesia or not).
All physicians who worked at the university neonatal units answered an anonymous questionnaire, which consisted of personal characteristics, knowledge regarding pain assessment, and personal opinion about the aspects related to pain in invasive procedures. In this regard, the physician was asked regarding whether newborns feel pain during lumbar puncture, intubation, mechanical ventilation, and in the postoperative period of minor (inguinal hernia repair) and major (laparotomy) surgeries. If the answer was positive, the professional was asked to state how much pain he thought the newborn felt in each procedure using a 10-cm horizontal visual analogic scale (VAS). Such a scale ranged from no pain (zero) to severe pain (10cm); pain was considered to be present when the marked distance was greater than 3.0cm.10 Each physician was also asked whether he/she thought it was adequate to prescribe analgesia for the above procedures; the only possible answers were yes or no.
Data were compared in the three study periods by descriptive analysis, using Pearson's partitioning chi-squared test for categorical variables, or Fisher's exact test. For the quantitative variables, comparison was made by analysis of variance with Tukey's post hoc test. As all patients admitted to the four units and all physicians from each of the units in three periods of the study were analyzed, the sample post hoc power was verified only for the number of painful procedures performed under analgesia. The SPSS software for Windows, version 19 (Statistical Package for Social Sciences, Chicago, IL, USA) was used for the statistical analysis.
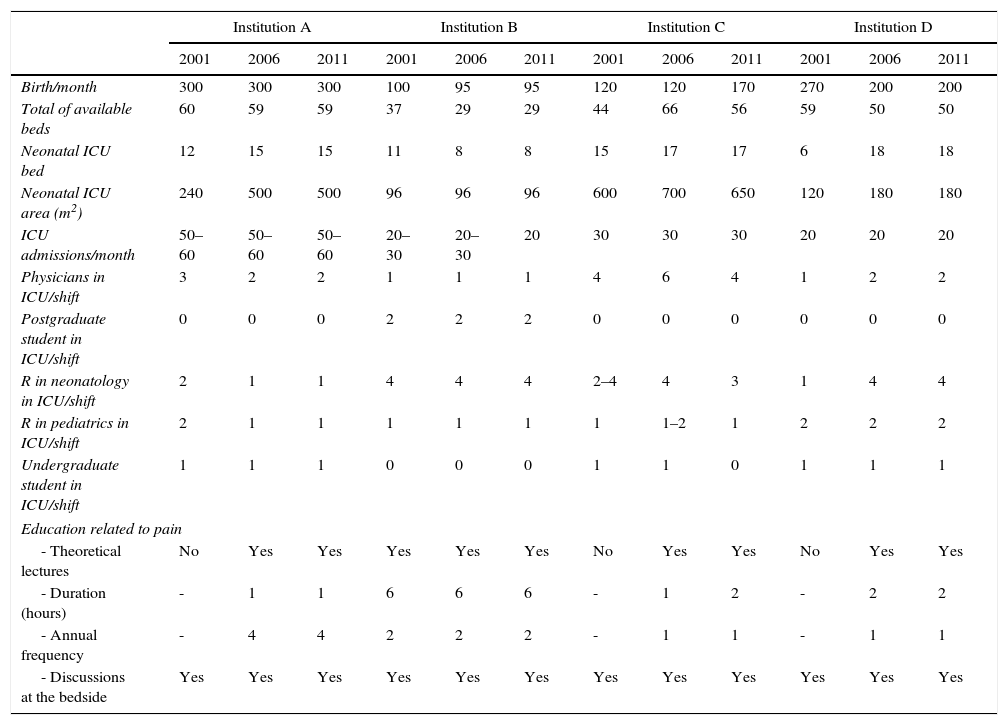
ResultsThe characteristics of the four units in the three study periods are shown in Table 1. All of them were reference units for high-risk pregnancies and included residents in Pediatrics and Neonatology. Regarding teaching on pain and analgesia in the neonatal period, only one institution reported having a formal theoretical program in 2001, although the heads of the NICUs reported having discussed pain and analgesia at bedside in all units. In 2006 and 2011, all units reported theoretical lectures and practical discussions on the topic.
Characteristics of the units regarding the total number of beds, physical area, monthly mean number of births and admissions, personnel involved every day in neonatal care in the neonatal ICUs (number of undergraduate students, residents in pediatrics and neonatology, graduate students, and doctors), education regarding pain and analgesia in the neonatal period.
| Institution A | Institution B | Institution C | Institution D | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | |
| Birth/month | 300 | 300 | 300 | 100 | 95 | 95 | 120 | 120 | 170 | 270 | 200 | 200 |
| Total of available beds | 60 | 59 | 59 | 37 | 29 | 29 | 44 | 66 | 56 | 59 | 50 | 50 |
| Neonatal ICU bed | 12 | 15 | 15 | 11 | 8 | 8 | 15 | 17 | 17 | 6 | 18 | 18 |
| Neonatal ICU area (m2) | 240 | 500 | 500 | 96 | 96 | 96 | 600 | 700 | 650 | 120 | 180 | 180 |
| ICU admissions/month | 50–60 | 50–60 | 50–60 | 20–30 | 20–30 | 20 | 30 | 30 | 30 | 20 | 20 | 20 |
| Physicians in ICU/shift | 3 | 2 | 2 | 1 | 1 | 1 | 4 | 6 | 4 | 1 | 2 | 2 |
| Postgraduate student in ICU/shift | 0 | 0 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| R in neonatology in ICU/shift | 2 | 1 | 1 | 4 | 4 | 4 | 2–4 | 4 | 3 | 1 | 4 | 4 |
| R in pediatrics in ICU/shift | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1–2 | 1 | 2 | 2 | 2 |
| Undergraduate student in ICU/shift | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 |
| Education related to pain | ||||||||||||
| - Theoretical lectures | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes |
| - Duration (hours) | - | 1 | 1 | 6 | 6 | 6 | - | 1 | 2 | - | 2 | 2 |
| - Annual frequency | - | 4 | 4 | 2 | 2 | 2 | - | 1 | 1 | - | 1 | 1 |
| - Discussions at the bedside | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
ICU, intensive care unit; R, residents.
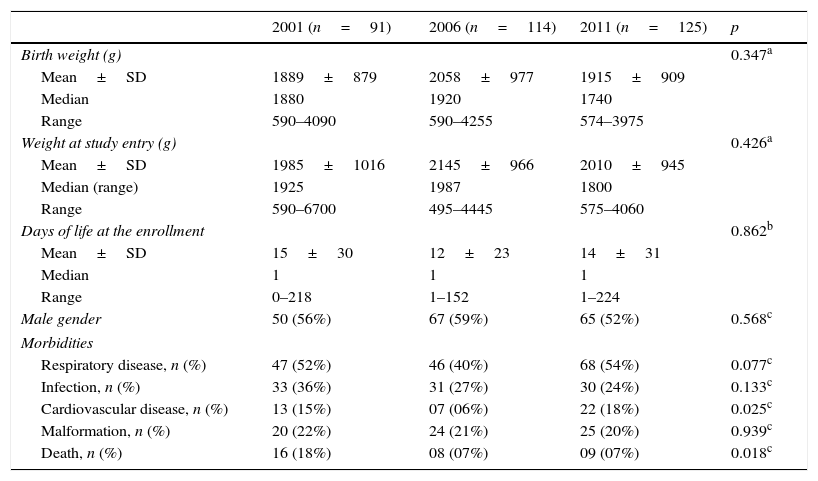
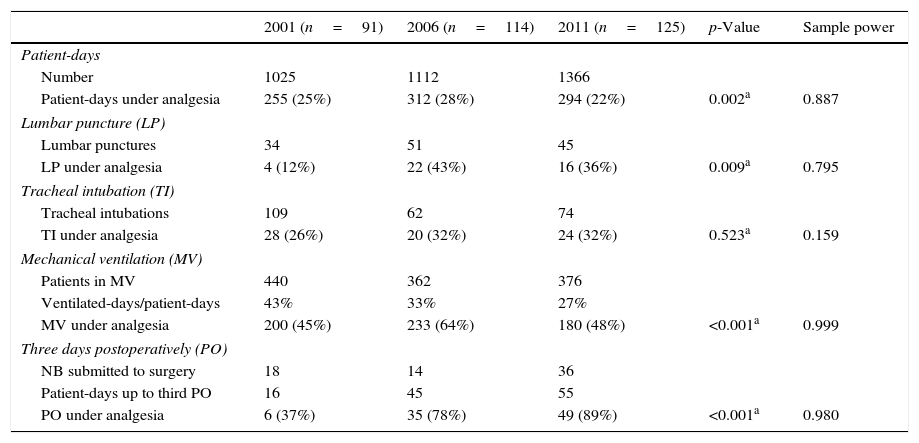
In the month of the study, a total of 91 patients were admitted in 2001, 114 in 2006, and 125 in 2011, considering the four institutions. The characteristics of these patients are shown in Table 2. The 91 neonates admitted to the four institutions totaled 1025 patient-days in 2001, the 114 newborns amounted to 1112 patient-days in 2006, and in 2011, 125 newborns totaled 1366 patient-days. As for the four assessed painful situations (lumbar puncture, tracheal intubation, mechanical ventilation, and the first three postoperative days), there was an increase of analgesic use in 2006 when compared with 2001. In 2011, compared with 2006, there was a reduction of analgesia prescribed to patients receiving mechanical ventilation and lumbar puncture and there were no modifications for tracheal intubation. As for the postoperative period (three days), there was a significant and progressive increase in the use of analgesia over the years (Table 3). For all the analyzed situations, the sample power was greater than 80%, except for tracheal intubation under analgesia.
Clinical characteristics of newborns assessed in the four neonatal intensive care units for a month, with a five-year interval.
| 2001 (n=91) | 2006 (n=114) | 2011 (n=125) | p | |
|---|---|---|---|---|
| Birth weight (g) | 0.347a | |||
| Mean±SD | 1889±879 | 2058±977 | 1915±909 | |
| Median | 1880 | 1920 | 1740 | |
| Range | 590–4090 | 590–4255 | 574–3975 | |
| Weight at study entry (g) | 0.426a | |||
| Mean±SD | 1985±1016 | 2145±966 | 2010±945 | |
| Median (range) | 1925 | 1987 | 1800 | |
| Range | 590–6700 | 495–4445 | 575–4060 | |
| Days of life at the enrollment | 0.862b | |||
| Mean±SD | 15±30 | 12±23 | 14±31 | |
| Median | 1 | 1 | 1 | |
| Range | 0–218 | 1–152 | 1–224 | |
| Male gender | 50 (56%) | 67 (59%) | 65 (52%) | 0.568c |
| Morbidities | ||||
| Respiratory disease, n (%) | 47 (52%) | 46 (40%) | 68 (54%) | 0.077c |
| Infection, n (%) | 33 (36%) | 31 (27%) | 30 (24%) | 0.133c |
| Cardiovascular disease, n (%) | 13 (15%) | 07 (06%) | 22 (18%) | 0.025c |
| Malformation, n (%) | 20 (22%) | 24 (21%) | 25 (20%) | 0.939c |
| Death, n (%) | 16 (18%) | 08 (07%) | 09 (07%) | 0.018c |
Number of patient-days, patient-days undergoing painful procedures, and patient-days that were under analgesia in the four neonatal intensive care units in the assessed years.
| 2001 (n=91) | 2006 (n=114) | 2011 (n=125) | p-Value | Sample power | |
|---|---|---|---|---|---|
| Patient-days | |||||
| Number | 1025 | 1112 | 1366 | ||
| Patient-days under analgesia | 255 (25%) | 312 (28%) | 294 (22%) | 0.002a | 0.887 |
| Lumbar puncture (LP) | |||||
| Lumbar punctures | 34 | 51 | 45 | ||
| LP under analgesia | 4 (12%) | 22 (43%) | 16 (36%) | 0.009a | 0.795 |
| Tracheal intubation (TI) | |||||
| Tracheal intubations | 109 | 62 | 74 | ||
| TI under analgesia | 28 (26%) | 20 (32%) | 24 (32%) | 0.523a | 0.159 |
| Mechanical ventilation (MV) | |||||
| Patients in MV | 440 | 362 | 376 | ||
| Ventilated-days/patient-days | 43% | 33% | 27% | ||
| MV under analgesia | 200 (45%) | 233 (64%) | 180 (48%) | <0.001a | 0.999 |
| Three days postoperatively (PO) | |||||
| NB submitted to surgery | 18 | 14 | 36 | ||
| Patient-days up to third PO | 16 | 45 | 55 | ||
| PO under analgesia | 6 (37%) | 35 (78%) | 49 (89%) | <0.001a | 0.980 |
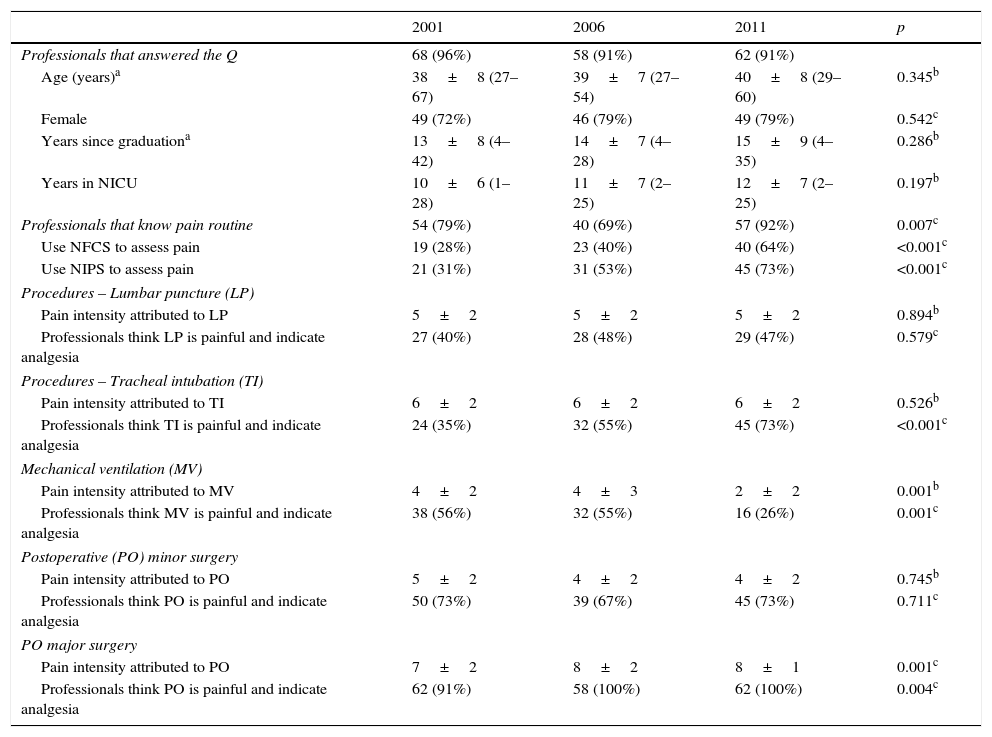
Regarding the medical opinion, 68 (96%) neonatologists answered the questionnaire in 2001, 58 (91%) in 2006, and 62 (91%) in 2011. There was no significant difference regarding the demographic data of the professionals in these three periods (Table 4). Over time, there was an increase in the number of professionals who stated they knew the unit pain routine and used the Neonatal Facial Coding System (NFCS) and/or Neonatal Infant Pain Scale (NIPS) pain scales.
Characteristics of professionals working in four units assessed together, their knowledge of the pain routine in their units and their opinions about the potentially painful procedures (lumbar puncture, intubation, mechanical ventilation, and minor and major postoperative).
| 2001 | 2006 | 2011 | p | |
|---|---|---|---|---|
| Professionals that answered the Q | 68 (96%) | 58 (91%) | 62 (91%) | |
| Age (years)a | 38±8 (27–67) | 39±7 (27–54) | 40±8 (29–60) | 0.345b |
| Female | 49 (72%) | 46 (79%) | 49 (79%) | 0.542c |
| Years since graduationa | 13±8 (4–42) | 14±7 (4–28) | 15±9 (4–35) | 0.286b |
| Years in NICU | 10±6 (1–28) | 11±7 (2–25) | 12±7 (2–25) | 0.197b |
| Professionals that know pain routine | 54 (79%) | 40 (69%) | 57 (92%) | 0.007c |
| Use NFCS to assess pain | 19 (28%) | 23 (40%) | 40 (64%) | <0.001c |
| Use NIPS to assess pain | 21 (31%) | 31 (53%) | 45 (73%) | <0.001c |
| Procedures – Lumbar puncture (LP) | ||||
| Pain intensity attributed to LP | 5±2 | 5±2 | 5±2 | 0.894b |
| Professionals think LP is painful and indicate analgesia | 27 (40%) | 28 (48%) | 29 (47%) | 0.579c |
| Procedures – Tracheal intubation (TI) | ||||
| Pain intensity attributed to TI | 6±2 | 6±2 | 6±2 | 0.526b |
| Professionals think TI is painful and indicate analgesia | 24 (35%) | 32 (55%) | 45 (73%) | <0.001c |
| Mechanical ventilation (MV) | ||||
| Pain intensity attributed to MV | 4±2 | 4±3 | 2±2 | 0.001b |
| Professionals think MV is painful and indicate analgesia | 38 (56%) | 32 (55%) | 16 (26%) | 0.001c |
| Postoperative (PO) minor surgery | ||||
| Pain intensity attributed to PO | 5±2 | 4±2 | 4±2 | 0.745b |
| Professionals think PO is painful and indicate analgesia | 50 (73%) | 39 (67%) | 45 (73%) | 0.711c |
| PO major surgery | ||||
| Pain intensity attributed to PO | 7±2 | 8±2 | 8±1 | 0.001c |
| Professionals think PO is painful and indicate analgesia | 62 (91%) | 58 (100%) | 62 (100%) | 0.004c |
Q, questionnaire; NICU, neonatal intensive care unit; NFCS, neonatal facial coding system; NIPS, neonatal infant pain scale.
As for the intensity of pain attributed to painful procedures, there was no difference between the three periods for lumbar puncture and intubation. There was a reduction in the intensity of pain attributed to mechanical ventilation between 2001/2006 and 2011 and the opposite occurred for major surgery (Table 4).
Regarding the practice of analgesia in the three evaluated periods, only 12% of lumbar punctures in 2001 were performed under adequate analgesia for the procedure. After five years (2006), there was an increase in analgesia indication in the units, with a slight decrease in 2011 (Table 3). In the three studied periods, 40–50% of physicians thought that the pain caused by lumbar puncture was at least moderate (VAS >3) and stated that in theory, they indicated the analgesia for the procedure (Table 4).
Regarding tracheal intubation, nearly 30% of the procedures were performed under analgesia in three periods of the study (Table 3). Of the respondents, 35%, 55%, and 73% in 2001, 2006, and 2011, respectively, reported VAS >3 and stated they used analgesics for tracheal intubation (p<0.001; Table 4).
For patients on mechanical ventilation, 45% of ventilated-days were under analgesia in 2001, 64% in 2006, and 48% in 2011 (p<0.001; Table 3). For this situation, there was a significant decrease in neonatologists that reported VAS >3 and stated they used analgesia between 2001–2006 and 2011 (p=0.002; Table 4).
Finally, in the first three postoperative days, 37%, 78%, and 89% of patients received analgesics respectively in 2001, 2006, and 2011 (p=0.013; Table 3). Regarding the physicians, for a small surgery, 73% in 2001, 67% in 2006, and 73% in 2011, considered the postoperative pain moderate to severe and said they prescribed analgesics (p<0.001; Table 4). For major surgeries, 91% in 2001, and 100% in 2006 and 2011 considered the postoperative pain moderate to severe and said they prescribed analgesics (p<0.001; Table 4).
DiscussionThe present study demonstrated, for almost all analyzed painful situations, a distance between the neonatologists’ theoretical attitude and the real practice in neonatal units, although there has been an increase in the awareness about the presence of pain in critically ill newborns mainly between 2001 and 2006, accompanied by more frequent use of analgesics in clinical practice for some of the painful procedures. The study findings confirm the literature3,4 and indicate that critically ill newborns are submitted to several potentially painful procedures, and that their management remains inadequate. The most frequent perception of pain by professionals and the greater use of analgesia for painful procedures in clinical practice between 2001 and 2006 appear to reflect the knowledge improvement in this area.11 Conversely, between 2006 and 2011, the stagnation or reduction in the perception that procedures cause pain and should be performed under analgesia, and the decrease in use of analgesics in clinical practice, except for the postoperative period, seem to be due to the publication of undesirable effects of analgesics in the neonatal period.12,13
The procedures analyzed here were chosen as they are part of the daily routine of a NICU and also because they cause pain, according to consolidated data in the literature14–18; in addition, there are published protocols for drug analgesia in these procedures.11,18–21 Regarding tracheal intubation, Bonow et al.,22 in 2004, evaluated 297 procedures in two neonatal intensive care and two pediatric units for six months. Medications for sedation and analgesia were used in 89% of intubations performed in the Pediatric ICU, and 24% of those in the NICU. In the same year, Simon et al.23 analyzed the use of premedication for intubation in 75 French pediatric and neonatal units and showed that 37% of newborns, 67% of infants, and 92% of older children received analgesics and/or sedatives prior to the procedure. The evidence-based international consensus11 concluded that tracheal intubation without the use of analgesia and sedation should be performed only in neonatal resuscitation in the delivery room or in urgency situations without available venous access; in 2010, the American Academy of Pediatrics19 recommended the use of premedication for tracheal intubation in neonates. In this study, it was observed that, even with progressive increase of the physician's perception that intubation causes pain, a significant percentage of patients were still intubated without any pain relief. One explanation for this would be its performance in emergency situations; however, outside the delivery room, such situations are rare and, in most cases, it is possible that, while a professional prepares the material for intubation, the other manages the analgesics.24 The beneficial effects of sedation and analgesia on intracranial pressure, airway injury, reduction of procedure time, and patient comfort should be considered.25
As for lumbar puncture, a local infiltration of lidocaine in neonates is recommended.21 Sabrine and Sinha26 observed the regular use of analgesics for lumbar puncture in only 9% of the surveyed English NICU. Porter et al.27 studied 140 lumbar punctures, and only in 4% specific analgesic medication was prescribed for the procedure. In this study, in all years, less than half of the newborns submitted to lumbar puncture received some type of analgesic for the procedure. This finding is troubling when compared to what occurs in children and adults, in whom the use of local anesthesia for the puncture is usual.28 It is noteworthy that over 50% of interviewed physicians felt that the pain caused by the lumbar puncture would not be intense enough to justify analgesia.
Analgesia with opioids for ventilated patients is a controversial subject. A study carried out in 2004 indicated worse neurological outcome in preterm infants on mechanical ventilation who received morphine within the first hours of life, for approximately 14 days, with association between this unfavorable outcome and the presence of hypotension prior to opioid infusion.12,13 A meta-analysis29 did not show sufficient evidence to recommend the routine use of opioids for newborns on mechanical ventilation. The incorporation of this knowledge probably explains the huge discrepancy of data between perception and practice of neonatologists regarding pain and analgesia for mechanical ventilation in 2011. It should be noted that, in that year, neonatologists attributed less pain to mechanical ventilation than in the previous years and stated they indicated analgesia less frequently. However, in practice, although the use of analgesia for ventilated patients has decreased, it was much higher than the neonatologists’ theoretical intention to use it.
Finally, regarding the postoperative period, it was the undertreatment of pain in neonates undergoing surgical procedures that triggered the interest of the scientific community on the subject.30 There is no doubt that postoperative pain increases neonatal morbidity and mortality.31,32 The present study demonstrated that medical knowledge in this regard has improved; in 2006 and 2011, all neonatologists considered the postoperative period a painful event and stated they prescribed analgesia. The clinical practice, however, can be analyzed from two points of view: one, optimistic, observing that the postoperative use of analgesia increased from 33% in 2001 to 89% in 2011, bringing the theoretical knowledge of neonatologists closer to their practice. Under the pessimistic viewpoint, it can be observed that, although all the neonatologists feel that postoperative newborns need analgesics, over 10% of hospitalized patients in the four university units in 2011 did not receive any analgesic dose in the first three days postoperatively. Medical knowledge, especially with regard to therapeutic procedures and medical posture, depends more on what students infer based on the performance of their mentors, than on the transmission of their theoretical knowledge.33 In this context, the gap between medical knowledge and practice in university hospitals, where appropriate and updated training of human resources is as much a priority as the high standard care to their patients, is of concern.
It is noteworthy that, to understand the present study, it is necessary to critically review its major limitation: the research compared neonatologists’ perceptions about the presence, intensity, and need to treat pain triggered by procedures, with the frequency of analgesic use in newborns undergoing such procedures, and it was not possible to individually point out the discrepancy between the theoretical knowledge and practical performance of each responding healthcare professional. The study was limited to analyzing the prescription of pharmacological analgesia, regardless of nonpharmacological measures, which could help relieve pain in several procedures. Finally, when considering only a month of each assessed year, the survey had limited statistical power to detect differences in the practice of analgesia for tracheal intubation. Nevertheless, the scenario shown here indicates the need to improve the models of continuing education regarding neonatal pain, so that the university neonatal units have professionals that can apply their knowledge at the bedside and modify such knowledge in accordance with the dynamic acquisition of information that is built from the critical reading of scientific literature on the subject.
It can be concluded that, over a ten-year period, there was an increase in the use of analgesics for the assessed painful procedures and an increased perception by physicians that newborns feel pain. The gap between the actual use of analgesics in clinical practice and medical perception about the need for analgesia during painful procedures persisted in the four assessed intensive care units. It is essential to analyze the factors that interfere in medical practice and develop strategies to treat pain associated with invasive procedures in the neonatal period.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Prestes AC, Balda RC, dos Santos GM, Rugolo LM, Bentlin MR, Magalhães M, et al. Painful procedures and analgesia in the NICU: what has changed in the medical perception and practice in a ten-year period? J Pediatr (Rio J). 2016;92:88–95.
Study conducted at Faculdade de Ciências Médicas da Santa Casa de São Paulo (FCMSCSP), São Paulo, SP, Brazil; Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil; Faculdade de Medicina de Botucatu (FMB), Universidade Estadual Paulista Júlio de Mesquita Filho (UNESP), Botucatu, SP, Brazil; and Escola Paulista de Medicina (EPM), Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.