Echocardiography has become an indispensable bedside diagnostic tool in the realm of pediatric intensive care units (PICU). It has proven to be an influential factor in the formula of clinical decision-making. This study aimed to delineate the impact of echocardiography on the management of critically ill pediatric patients in the PICU at Sultan Qaboos University Hospital, Oman.
MethodThis was a retrospective cohort study conducted in a five-bed PICU. Patients admitted to the PICU from January of 2011 to December of 2012 were reviewed. Those who have undergone bedside echocardiography during their ICU stay were recruited. Electronic patient record was used as data source.
ResultsOver a-24-month period, 424 patients were admitted in this PICU. One hundred and one clinically indicated transthoracic echocardiograms were performed. 81.8% of these presented new findings (n=82) that significantly impacted the clinical decision of patient management, namely, alteration in drug therapy and procedure, whereas no difference in the management was yielded in the remaining 17.8% of the studied cases.
ConclusionsEchocardiography had a significant impact on the management of PICU patients. Such salutary effect was consequently reflected on the outcome. Pediatric intensivists are encouraged to acquire such bedside skill.
A ecocardiografia se tornou uma ferramenta de diagnóstico relevante, indispensável no âmbito das unidades de terapia intensiva pediátrica (UTIP). Ela se tornou um fator influente na tomada de decisões clínicas. O objetivo deste estudo foi delinear o impacto da ecocardiografia sobre o manejo de pacientes pediátricos gravemente doentes na UTIP do Hospital Universitário Sultan Qaboos, em Omã.
MétodoEste é um estudo de coorte retrospectivo realizado em uma UTIP de cinco leitos. Foram analisados pacientes internados na UTIP entre janeiro de 2011 e dezembro de 2012. Foram recrutados os pacientes que passaram por ecocardiografia durante sua internação na UTI. O registro eletrônico dos pacientes foi utilizado como fonte de dados.
ResultadosEm um período de 24 meses, 424 pacientes foram internados em nossa UTIP 101 pacientes foram encaminhados para ecocardiografias transtorácicas. 81,8% delas tiveram novos achados (n=82) que afetaram significativamente a decisão clínica, como a terapia medicamentosa e procedimentos, ao passo que não houve nenhuma diferença no manejo nos outros 17,8% dos casos estudados.
ConclusõesA ecocardiografia teve um impacto significativo sobre o manejo de pacientes da UTIP. Esse efeito refletiu-se nos resultados. Os intensivistas pediátricos devem ser incentivados a adquirir essa habilidade relevante.
Management of critically ill pediatric patients is a demanding task that requires proper prioritization and judicious time management. Multi-system affection with overlap of symptoms often complicates the clinical picture. Hemodynamic assessment has recently taken top priority in the management of critically ill patients.1 This is clearly illustrated in the paradigm shift from ABC to CAB.2 Echocardiography is an integral component of the clinical service in the pediatric intensive care unit (PICU). It is considered a handy bedside imaging modality, and an accurate diagnostic tool that explores a crucial body system.1 To incorporate echocardiogram findings along with the clinical signs results in a clear image detailing the hemodynamic status of the critically ill child. This study aimed to delineate the clinical usage of echocardiography in the PICU setting.
MethodsThis was a retrospective observational study. Patients admitted to of the Sultan Qaboos University Hospital PICU period from January of 2011 to December of 2012 were assessed.
This is an open combined medical-surgical five-bed PICU. Moreover, it is an intensivist-led PICU with the support of pediatric board-certified subspecialists. Apart from post-cardiothoracic operative cases, all post-traumatic, medical, and surgical critically ill children are attended to at this unit.
Electronic patient records were reviewed to identify those who had undergone transthoracic echocardiography. The study protocol was approved by the institutional review board.
The following data were collected; (1) age and sex of the patients at PICU admission, (2) clinical indications for echocardiography, (3) echocardiographic findings, (4) clinical decision or intervention based on the echocardiographic findings. Intervention or management alteration after the echocardiography was classified into four main categories; (1) altered drug therapy, (2) altered procedure, (3) altered decision-making, and (4) others (the exact nature of these changes was specified in details).
Statistical analysisData were analyzed using SPSS version 17.0 (SPSS Inc. Released 2008. SPSS Statistics for Windows, Chicago, USA). Descriptive statistics, such as mean(±standard deviation) for normally distributed data or median and interquartile range (IQR) for non-normally distributed variables, were calculated for quantitative parameters. Qualitative data were summarized as frequency and percentage for categorical variables. The Fisher's exact test was used to test the significance of the results at the 5% level. Some data were violated to affirm fitting the assumptions required by the statistical analyses.
ResultsDuring the study period, 424 patients were admitted to this PICU, and 101 echocardiograms were performed for 93 patients. Nine patients had two or more echocardiograms performed during their PICU stay. There were 57 males and 44 females; most patients (n=41, 40.6%) were below 12 months of age. The age ranged from 1 to 5 years among 32 patients (31.7%), while 28 patients (27.5%) were above 5 years. A total of 80 patients were discharged from PICU (79.2%), whereas 21 patients (20.8%) died.
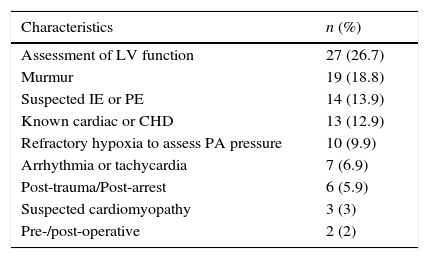
Two registered cardiac sonographers and one consultant cardiologist (second author) were the staff that carried out the echocardiographic examination. Interpretations were provided by a board-certified consultant pediatric cardiologist. Indications for echocardiograms are shown in Table 1. Over one-fourth of exams were conducted to assess left ventricular function in hemodynamically unstable patients (27 exams, 26.7%). Suspicion of congenital heart disease was the second most common indication (19 exams, 18.8%).
Indication for 101 echocardiography exams.
| Characteristics | n (%) |
|---|---|
| Assessment of LV function | 27 (26.7) |
| Murmur | 19 (18.8) |
| Suspected IE or PE | 14 (13.9) |
| Known cardiac or CHD | 13 (12.9) |
| Refractory hypoxia to assess PA pressure | 10 (9.9) |
| Arrhythmia or tachycardia | 7 (6.9) |
| Post-trauma/Post-arrest | 6 (5.9) |
| Suspected cardiomyopathy | 3 (3) |
| Pre-/post-operative | 2 (2) |
LV, left ventricular; IE, infective endocarditis; PE, pericardial effusion; CHD, congenital heart disease; PA, pulmonary artery.
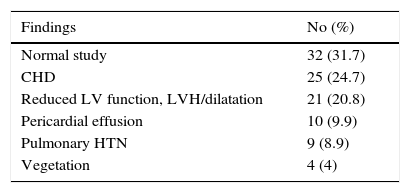
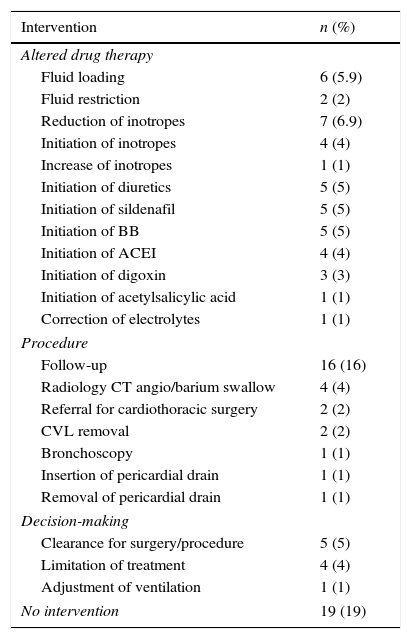
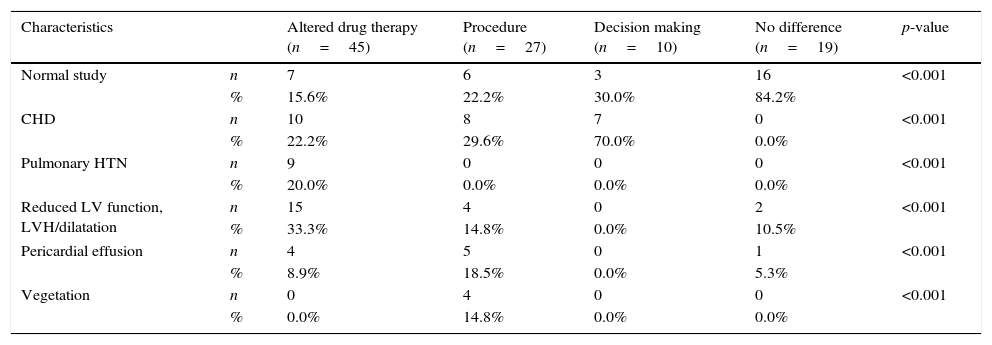
The findings were classified into categories of interest (Table 2). Normal exam was the most common finding (30%); 81 exams (81%) produced new findings that resulted in additional clinical management steps of potential salutary effect, and 19 (18.8%) yielded clinically insignificant findings (Table 3). Such post-echocardiography clinical management alterations are detailed in Table 4). There was a significant positive correlation between the findings of the studies and the clinical intervention or the clinical decision. It is noteworthy that the p-value of all results was <0.001.
Echocardiographic findings in 101 exams.
| Findings | No (%) |
|---|---|
| Normal study | 32 (31.7) |
| CHD | 25 (24.7) |
| Reduced LV function, LVH/dilatation | 21 (20.8) |
| Pericardial effusion | 10 (9.9) |
| Pulmonary HTN | 9 (8.9) |
| Vegetation | 4 (4) |
CHD, congenital heart disease; LV, left ventricular; LVH, left ventricular hypertrophy; HTN, hypertension.
Impact of echocardiography on decision-making.
| Intervention | n (%) |
|---|---|
| Altered drug therapy | |
| Fluid loading | 6 (5.9) |
| Fluid restriction | 2 (2) |
| Reduction of inotropes | 7 (6.9) |
| Initiation of inotropes | 4 (4) |
| Increase of inotropes | 1 (1) |
| Initiation of diuretics | 5 (5) |
| Initiation of sildenafil | 5 (5) |
| Initiation of BB | 5 (5) |
| Initiation of ACEI | 4 (4) |
| Initiation of digoxin | 3 (3) |
| Initiation of acetylsalicylic acid | 1 (1) |
| Correction of electrolytes | 1 (1) |
| Procedure | |
| Follow-up | 16 (16) |
| Radiology CT angio/barium swallow | 4 (4) |
| Referral for cardiothoracic surgery | 2 (2) |
| CVL removal | 2 (2) |
| Bronchoscopy | 1 (1) |
| Insertion of pericardial drain | 1 (1) |
| Removal of pericardial drain | 1 (1) |
| Decision-making | |
| Clearance for surgery/procedure | 5 (5) |
| Limitation of treatment | 4 (4) |
| Adjustment of ventilation | 1 (1) |
| No intervention | 19 (19) |
BB, β-adrenoreceptor blocker; ACEI, angiotensin-converting enzyme inhibitors; CT, computed tomography; CVL, central venous line.
Interventions after echocardiography.
| Characteristics | Altered drug therapy (n=45) | Procedure (n=27) | Decision making (n=10) | No difference (n=19) | p-value | |
|---|---|---|---|---|---|---|
| Normal study | n | 7 | 6 | 3 | 16 | <0.001 |
| % | 15.6% | 22.2% | 30.0% | 84.2% | ||
| CHD | n | 10 | 8 | 7 | 0 | <0.001 |
| % | 22.2% | 29.6% | 70.0% | 0.0% | ||
| Pulmonary HTN | n | 9 | 0 | 0 | 0 | <0.001 |
| % | 20.0% | 0.0% | 0.0% | 0.0% | ||
| Reduced LV function, LVH/dilatation | n | 15 | 4 | 0 | 2 | <0.001 |
| % | 33.3% | 14.8% | 0.0% | 10.5% | ||
| Pericardial effusion | n | 4 | 5 | 0 | 1 | <0.001 |
| % | 8.9% | 18.5% | 0.0% | 5.3% | ||
| Vegetation | n | 0 | 4 | 0 | 0 | <0.001 |
| % | 0.0% | 14.8% | 0.0% | 0.0% |
CHD, congenital heart disease; HTN, hypertension; LV, left ventricular; LVH, left ventricular hypertrophy.
Determining the impact of echocardiography in ICU has long been of interest to research and clinical studies.3–7 Various studies assessed the use of echocardiograms in adult ICU patients, yet few dealt with the pediatric population.8–12 The present study has clearly demonstrated the significance of echocardiography in approximately 82% of the cases. Not only it supported the clinical decision in most of the cases, but it also helped adjusting the management of those patients. Normal echocardiographic findings were the most prevalent result. This illustrates how ambiguous the cardiac condition could be in the eyes of the clinician were it not for the echocardiography. Normal heart by echocardiographic examination is an invaluable information to be incorporated in the assessment of a hypotensive patient. Congenital heart disease was the second most common finding, an observation that is unique to the pediatric studies when compared with adult studies.
Assessment of the left ventricular function is by far the most common indication of echocardiograms across both adult and pediatric studies.4–12 It is imperative for the clinician to define the cardiac contribution to the hypotensive state of a critical patient. Sometimes, the clinical decision is at the point of decision where the clinician is not sure whether to primarily focus on supporting the cardiac function or to adopt fluid support with special consideration to sepsis.13 Echocardiography might be a very helpful indicator in such critical timing. Such crucial role of echocardiography could be sufficiently achieved even when it is not performed by a cardiologist.3 Interestingly, it has been shown that only minimal training would qualify a non-cardiologist to accurately assess left ventricular function when compared with blinded cardiologist's interpretations. Furthermore, a prospective single-center study has shown that a critical care physician could be capable of assessing LV function through echocardiography, in good correlation with the cardiac index measured invasively by pulmonary catheterization.13
Pericardial effusion was one the concerns addressed by the echocardiography in different ICU studies.4–6 Despite having defined clinical diagnostic criteria, the sensitivity of these findings highlight the need for echocardiography for a firm diagnosis.
Moreover, unexplained hypoxemia is not an uncommon ICU dilemma, especially complicating the picture of ventilated patients. Screening for pulmonary hypertension with tricuspid regurge jet velocity has proven to be an invaluable clue to explain defective oxygenation.13 Obviously, these important diagnostic clues change the management. Echoing previous studies, the most common resulting intervention was altered drug therapy, mainly inotropes and fluid management.4,14
The present study bears the limitations of the retrospective observational design. Determination of the causal relationship and proper definition of the effect of confounders were both restricted. Furthermore, this was a single-center study with relatively small sample size. The fact that this study was neither randomized nor blinded hindered proper assessment of the impact of echocardiography upon the outcome of critically ill children. Such limitations prevent the generalization of the study findings.
Additionally, candidate patients who would most probably benefit from the echocardiography could not be identified. Nevertheless, those candidates might be the hemodynamically unstable patients, since the most common indications for echocardiography were hypotension and assessment of left ventricular function.
Echocardiography is a noninvasive, accurate bedside exam in the PICU. Establishing intensivist-driven echocardiograms affects the management of the critically ill patient admitted to PICU. Large prospective clinical studies are needed to properly define the indications and effects of such handy procedure in the PICU setting.
Conflicts of interestThe authors declare no conflicts of interest.
The authors are grateful to Dr. Ismail El-Beshlawi for his advice on the preparation and writing of this manuscript.
Please cite this article as: Rabah F, Al-Senaidi K, Beshlawi I, Alnair A, Abdelmogheth A-A. Echocardiography in PICU: when the heart sees what is invisible to the eye. J Pediatr (Rio J). 2016;92:96–100.