Gastroschisis is a defect of the abdominal wall, resulting in congenital evisceration and requiring neonatal intensive care, early surgical correction, and parenteral nutrition. This study evaluated newborns with gastroschisis, seeking to associate nutritional characteristics with time of hospital stay.
MethodsThis was a retrospective cohort study of 49 newborns undergoing primary repair of gastroschisis between January 1995 and December 2010. The newborns’ characteristics were described with emphasis on nutritional aspects, correlating them with length of hospital stay.
ResultsThe characteristics that influenced length of hospital stay were: (1) newborn small for gestational age (SGA); (2) use of antibiotics; (3) day of life when enteral feeding was started; (4) day of life when full diet was reached. SGA infants had longer length of hospital stay (24.2%) than other newborns. The length of hospital stay was increased by 2.1% for each additional day taken to introduce enteral feeding. However, slower onset of full enteral feeding acted as a protective factor, decreasing length of stay by 3.6%. The volume of waste drained by the stomach catheter in the 24h prior the start of enteral feeding was not associated with the timing of diet introduction or length of hospital stay.
ConclusionEarly start of enteral feeding and small, gradual increase of volume can shorten the use of parenteral nutrition. This management strategy contributes to reduce the incidence of infection and length of hospital stay of newborns with gastroschisis.
a gastrosquise é uma malformação da parede abdominal que resulta em evisceração congênita, e requer tratamento intensivo neonatal, correção cirúrgica precoce e nutrição parenteral. Investigou-se neste estudo os recém-nascidos com gastrosquise, procurando correlacionar as suas características nutricionais com o tempo da internação hospitalar.
Métodosestudo de coorte retrospectivo de 49 recém-nascidos submetidos à correção primária de gastrosquise no período de janeiro de 1995 a dezembro de 2010. As características dos neonatos foram descritas com ênfase nos aspectos nutricionais relacionando-as com o tempo de internação hospitalar.
Resultadosas características que influenciaram a duração da internação foram: 1) recém-nascidos pequenos para a idade gestacional (PIG); 2) uso de antibióticos; 3) dia de vida ao iniciar a dieta enteral; 4) dia de vida ao atingir a dieta plena. Recém-nascidos PIG tiveram maior tempo de internação (24,2%) que demais neonatos. O tempo de internação foi aumentado em 2,1% para cada dia a mais que se demorou a introduzir a dieta enteral. Entretanto, atingir mais lentamente o aporte pleno da dieta enteral agiu como fator protetor, diminuindo 3,6% no tempo de internação. O volume de resíduo drenado pelo cateter gástrico, nas últimas 24 horas antes do início da dieta enteral, não apresentou correlação com o momento da introdução da dieta, nem com a duração da hospitalização.
Conclusãoiniciar a dieta enteral precocemente, com aumento gradativo em pequenos volumes pode abreviar a duração da nutrição parenteral. Este manejo contribui para a diminuição da incidência de infecções e do tempo de hospitalização de recém-nascidos com gastrosquise.
In Brazil, in recent years, congenital abnormalities have become the second most important cause of infant mortality1 and have generated various morbidities that compromise these children's future quality of life.
Several factors have contributed to the decline in infant mortality rates in recent years. Among them are the advances in perinatal care, expansion of neonatal intensive care units, improved mechanical ventilation devices, use of parenteral nutrition, advances in pre- and postnatal diagnostic methods, and updated protocols for perinatal care. Thus, newborns with gastroschisis can currently achieve survival rates that surpass 90%, especially in developed countries.2
Nevertheless, the length of hospital stay is still a matter of concern. The high cost, the nutritional disability, and the complications, in addition to the family problems caused by them, make congenital malformations important issues to be identified and studied.
Newborns with gastroschisis have a defect in the anterior abdominal wall, unrelated to the umbilical cord, which results in the exteriorization of the abdominal viscera from the time of intrauterine life. A frequency of two to five cases of gastroschisis per 10,000 live births is estimated, with an upward trend in several countries over the last 20–30 years.3,4
The treatment of gastroschisis requires intensive care shortly after birth, surgical correction within the first hours of life, and parenteral nutrition. The main complications are due to intestinal dysfunction (paralytic ileus, obstruction, atresia, malrotation, adhesions, resection, short bowel), the length of hospital stay, and episodes of septicemia and malnutrition. Depending on the viscero-abdominal disproportion, surgical correction can be performed in a single procedure with primary closure of the abdominal wall, or using a staged technique, with the creation of an extra-abdominal silo, initially, to contain and temporarily protect the externalized viscera.5
The understanding of the nutritional aspects of these newborns and their impact on hospital stay allows the multidisciplinary team to establish strategies to decrease morbidity and mortality, as well as to establish nutritional approach protocols, concentrating on the volume of the offered nutrition and the time of its introduction.
The aim of this study was to identify and describe the profile of newborns with gastroschisis undergoing primary surgical correction and associate their nutritional characteristics with length of hospital stay.
MethodsA retrospective cohort study was conducted, including all newborns with gastroschisis undergoing primary surgical closure admitted at Maternidade Otto Cirne do Hospital das Clínicas da Universidade Federal de Minas Gerais (HC–UFMG) from January 1995 to December 2010.
The diagnosis was obtained by fetal ultrasonography and/or through the clinical examination at birth.
A total of 40,819 live births were identified through analysis of the Estudo Colaborativo Latino Americano de Malformações Congênitas (ECLAMC) (Latin-American Collaborative Study of Congenital Malformations), of which 4111 live births had malformations; of these, 89 had gastroschisis. A total of 49 patients, according to the identification found in the medical records and confirmed by the analysis carried out by the pediatric surgery team of HC–UFMG, had been submitted to primary closure. Newborns with genetic syndromes, those born of multiple pregnancies, those not born at HC–UFMG, and those with gastroschisis repaired using the staged technique were excluded from the study.
Variables related to the newborn were identified, such as gender, gestational age, classification in relation to gestational age and birth weight, Apgar score at 1 and 5min, presence of other malformations, location of the anatomical defect in relation to the umbilical cord, aspect of the externalized bowel loops (simple: no alterations; complex: necrosis, ischemia, perforation, stenosis and atresia), content of externalized viscera (only intestine or associated with other organs), the size of the abdominal wall defect, time until the surgery, whether bowel resection was performed in the first surgery, the need for further interventions during hospitalization, time of mechanical ventilation, number of antibiotic therapy cycles, use of muscle relaxant, and occurrence of hemodynamic instability (shock). Nutritional approach data were assessed, such as time of parenteral nutrition, day of life when the diet was initiated, volume of gastric residue in 24h before the start of the diet, day of life when full diet was reached, sodium and serum albumin measurement, whether or not enteral nutrition was interrupted after its start, weight at discharge, and weight at discharge/birthweight ratio.
A descriptive analysis was performed of newborn characteristics and nutritional aspects. The variables were submitted to univariate and multivariate analysis considering the time of the first hospitalization and its outcome (discharge or death).
R software®, version 3.0.3 for Windows (Microsoft®, WA, USA), was used for the univariate and multivariate analysis. The stepwise6 method was used to select the significant variables involved with length of hospital stay of newborns, whereas the forward method was used in the univariate analysis, considering a significance level of 25%. The Mann–Whitney test was used for the univariate analysis, and time was stratified until discharge over the categorical variables, whereas Spearman's correlation test was used to associate time until discharge with other quantitative variables.
The selected variables were used in the multiple Poisson regression, applying the backward method, with a level of significance of 5%. The final regression, after the backward and forward procedures, was termed stepwise Poisson regression. The quasi-likelihood method7,8 was used for the phenomena of over- or under-dispersion for model estimation, allowing the estimation of robust variance to these phenomena. Nagelkerke9 pseudo R2 was calculated for logistic regression, while R2 adjusted to log-linear models10 was calculated for Poisson regression.
This study was approved by the Ethics Committee of UFMG.
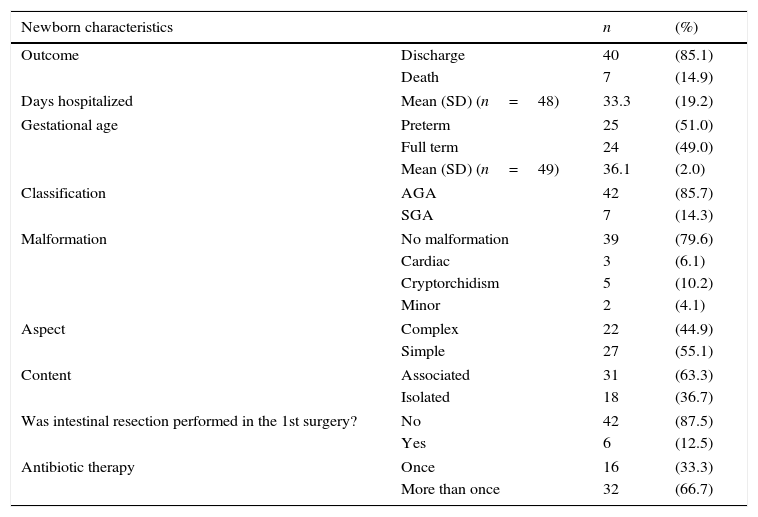
ResultsThe characteristics of newborns with gastroschisis submitted to primary closure and the variables related to their nutritional status are shown in Table 1.
Frequency and descriptive measures of the characteristic variables of neonates with gastroschisis and nutritional aspects, from January 1995 to December 2010.
| Newborn characteristics | n | (%) | |
|---|---|---|---|
| Outcome | Discharge | 40 | (85.1) |
| Death | 7 | (14.9) | |
| Days hospitalized | Mean (SD) (n=48) | 33.3 | (19.2) |
| Gestational age | Preterm | 25 | (51.0) |
| Full term | 24 | (49.0) | |
| Mean (SD) (n=49) | 36.1 | (2.0) | |
| Classification | AGA | 42 | (85.7) |
| SGA | 7 | (14.3) | |
| Malformation | No malformation | 39 | (79.6) |
| Cardiac | 3 | (6.1) | |
| Cryptorchidism | 5 | (10.2) | |
| Minor | 2 | (4.1) | |
| Aspect | Complex | 22 | (44.9) |
| Simple | 27 | (55.1) | |
| Content | Associated | 31 | (63.3) |
| Isolated | 18 | (36.7) | |
| Was intestinal resection performed in the 1st surgery? | No | 42 | (87.5) |
| Yes | 6 | (12.5) | |
| Antibiotic therapy | Once | 16 | (33.3) |
| More than once | 32 | (66.7) | |
| Nutritional aspects of the newborn | n | (%) | |
|---|---|---|---|
| Time of parenteral nutrition | Not assessed | 4 | (8.3) |
| ≤22 | 31 | (64.6) | |
| >22 | 13 | (27.1) | |
| Mean (SD) (n=44) | 22.0 | (10.9) | |
| Day of life when enteral nutrition was started | Not assessed | 3 | (6.2) |
| ≤12 | 25 | (52.1) | |
| >12 | 20 | (41.7) | |
| Mean (SD) (n=45) | 12.4 | (4.4) | |
| Gastric residue | Not assessed | 3 | (6.4) |
| ≤25mL | 27 | (57.4) | |
| >25mL | 17 | (36.2) | |
| Mean (SD) (n=44) | 25.1 | (26.6) | |
| Day of life when full diet was reached | Not assessed | 6 | (12.5) |
| ≤23 | 28 | (58.3) | |
| >23 | 14 | (29.2) | |
| Mean (SD) (n=42) | 22.9 | (8.4) | |
| Serum Na+ measurement (mEq/mL) | Mean (SD) (n=48) | 126.8 | (4.9) |
| Albumin measurement (g/dL) | Mean (SD) (n=17) | 2.4 | (0.6) |
| Interrupted the diet after it was started | No | 35 | (72.9) |
| Yes | 13 | (27.1) | |
| Weight | Mean (SD) (n=49) | 2,414.0 | (552.1) |
| Weight at discharge | Mean (SD) (n=46) | 2,790.9 | (571.1) |
| Discharge weight/birth weight ratio | Gained | 39 | (84.8) |
| Lost | 7 | (15.2) | |
| Mean (SD) (n=46) | 1.18 | (0.19) | |
Seven newborns who died were identified, corresponding to 14.9% of the newborns. The mean length of hospital stay was 33.3 days.
Regarding the classification of weight in relation to gestational age, 14.3% of the newborns were classified as small for gestational age (SGA) and 85.7% were classified as adequate for gestational age (AGA).
Considering that all neonates with gastroschisis receive at least one initial course of antibiotics during hospitalization, 66.7% of infants in this study received more than one antibiotic therapy cycle.
The parenteral nutrition time of 64.6% of the newborns was ≤22 days. Gastric residue was ≤25mL in the last 24h before the start of enteral nutrition in 57.4% of newborns. As for the age of start of enteral feeding, 52.1% of newborns started enteral diet until the 12th day of life, and 58.3% of the newborns reached full diet within an average of 23 days.
The mean value found for serum Na+ was 126.8mEq/mL, whereas the mean value for serum albumin levels was 2.4g/dL.
In 27.1% of the infants, enteral nutrition was interrupted after its start due to abdominal distension, bilious vomiting, or bowel movement interruption. Regarding the weight, 15.2% of newborns had weight loss from birth until discharge or death.
Newborns who died very early, even before the period of parenteral and enteral nutrition introduction, could not have their nutritional characteristics assessed and were excluded from the analysis. At 13 days of life, 90% of the newborns were alive, whereas at 30 days, at least 50% of the infants were still hospitalized.
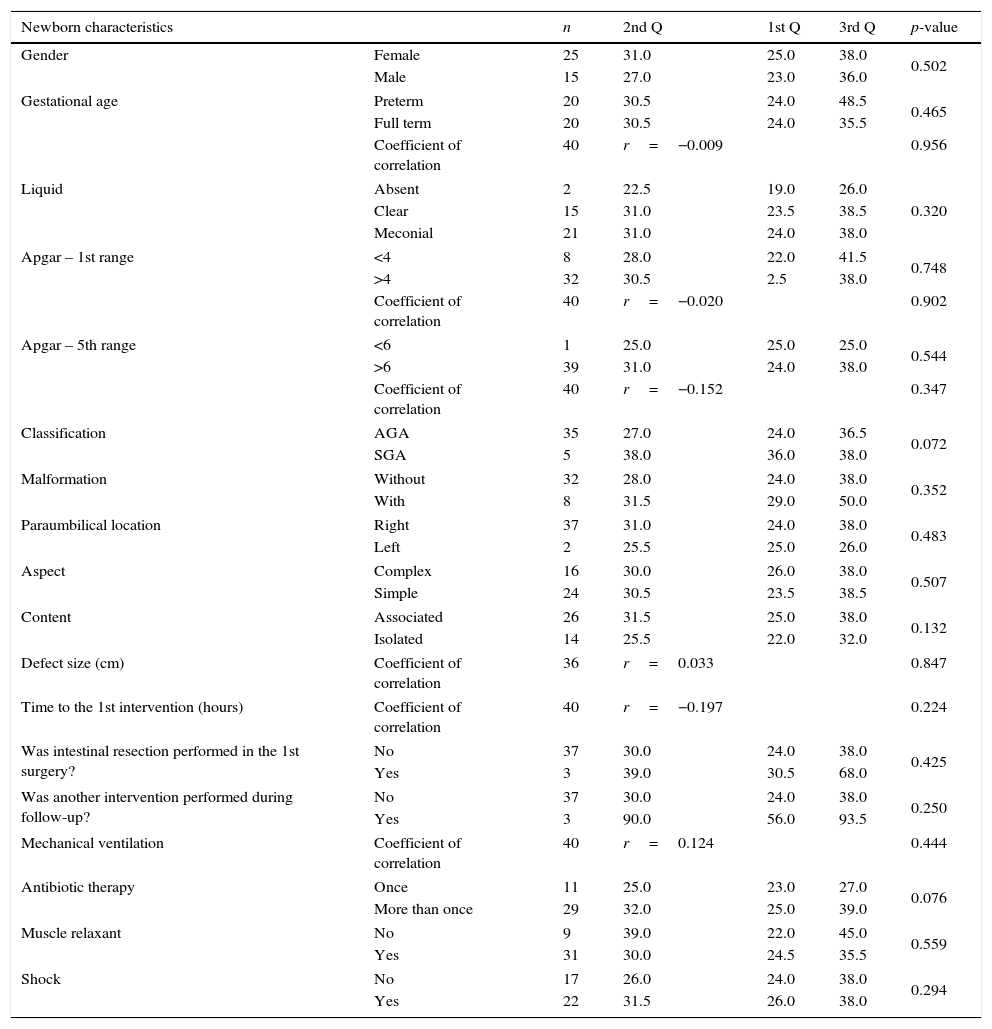
At the hospital stay analysis, the results were arranged according to the newborn and nutritional characteristics (Table 2).
Univariate analysis of the characteristics of newborns with gastroschisis, from January 1995 to December 2010.
| Newborn characteristics | n | 2nd Q | 1st Q | 3rd Q | p-value | |
|---|---|---|---|---|---|---|
| Gender | Female | 25 | 31.0 | 25.0 | 38.0 | 0.502 |
| Male | 15 | 27.0 | 23.0 | 36.0 | ||
| Gestational age | Preterm | 20 | 30.5 | 24.0 | 48.5 | 0.465 |
| Full term | 20 | 30.5 | 24.0 | 35.5 | ||
| Coefficient of correlation | 40 | r=−0.009 | 0.956 | |||
| Liquid | Absent | 2 | 22.5 | 19.0 | 26.0 | 0.320 |
| Clear | 15 | 31.0 | 23.5 | 38.5 | ||
| Meconial | 21 | 31.0 | 24.0 | 38.0 | ||
| Apgar – 1st range | <4 | 8 | 28.0 | 22.0 | 41.5 | 0.748 |
| >4 | 32 | 30.5 | 2.5 | 38.0 | ||
| Coefficient of correlation | 40 | r=−0.020 | 0.902 | |||
| Apgar – 5th range | <6 | 1 | 25.0 | 25.0 | 25.0 | 0.544 |
| >6 | 39 | 31.0 | 24.0 | 38.0 | ||
| Coefficient of correlation | 40 | r=−0.152 | 0.347 | |||
| Classification | AGA | 35 | 27.0 | 24.0 | 36.5 | 0.072 |
| SGA | 5 | 38.0 | 36.0 | 38.0 | ||
| Malformation | Without | 32 | 28.0 | 24.0 | 38.0 | 0.352 |
| With | 8 | 31.5 | 29.0 | 50.0 | ||
| Paraumbilical location | Right | 37 | 31.0 | 24.0 | 38.0 | 0.483 |
| Left | 2 | 25.5 | 25.0 | 26.0 | ||
| Aspect | Complex | 16 | 30.0 | 26.0 | 38.0 | 0.507 |
| Simple | 24 | 30.5 | 23.5 | 38.5 | ||
| Content | Associated | 26 | 31.5 | 25.0 | 38.0 | 0.132 |
| Isolated | 14 | 25.5 | 22.0 | 32.0 | ||
| Defect size (cm) | Coefficient of correlation | 36 | r=0.033 | 0.847 | ||
| Time to the 1st intervention (hours) | Coefficient of correlation | 40 | r=−0.197 | 0.224 | ||
| Was intestinal resection performed in the 1st surgery? | No | 37 | 30.0 | 24.0 | 38.0 | 0.425 |
| Yes | 3 | 39.0 | 30.5 | 68.0 | ||
| Was another intervention performed during follow-up? | No | 37 | 30.0 | 24.0 | 38.0 | 0.250 |
| Yes | 3 | 90.0 | 56.0 | 93.5 | ||
| Mechanical ventilation | Coefficient of correlation | 40 | r=0.124 | 0.444 | ||
| Antibiotic therapy | Once | 11 | 25.0 | 23.0 | 27.0 | 0.076 |
| More than once | 29 | 32.0 | 25.0 | 39.0 | ||
| Muscle relaxant | No | 9 | 39.0 | 22.0 | 45.0 | 0.559 |
| Yes | 31 | 30.0 | 24.5 | 35.5 | ||
| Shock | No | 17 | 26.0 | 24.0 | 38.0 | 0.294 |
| Yes | 22 | 31.5 | 26.0 | 38.0 | ||
AGA, adequate for gestational age; SGA, small for gestational age.
For the general characteristics related to newborns, no significant variable could be associated to hospital length of stay.
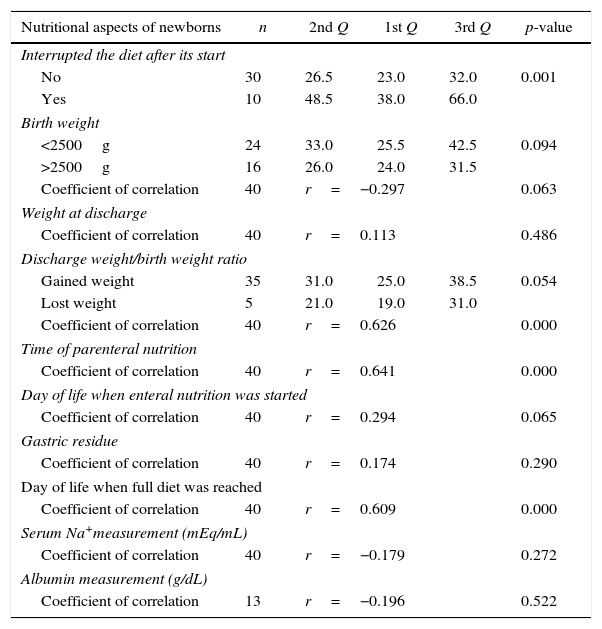
Regarding the assessed nutritional aspects, it was possible to identify the following variables (with significant value, p<0.05) to explain the length of hospital stay: “Interrupted the enteral diet after its start,” “Weight at discharge/birth weight ratio,” “Parenteral nutrition time,” and “Day of life when the newborn reached full diet” (Table 3).
Univariate analysis of variables related to the nutritional aspects of neonates with gastroschisis, from January 1995 to December 2010.
| Nutritional aspects of newborns | n | 2nd Q | 1st Q | 3rd Q | p-value |
|---|---|---|---|---|---|
| Interrupted the diet after its start | |||||
| No | 30 | 26.5 | 23.0 | 32.0 | 0.001 |
| Yes | 10 | 48.5 | 38.0 | 66.0 | |
| Birth weight | |||||
| <2500g | 24 | 33.0 | 25.5 | 42.5 | 0.094 |
| >2500g | 16 | 26.0 | 24.0 | 31.5 | |
| Coefficient of correlation | 40 | r=−0.297 | 0.063 | ||
| Weight at discharge | |||||
| Coefficient of correlation | 40 | r=0.113 | 0.486 | ||
| Discharge weight/birth weight ratio | |||||
| Gained weight | 35 | 31.0 | 25.0 | 38.5 | 0.054 |
| Lost weight | 5 | 21.0 | 19.0 | 31.0 | |
| Coefficient of correlation | 40 | r=0.626 | 0.000 | ||
| Time of parenteral nutrition | |||||
| Coefficient of correlation | 40 | r=0.641 | 0.000 | ||
| Day of life when enteral nutrition was started | |||||
| Coefficient of correlation | 40 | r=0.294 | 0.065 | ||
| Gastric residue | |||||
| Coefficient of correlation | 40 | r=0.174 | 0.290 | ||
| Day of life when full diet was reached | |||||
| Coefficient of correlation | 40 | r=0.609 | 0.000 | ||
| Serum Na+measurement (mEq/mL) | |||||
| Coefficient of correlation | 40 | r=−0.179 | 0.272 | ||
| Albumin measurement (g/dL) | |||||
| Coefficient of correlation | 13 | r=−0.196 | 0.522 | ||
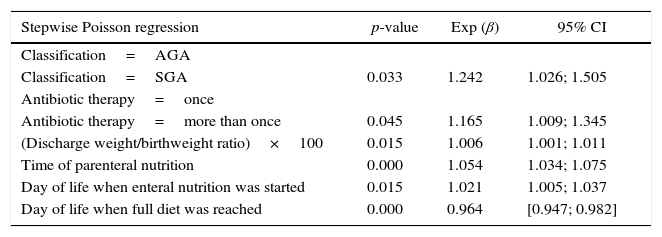
Subsequently, these variables were applied in multiple Poisson regression; the regression model is shown in Table 4.
Stepwise Poisson regression analysis with robust variance for hospital stay of newborns with gastroschisis, from January 1995 to December 2010.
| Stepwise Poisson regression | p-value | Exp (β) | 95% CI |
|---|---|---|---|
| Classification=AGA | |||
| Classification=SGA | 0.033 | 1.242 | 1.026; 1.505 |
| Antibiotic therapy=once | |||
| Antibiotic therapy=more than once | 0.045 | 1.165 | 1.009; 1.345 |
| (Discharge weight/birthweight ratio)×100 | 0.015 | 1.006 | 1.001; 1.011 |
| Time of parenteral nutrition | 0.000 | 1.054 | 1.034; 1.075 |
| Day of life when enteral nutrition was started | 0.015 | 1.021 | 1.005; 1.037 |
| Day of life when full diet was reached | 0.000 | 0.964 | [0.947; 0.982] |
Pseudo R2=82.67%.
AGA, adequate for gestational age; SGA, small for gestational age.
Using pseudo R2 (multiple regression), it was observed that 82.7% of the total variability of length of hospital stay until discharge was explained by the variables: “Classification,” “Antibiotic therapy,” “Discharge weight/birthweight ratio,” “Parenteral nutrition time,” “Day of life when neonate started enteral nutrition,” and “Day of life when neonate reached full diet.”
Newborns classified as SGA had a mean length of hospital stay 24.2% longer than the infants who were classified as AGA. Those who received more than one antibiotic cycle showed a mean length of stay 16.5% longer than newborns that underwent only one cycle.
For each extra day before starting enteral feeding, the mean length of stay increased by 2.1%.
For each extra day before reaching full diet, the mean hospital stay decreased by 3.6%.
For each extra day receiving parenteral nutrition time, the mean time from admission to discharge increased by 5.4%.
DiscussionIn this study, the most relevant characteristics that influenced the length of hospital stay of newborns were: (1) weight classification for gestational age (SGA newborns); (2) use of two or more antibiotic cycles during hospitalization; (3) the association between the newborn's weight at discharge and the newborn's birth weight; (4) time of parenteral nutrition administration; (5) day of life when the newborn started enteral nutrition; (6) day of life when the newborn reached full diet; (7) the interruption of enteral diet.
Adequate fetal growth, especially in late pregnancy, depends on the normal function of the gastrointestinal tract, which may not occur in gastroschisis.11 In this study, the mean length of hospital stay of newborns classified as SGA was higher than in AGA newborns.
It is known that one of the common complications among newborns with gastroschisis is intrauterine growth restriction (IUGR),12 which manifests as low birth weight (≤2500g).11 The lower fetal growth can be influenced by loss of nutrients and proteins through the intestinal exposure to amniotic fluid, with a secondary nutritional deprivation13 causing a lower tolerance to the progression of enteral feeding, requiring longer time of parenteral nutrition and thus, longer hospital stays.
This study did not identify a higher number of newborns with gastroschisis classified as SGA; however, they had longer hospital stay, in contrast to the findings of Puligandla et al.,12 who did not observe any differences in the outcome of the SGA newborns regarding several characteristics, including length of hospital stay.
The mean length of stay of newborns who received more than one cycle of antibiotic therapy was longer than those who received only one in the present study. The use of antibiotics in infants with gastroschisis is aimed toward reducing the contamination of the externalized bowel.5 The use of more than one cycle of antibiotics is related to the higher number of infections affecting the newborn. The occurrence of infection in the neonatal period is directly related to the delay in diet introduction, and the prolonged time of total parenteral nutrition and central venous access devices.
Also, the higher the ratio between the discharge weight and birth weight, the longer the length of hospital stay. This occurs because the neonate with longer hospitalization gains more weight while undergoing hospital care, reflecting the adequacy of nutritional support during hospitalization.
Additionally, the longer the duration of parenteral nutrition, the longer the hospital length of stay. The typical duration of parenteral nutrition until the final outcome is 28 days, as seen in the study by Islam.3 In three analyzed studies,14–16 the mean time to full enteral feeding was between 17 and 42 days, with a mean hospital stay between 24 and 67 days.4 In the present study, the mean length of stay was 33 days and the time to reach full diet was, on average, 22 days of life.
In this study, newborns who had intolerance to enteral nutrition after its start, (manifested by abdominal distention, vomiting, massive bilious gastric stasis, and interruption/decrease of gases and feces elimination) had longer hospital stays, compared to newborns that had no interruption of the enteral diet administration.
Parenteral nutrition is an important survival factor in the early days of these neonates. However, its prolonged use is associated with increased risk of infections and adverse effects on the liver (cholestasis, jaundice, increase in liver enzymes and direct bilirubin).17
A longer length of hospital stay is observed in gastroschisis due to complications and associated morbidities, increasing hospital medical costs and affecting the family life of these neonates.
It is noteworthy that delay in the introduction of enteral feeding becomes a factor that increases the length of hospital stay of these neonates; however, after diet introduction, the supply of the total required volume should not be accelerated. A slow increase in the diet volume is suggested each day, as rapid increases in volume are not favorable. This has also been demonstrated by the studies performed by Walter-Nicolet et al.18 These authors stated that the introduction of early minimal enteral diet (low volume provided at the same rate for at least five days) can promote the growth of intestinal mucosa, optimize the maturation of intestinal muscle function, increase the release of hormones and local peptides, and alter the intestinal flora. Thus, enteral nutrition management helps to reduce complications of parenteral nutrition and accelerate the tolerance to enteral nutrition.
This study showed that newborns started the enteral diet with varying amounts of gastric residue; this variable was not significant for the outcome. Therefore, the start of enteral diet should not be delayed based solely on the volume or bilious aspect of gastric drainage.
Other authors have also studied the impact of early enteral nutrition in the postoperative outcome of newborns with gastroschisis.19,20 Aljahdali et al.19 observed a better evolution when diets were initiated seven days after the abdominal wall closure. Sharp et al.20 found that for every day of delay of the start of enteral nutrition, there was an increase in the length of stay of 1.05 days and an increase in the duration of enteral nutrition of 1.06 days.
In this study, the best outcomes were obtained in neonates who started enteral nutrition within 12 days of life. Arnon et al.21 stated that SGA newborns benefited from early enteral nutrition (beginning within the first 24h of life), resulting in lower hospital stay when compared to infants who started the diet later.
Several studies have aimed to evaluate the importance of hydration status and serum sodium measurement and its management, as well as the degree of malnutrition (hypoalbuminemia) in patients with gastroschisis with the outcome observed in these patients.17,22,23 In the present study, the occurrence of hyponatremia and hypoalbuminemia related to the severity and the degree of initial hypercatabolism of the newborn did not correlate with hospital stay. Data on albumin measurement was found for only 17 infants, showing that in the HC–UFMG, until 2010, the evaluation of this parameter was not part of routine care for newborns with gastroschisis. The failure to complete the medical records with this information is a limiting factor, making it difficult to attain a better evaluation.
Although this study was conducted with a 16-year cohort, the number of patients involved was small, which hinders the extension of the results to other populations. Furthermore, the involvement of a single study center contributes to the small sample, even considering the increasing prevalence of gastroschisis in recent years.
An important bias to be considered is the fact that data collection was obtained from non-electronic and non-standardized medical records. In this type of collection, the information is scattered in the file and absent in some cases, as it depends on the examiner's notes at the time the events occurred.
The decision to study patients with gastroschisis submitted only to primary surgical closure was made in an attempt to identify factors related to the length of stay specific for this group of infants, who are more likely to receive early enteral feeding, as they do not require a second surgical procedure, characteristic of the staged correction.
The mortality rate of newborns with gastroschisis is low, between 5% and 10%, as shown by Snyder24 and Drive et al.25 However, in this study, mortality was higher (14.9%) when compared with the results from developed countries.24,25 In the seven newborns who died, this outcome occurred very early, before the seventh day of life, and thus, there was not enough time to assess the implemented nutritional measures.
In conclusion, this study demonstrates that the earlier enteral diet is started (≤12 days) and the slower full enteral feeding is reached (>23 days), the better the prognosis of the newborn and the shorter the hospital length of stay. The authors emphasize the importance of small, gradual volume increases to improve the newborn's tolerance to the diet.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Miranda da Silva Alves F, Miranda ME, de Aguiar MJ, Bouzada Viana MC. Nutritional management and postoperative prognosis of newborns submitted to primary surgical repair of gastroschisis. J Pediatr (Rio J). 2016;92:268–75.