To describe the opinions of pediatricians who teach resuscitation in Brazil on initiating and limiting the delivery room resuscitation of extremely preterm infants.
MethodCross-sectional study with electronic questionnaire (Dec/2011–Sep/2013) sent to pediatricians who are instructors of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics, containing three hypothetical clinical cases: (1) decision to start the delivery room resuscitation; (2) limitation of neonatal intensive care after delivery room resuscitation; (3) limitation of advanced resuscitation in the delivery room. For each case, it was requested that the instructor indicate the best management for each gestational age between 23 and 26 weeks. A descriptive analysis was performed.
Results560 (82%) instructors agreed to participate. Only 9% of the instructors reported the existence of written guidelines at their hospital regarding limitations of delivery room resuscitation. At 23 weeks, 50% of the instructors would initiate delivery room resuscitation procedures. At 26 weeks, 2% would decide based on birth weight and/or presence of fused eyelids. Among the participants, 38% would re-evaluate their delivery room decision and limit the care for 23-week neonates in the neonatal intensive care unit. As for advanced resuscitation, 45% and 4% of the respondents, at 23 and 26 weeks, respectively, would not apply chest compressions and/or medications.
ConclusionDifficulty can be observed regarding the decision to not resuscitate a preterm infant with 23 weeks of gestational age. At the same time, a small percentage of pediatricians would not resuscitate neonates of unquestionable viability at 26 weeks of gestational age in the delivery room.
Descrever opiniões dos pediatras que ensinam reanimação no Brasil a respeito de iniciar e limitar a reanimação em sala de parto de neonatos pré-termo extremos.
MétodoEstudo transversal com questionário eletrônico (Dez/11-Set/13) enviado aos instrutores do Programa de Reanimação Neonatal da Sociedade Brasileira de Pediatria contendo três casos clínicos hipotéticos: 1) decisão de iniciar ou não a reanimação; 2) limitação ou não dos cuidados intensivos após a reanimação em sala de parto; 3) limitação ou não da reanimação avançada em sala de parto. Para cada caso foi solicitada a indicação da conduta para cada idade gestacional entre 23-26 semanas. A análise foi descritiva por meio da frequência das respostas.
Resultados560 (82%) instrutores consentiram em participar. Apenas 9% instrutores afirmaram existir em seu hospital norma escrita sobre quando não iniciar a reanimação em sala de parto. Com 23 semanas, 50% dos instrutores fariam a reanimação em sala de parto e, com 26 semanas, 2% baseariam sua decisão no peso ao nascer e/ou na abertura da fenda palpebral. Dos entrevistados, 38% reavaliariam sua decisão e limitariam o cuidado na UTI a medidas de conforto para nascidos de 23 semanas reanimados na sala de parto. Quanto aos procedimentos de reanimação avançada, 45% e 4% com 23 e 26 semanas, respectivamente, não indicariam tais manobras.
ConclusãoObserva-se dificuldade na opção de não reanimar neonatos com 23 semanas de gestação e, ao mesmo tempo, um pequeno percentual de pediatras não reanima, na sala de parto, neonatos cuja viabilidade não é questionada (26 semanas).
Available data indicate that infants at less than 23 weeks of gestational age are too immature to survive with the current technology; on the other hand, those born at 25 weeks or more have significant survival rates and a large proportion of them survive without severe sequelae.1–4 Thus, using as guide the survival rates of preterm neonates, the literature, in general, has established as the limit of viability the period between 22 and 25 weeks of gestational age (GA), below which the degree of biological immaturity is a limiting factor to life and above which the benefit of treatment is not challenged.5,6
However, there is great difficulty in defining the proper management for fetuses born between these limits. During this period, the uncertainty of the result is the rule, rather than the exception, and is therefore referred to as the “gray area,” because survival and prognosis are uncertain, and there is doubt about the best approach to be used and the degree of investment and intervention to be made, since the data available for decision-making are limited, and although they help, they do not overrule the uncertainty or the possibility of error. For the group of infants born in the gray area, two courses of action are possible: (1) restriction of life support measures and the possibility of death as outcome, or increase in sequelae if the patient does not die; or (2) access to all available technology, having as possible outcomes death with pain and suffering, or the possibility of survival with high rates of major sequelae, or the chance of a good clinical evolution, with survival without sequelae or with minor sequelae.5,7–10
Therefore, considering the multiple uncertainties, the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics (Programa de Reanimação Neonatal da Sociedade Brasileira de Pediatria [PRN-SBP]) recommends caution and, considering the additional information obtained after the birth, the decision not to resuscitate may be made by the medical team in the delivery room or, if doubts remain, the team must resuscitate the patient, take him to the NICU, and then gather the necessary information, including the family's wishes, in order to eventually limit the life support measures.
In this context, it is essential to know what Brazilian physicians think about the role of parents in decision-making about the type of intervention they want for their children, such as how the decisions are made about the resuscitation of an extremely preterm neonate and how the possible sequelae of these fetuses are addressed with parents; i.e., what Brazilian physicians think about these ethical issues. Thus, the aim of this research was to describe the opinions of pediatricians who teach resuscitation in Brazil regarding the decisions to initiate and limit resuscitation of extremely preterm newborns in the delivery room, based on hypothetical clinical cases, comparing them according to the Brazilian macro-region where the professional works.
MethodAfter being approved by the Research Ethics Committee of Universidade Federal de São Paulo and the Board of the Brazilian Society of Pediatrics, a cross-sectional study was carried out from December 2011 to September 2013 with pediatricians who were active PRN-SBP instructors. Sample size calculation was not performed, because the study aimed to evaluate the universe of active PRN-SBP instructors.
An electronic questionnaire was developed, using as a basis the tool validated and utilized by Martinez et al.11 All active PRN-SBP instructors received a link to the questionnaire by email and a personal password access. After entering the password, the instructor received an explanation of the research, and after agreeing to participate by accepting the informed consent, access to the questionnaire was provided.
The questionnaire had three axes. The first axis referred to the characterization of the interviewee, with demographic and professional data. The second axis contained 17 multiple-choice questions and an obligatory answer regarding the current practices on neonatal resuscitation and ethical issues involved in the resuscitation of extremely preterm neonates. The last axis discussed the three clinical cases that are the focus of this study. The response control for each instructor was accessible only to the main investigator, and anonymity was guaranteed regarding the tabulation of results.
As for the three clinical cases, the first one concerned the decision to start resuscitation in the delivery room: You are called urgently to the delivery room to assist a vaginal birth of a twin pregnancy. The first twin was born with irregular breathing and the second was born with poor vitality, with apnea and bradycardia. There was no time to talk to the parents about resuscitation. Indicate, for each gestational age (23, 24, 25, and 26 weeks), the choice regarding your management: 1) You resuscitate the two newborns; 2) You do not resuscitate the second, but resuscitate the first; 3) You do not resuscitate either of them; 4) You verify if the eyelids are still fused in each newborn and make the decision to resuscitate; 5) You verify the birth weight of each patient and make the decision.
The second case concerned the limitation or not of neonatal intensive care after resuscitation in the delivery room: Assuming that the two newborns from Case 1 were resuscitated in the delivery room by the on-duty pediatrician, who referred them to the NICU where you are on call. Currently, the patients are in the transport incubator, receiving free flow oxygen and showing intense respiratory effort. Indicate, for each gestational age (23, 24, 25, and 26 weeks), the choice regarding your management: 1) Provide comfort care (heat and free flow oxygen); 2) Provide continuous positive airway pressure (CPAP) nasally; 3) Provide mechanical ventilation and surfactant.
The third case addressed the limitation of advanced resuscitation in the delivery room: You are called to the delivery room to assist an extremely preterm neonate born due to placental abruption. You talk briefly to the mother and explain about the possibility of the child being born in critical condition and dying in the delivery room. The mother asks that everything be done to save the newborn's life. The patient is born showing apnea and severe bradycardia, is quickly intubated after failed mask ventilation, and remains with heart rate (HR) <60 bpm despite adequate ventilation. Indicate, for each gestational age (23, 24, 25, and 26 weeks), the choice regarding your management: 1) Indicate chest compressions and adrenaline, and considers umbilical catheterization for volume expansion; 2) Maintain only ventilation, transfer the patient to the NICU, and wait for the newborn's death; 3) Suspend ventilation and wait for the newborn's death to occur in the delivery room.
The statistical analysis was descriptive. The qualitative variables were described by frequency of events, and the quantitative variables, by measures of central tendency. All answers were analyzed for the group as a whole and according to the region where instructors worked (North, Northeast, and Midwest vs. South and Southeast). The comparison of the responses according to the five Brazilian macro-regions where the interviewed instructors worked was carried out by chi-squared test, with a level of significance of p<0.05.
ResultsDuring the study period, there were 829 instructors, of whom 130 were inactive and 14 refused to participate. Thus, the final target population of the study consisted of 685 active PRN-SBP instructors. Of these, 560 instructors (82%) answered the questionnaire. The distribution of instructors who answered the questionnaire per state ranged from 76% (São Paulo) to 100% (Amazonas, Rondônia, Roraima, and Espírito Santo).
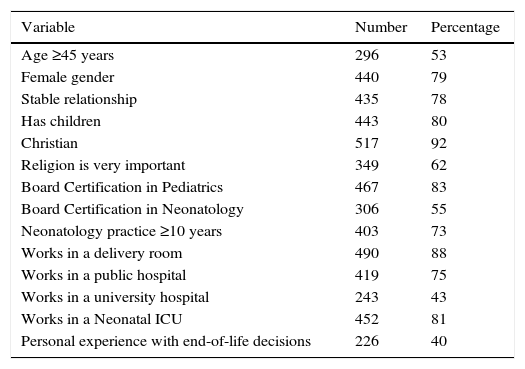
The general characteristics of the respondents are shown in Table 1. The mean age of the respondents was 45±9 years (range: 27–67). As for religion, of the 517 who professed the Christian faith, 68% were Catholics, 15% Spiritualists, 7% were evangelical Protestants, and 2% professed other Protestant beliefs. In terms of place of residence, the instructors were distributed as follows: 68 (12%) in the North, 179 (32%) in the Northeast, 36 (6%) in the Midwest, 208 (37%) in the Southeast, and 69 (12%) in the South, with 363 (65%) living in the state capitals and 197 (35%) in the countryside. Regarding training and professional performance, the time since graduation from medical school was on average 22±9 years (range: 4–45) and the time working in neonatology was 16±8 years (range: 1–40).
General characteristics of the 560 instructors of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics who participated in the study.
| Variable | Number | Percentage |
|---|---|---|
| Age ≥45 years | 296 | 53 |
| Female gender | 440 | 79 |
| Stable relationship | 435 | 78 |
| Has children | 443 | 80 |
| Christian | 517 | 92 |
| Religion is very important | 349 | 62 |
| Board Certification in Pediatrics | 467 | 83 |
| Board Certification in Neonatology | 306 | 55 |
| Neonatology practice ≥10 years | 403 | 73 |
| Works in a delivery room | 490 | 88 |
| Works in a public hospital | 419 | 75 |
| Works in a university hospital | 243 | 43 |
| Works in a Neonatal ICU | 452 | 81 |
| Personal experience with end-of-life decisions | 226 | 40 |
ICU, intensive care unit.
Only 50 (9%) of the respondents reported the existence of written guidelines in their hospitals on when to avoid starting resuscitation in the delivery room and when intensive care is indicated for extreme prematurity. However, even without an established institutional guideline, 445 (80%) pediatricians reported using some criteria to limit resuscitation: gestational age was mentioned by 426 (96%) and birth weight by 299 (67%), with 33% reporting that they considered gestational age as the sole criterion for the decision, 5% reported considering only birth weight, and 62% considered both criteria. For 355 (80%) respondents, the reported gestational age used to limit resuscitation was below 24 weeks, and for 263 (59%) pediatricians, the birth weight limit was 500g.
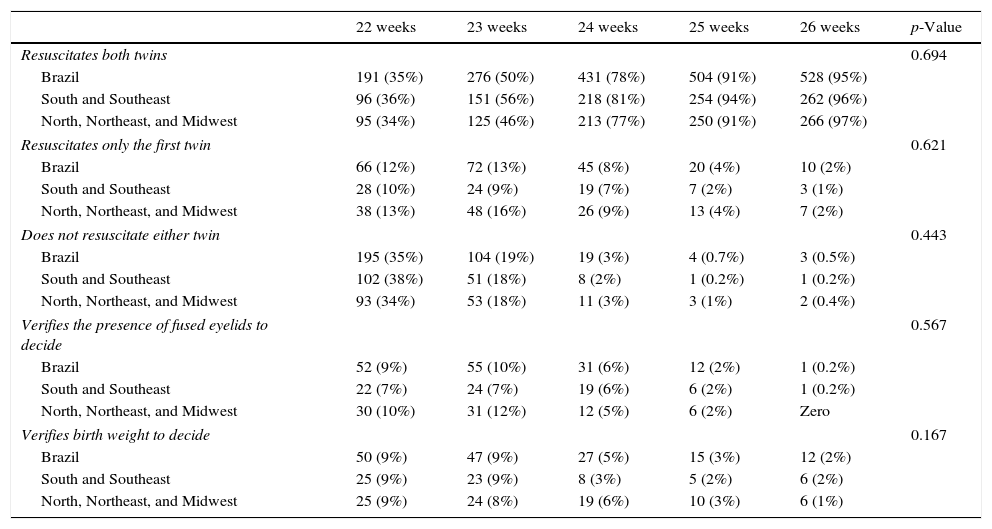
Table 2 shows the percentage of answers to the alternatives related to Case Study 1, according to the gestacional age (GA) of each patient. The greater the GA, the greater the chance the interviewee would resuscitate the two twins. However, even at 23 weeks, 50% of the assessed resuscitation instructors would resuscitate the two neonates; at 26 weeks, 2% would base their decision on the birth weight and/or the presence of fused eyelids. This behavior was observed for the instructors as a whole and also according to their work area (chi-squared: p=0.694).
Decision to start resuscitation in twins when the first twin had, soon after birth, irregular breathing and the second twin had apnea, according to gestational age and the Brazilian region where the pediatrician works.
| 22 weeks | 23 weeks | 24 weeks | 25 weeks | 26 weeks | p-Value | |
|---|---|---|---|---|---|---|
| Resuscitates both twins | 0.694 | |||||
| Brazil | 191 (35%) | 276 (50%) | 431 (78%) | 504 (91%) | 528 (95%) | |
| South and Southeast | 96 (36%) | 151 (56%) | 218 (81%) | 254 (94%) | 262 (96%) | |
| North, Northeast, and Midwest | 95 (34%) | 125 (46%) | 213 (77%) | 250 (91%) | 266 (97%) | |
| Resuscitates only the first twin | 0.621 | |||||
| Brazil | 66 (12%) | 72 (13%) | 45 (8%) | 20 (4%) | 10 (2%) | |
| South and Southeast | 28 (10%) | 24 (9%) | 19 (7%) | 7 (2%) | 3 (1%) | |
| North, Northeast, and Midwest | 38 (13%) | 48 (16%) | 26 (9%) | 13 (4%) | 7 (2%) | |
| Does not resuscitate either twin | 0.443 | |||||
| Brazil | 195 (35%) | 104 (19%) | 19 (3%) | 4 (0.7%) | 3 (0.5%) | |
| South and Southeast | 102 (38%) | 51 (18%) | 8 (2%) | 1 (0.2%) | 1 (0.2%) | |
| North, Northeast, and Midwest | 93 (34%) | 53 (18%) | 11 (3%) | 3 (1%) | 2 (0.4%) | |
| Verifies the presence of fused eyelids to decide | 0.567 | |||||
| Brazil | 52 (9%) | 55 (10%) | 31 (6%) | 12 (2%) | 1 (0.2%) | |
| South and Southeast | 22 (7%) | 24 (7%) | 19 (6%) | 6 (2%) | 1 (0.2%) | |
| North, Northeast, and Midwest | 30 (10%) | 31 (12%) | 12 (5%) | 6 (2%) | Zero | |
| Verifies birth weight to decide | 0.167 | |||||
| Brazil | 50 (9%) | 47 (9%) | 27 (5%) | 15 (3%) | 12 (2%) | |
| South and Southeast | 25 (9%) | 23 (9%) | 8 (3%) | 5 (2%) | 6 (2%) | |
| North, Northeast, and Midwest | 25 (9%) | 24 (8%) | 19 (6%) | 10 (3%) | 6 (1%) | |
p-Value, significance level according to the chi-squared test.
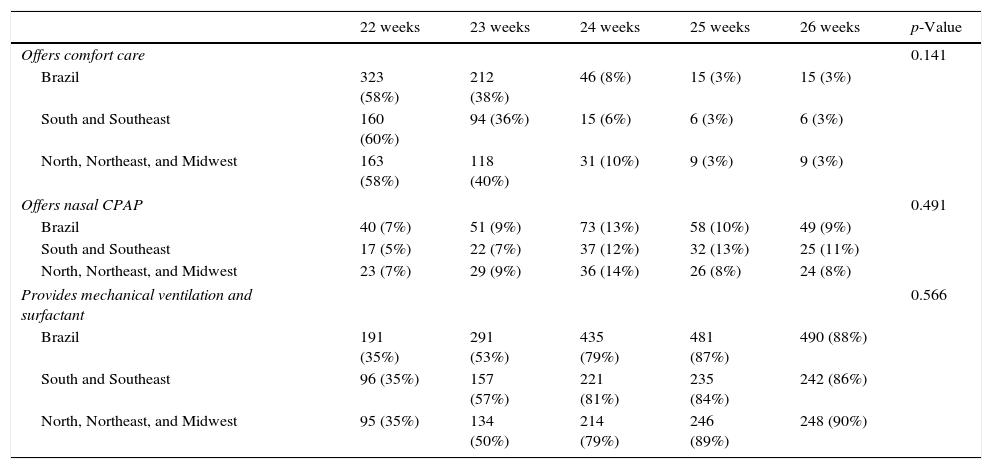
Table 3 shows the percentage of answers for the alternatives related to Case 2 according to the GA of each patient. The greater the GA, the greater the chance the respondent would offer full intensive care, i.e., mechanical ventilation and exogenous surfactant replacement. Part of the respondents considered the possibility that once the neonate was resuscitated in the delivery room, they would review the decision and provide comfort care in the NICU, as 38% of the assessed pediatricians would limit the ICU care to comfort measures for newborns at 23 week of GA effectively resuscitated in the delivery room, the same being mentioned by 3% of respondents for neonates at 26 weeks. Such behavior is observed for the instructors as a whole and also according to their area of work (chi-squared: p=0.141).
Type of care provided to the twins in Case 1 at the neonatal intensive care unit if those patients had been resuscitated, according to gestational age and Brazilian region where the interviewed pediatricians work.
| 22 weeks | 23 weeks | 24 weeks | 25 weeks | 26 weeks | p-Value | |
|---|---|---|---|---|---|---|
| Offers comfort care | 0.141 | |||||
| Brazil | 323 (58%) | 212 (38%) | 46 (8%) | 15 (3%) | 15 (3%) | |
| South and Southeast | 160 (60%) | 94 (36%) | 15 (6%) | 6 (3%) | 6 (3%) | |
| North, Northeast, and Midwest | 163 (58%) | 118 (40%) | 31 (10%) | 9 (3%) | 9 (3%) | |
| Offers nasal CPAP | 0.491 | |||||
| Brazil | 40 (7%) | 51 (9%) | 73 (13%) | 58 (10%) | 49 (9%) | |
| South and Southeast | 17 (5%) | 22 (7%) | 37 (12%) | 32 (13%) | 25 (11%) | |
| North, Northeast, and Midwest | 23 (7%) | 29 (9%) | 36 (14%) | 26 (8%) | 24 (8%) | |
| Provides mechanical ventilation and surfactant | 0.566 | |||||
| Brazil | 191 (35%) | 291 (53%) | 435 (79%) | 481 (87%) | 490 (88%) | |
| South and Southeast | 96 (35%) | 157 (57%) | 221 (81%) | 235 (84%) | 242 (86%) | |
| North, Northeast, and Midwest | 95 (35%) | 134 (50%) | 214 (79%) | 246 (89%) | 248 (90%) | |
p-Value, significance level according to the chi-squared test.
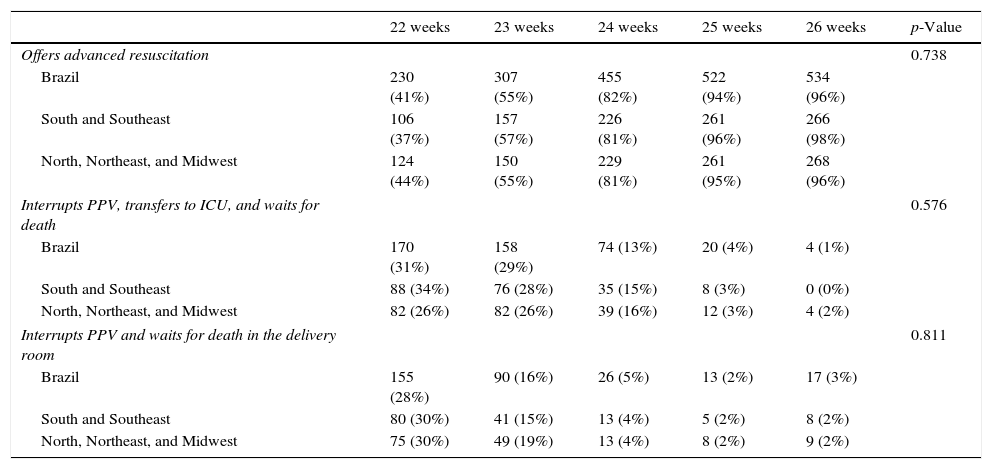
Table 4 shows the percentage of answers for the alternatives related to Case Study 3, according to the GA of each patient. It is observed once again that the higher the GA, the greater the chance that the interviewee would offer advanced resuscitation, starting chest compressions and medications to resuscitate the newborn. At 23 weeks, 55% of the assessed instructors would offer full advanced resuscitation to the patient and, at 26 weeks, 4% would interrupt resuscitation efforts in this situation. Such behavior is observed for instructors as a whole and also according to their region (chi-squared: p=0.738).
Management of a born in poor condition due to placental abruption, that maintains heart rate <60bpm, even after intubation, when the mother has requested that everything should be done to save the newborn's life, according to gestational age and Brazilian region where the interviewed pediatricians work.
| 22 weeks | 23 weeks | 24 weeks | 25 weeks | 26 weeks | p-Value | |
|---|---|---|---|---|---|---|
| Offers advanced resuscitation | 0.738 | |||||
| Brazil | 230 (41%) | 307 (55%) | 455 (82%) | 522 (94%) | 534 (96%) | |
| South and Southeast | 106 (37%) | 157 (57%) | 226 (81%) | 261 (96%) | 266 (98%) | |
| North, Northeast, and Midwest | 124 (44%) | 150 (55%) | 229 (81%) | 261 (95%) | 268 (96%) | |
| Interrupts PPV, transfers to ICU, and waits for death | 0.576 | |||||
| Brazil | 170 (31%) | 158 (29%) | 74 (13%) | 20 (4%) | 4 (1%) | |
| South and Southeast | 88 (34%) | 76 (28%) | 35 (15%) | 8 (3%) | 0 (0%) | |
| North, Northeast, and Midwest | 82 (26%) | 82 (26%) | 39 (16%) | 12 (3%) | 4 (2%) | |
| Interrupts PPV and waits for death in the delivery room | 0.811 | |||||
| Brazil | 155 (28%) | 90 (16%) | 26 (5%) | 13 (2%) | 17 (3%) | |
| South and Southeast | 80 (30%) | 41 (15%) | 13 (4%) | 5 (2%) | 8 (2%) | |
| North, Northeast, and Midwest | 75 (30%) | 49 (19%) | 13 (4%) | 8 (2%) | 9 (2%) | |
PPV, positive pressure ventilation; ICU, intensive care unit; p-value, significance level according to the chi-square test.
The most important findings of this study are: the significant response rate (82%), which allows us to know and depict the practices of professionals who teach resuscitation in the delivery room in Brazil; the difficulty in choosing not to resuscitate children at the lower limit of the gray zone, at 23 weeks of gestation; the presence of a small percentage of pediatricians who do not resuscitate neonates in the delivery room whose viability is not questioned (26 weeks gestation); the extreme difficulty in the delivery room management for neonates with 24–25 weeks of gestation, with heterogeneous and not necessarily consistent opinions; and finally, the fact that the reported neonatal resuscitation practices are relatively uniform in Brazil from a regional point of view.
In a similar questionnaire on decisions made in the delivery room sent to neonatologists in the state of Illinois, United States, the response rate was 66%. Among the neonatologists who answered the questionnaire, 55% said they would not resuscitate a neonate born at 22 weeks of GA, as the upper resuscitation limit for 85% of these professionals would be 23–25 weeks.12 Those authors concluded that physicians, to decide on resuscitation in the delivery room, are influenced by the parents’ opinion as well as their own experience and opinion. Moreover, the fear of being sued and the ethical teachings during medical education also play an important role in this decision. Peerzada et al.,13 in 2006, reported that 94% of Swedish neonatologists who answered a questionnaire considered futile any treatment in neonates below 23 weeks of gestation and that resuscitation of those at 23 weeks had uncertain benefits, stating they would not follow the parents’ wishes if they wanted resuscitation. The findings of this study show a very different profile of the assessed pediatricians. Brazilian physicians have difficulty in making the decision not to start resuscitation, as 50% of resuscitation instructors would start resuscitation in a patient at 23 weeks, a fact that is in opposition to their own opinions, since 88% of them have previously considered that the GA limit for resuscitation should be around 24 weeks. This mismatch between what pediatricians say they practice and what they think is the ideal involves several issues, especially the lack of clear guidelines and criteria for the limitation of therapeutic efforts, in addition to the misperceptions that permeate answers that depend on concepts related to what is ethical, what is moral, and what is legal. Such behavior also seems to be the reality in South America, as Fajardo et al.14 showed in 2012 that, in Latin American countries, the usual practice is to provide intensive care and not to limit life support, differently from what is practiced in North America and Europe.
Regarding advanced resuscitation, there seems to be great dissent among the instructors who participated in the study in relation to providing chest compressions and medications to extreme preterm infants, as 45% of respondents would not perform advanced resuscitation in 23-week neonates, while 55% would perform the advanced procedures. Extremely preterm newborns who receive cardiopulmonary resuscitation in the delivery room have a 2.9- to 3.7-fold higher risk of death and 1.5- to 2.3-fold higher risk of severe neurological damage in relation the group of patients who do not need this intervention in the delivery room.15,16
It is also worth mentioning that, although there are no recommendations in this respect, fused eyelids and birth weight also guided the decision regarding resuscitation in the delivery room for several interviewees. Perhaps this is due to the fact that, in practice, GA is not accurately known in a significant number of cases, which means that pediatricians try to estimate it through parameters that, although inaccurate, approximately reflect extreme prematurity. Fused eyelids are present in approximately 20% of live births with GA between 24 and 27 weeks, and thus, this condition is not a good parameter for decision-making in the delivery room.17 Birth weight should also be considered with caution, as there is no direct association between weight and maturity of the newborn, with the obstetric estimate of fetal weight being accurate in only 15–20% of cases.18,19
Another interesting point observed in this study was related to where one should wait for the death of infants for whom the decision not to resuscitate was made. There is some difficulty for Brazilian pediatricians in keeping the newborn together with the parents in the delivery room, which is a guideline of the American Academy of Pediatrics.20 Such conduct may be due in part to the PRN-SBP guidelines, which recommend, when in doubt or when there is scarce data to make a decision, and especially when the GA is not known, that it is better to resuscitate in the delivery room and postpone the decision to limit therapy until later, when more data can be obtained to better support the decision.
Despite the wealth of information, the study has limitations, especially the fact that it is based on answers to a questionnaire and on hypothetical clinical cases, which may significantly differ from the professional's performance in a real-life scenario. Another issue is related to the choice of a questionnaire with closed answers on a subject in which the subtlety of speech may reflect wide variations in practice. Despite these limitations, this is the first study that discloses the opinions of Brazilian pediatricians regarding interventions early in life.
Moreover, even in the international scenario, the extremely high percentage of questionnaire responses and the fact that the respondents represent the entire population of opinion makers regarding neonatal resuscitation are points to be highlighted, and can be used for the development of clearer guidelines on the ethical dilemmas the pediatrician faces when treating newborns at the limit of viability.
This study represents an initial step to understand what pediatricians think and how they act in the delivery room. The questionnaire indicates that the resuscitation of extremely preterm newborns is permeated by ambivalence and contradictions. A frank and comprehensive debate on the subject during medical graduation, pediatric residency and neonatal fellowship is essential to provide a broader basis for the discussion and support of resuscitation decisions related to the beginning of life in the presence of borderline maturity conditions for extrauterine survival.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the PRN-SBP instructors for their important collaboration; the State Coordinators of PRN-SBP for encouraging local participation; and the Brazilian Society of Pediatrics for supporting the research in the context of the Neonatal Resuscitation Program.
Please cite this article as: Ambrósio CR, de Almeida MF, Guinsburg R. Opinions of Brazilian resuscitation instructors regarding resuscitation in the delivery room of extremely preterm newborns. J Pediatr (Rio J). 2016;92:609–15.
Study carried out at the Division of Neonatal Medicine, Department of Pediatrics, Escola Paulista de Medicina, Universidade Federal de São Paulo, São Paulo, SP, Brazil; and Neonatal Resuscitation Program, Sociedade Brasileira de Pediatria, São Paulo, SP, Brazil.