To evaluate the differences in hospital survival between modes of transport to a tertiary center in Colombia for critically ill neonates.
MethodsObservational study of seriously ill neonates transported via air or ground, who required medical care at a center providing highly complex services. Data on sociodemographic, clinical, the Transport Risk Index of Physiologic Stability (TRIPS), and mode of transport were collected. Patients were described, followed by a bivariate analysis with condition (live or dead) at time of discharge as the dependent variable. A multiple Poisson regression with robust variance model was used to adjust associations.
ResultsA total of 176 neonates were transported by ambulance (10.22% by air) over six months. The transport distances were longer by air (median: 237.5km) than by ground (median: 11.3km). Mortality was higher among neonates transported by air (33.33%) than by ground (7.79%). No differences in survival were found between the two groups when adjusted by the multiple model. An interaction between mode of transport and distance was observed. Live hospital discharge was found to be associated with clinical severity upon admittance, birth weight, hemorrhaging during the third trimester, and serum potassium levels when admitted.
ConclusionsMode of transport was not associated with the outcome. In Colombia, access to medical services through air transport is a good option for neonates in critical condition. Further studies would determine the optimum distance (time of transportation) to obtain good clinical outcomes according type of ambulance.
Avaliar as diferenças na sobrevida hospitalar entre os modos de transporte para um centro terciário na Colômbia para neonatos gravemente doentes.
MétodosEstudo observacional de neonatos gravemente doentes transportados por ar ou terra que precisam de cuidados médicos em um centro que oferece serviços altamente complexos. Foram coletados dados sociodemográficos, clínicos, sobre o Índice de Risco da Estabilidade Fisiológica no Transporte (TRIPS) e o meio de transporte. Os pacientes foram descritos e submetidos a uma análise bivariada, com a condição (vivo ou morto) no momento da alta sendo a variável dependente. Uma regressão múltipla de Poisson com modelo de variância robusta foi utilizada para ajustar as associações.
ResultadosUm total de 176 neonatos foram transportados por ambulância (10,22% pelo ar) ao longo de seis meses. As distâncias foram maiores pelo ar (mediana: 237,5 km) que por terra (mediana: 11,3 km). A mortalidade foi mais alta entre neonatos transportados pelo ar (33,33%) que por terra (7,79%). Não foram encontradas diferenças na sobrevida entre os dois grupos após o ajuste com o modelo múltiplo. Foi observada uma interação entre o meio de transporte e a distância. A alta hospitalar com vida foi associada à gravidade clínica na internação, ao peso ao nascer, à hemorragia durante o terceiro trimestre e aos níveis de potássio sérico na internação.
ConclusõesO meio de transporte não foi associado ao resultado. Na Colômbia, o acesso a serviços médicos por transporte aéreo é uma boa opção para neonatos em condições críticas. Estudos adicionais determinariam a distância ideal (tempo de transporte) para obter bons resultados clínicos de acordo com o tipo de ambulância.
Transportation is an important factor to ensure quality medical care for neonatal patients who do not have the opportunity to obtain optimal care or whose pathology is complex.1 This is because the infrastructure required to treat these patients is not always available in the areas where they are born. For a health system, effective ambulance services (ground and air) may provide a means to improve access to health services. It is important, because according to Campbell et al., access to clinical care and its effectiveness are the factors related to the quality of services.2
Worldwide, ambulance transport is the first line of response for inter-hospital referrals of critical patients. Many of these patients are transported by ground, while medical air transport services have been used for critical patients who require immediate care or when geographic difficulties limit access by ground.3 Several studies regarding air transport have been conducted in developed countries – primarily in the United States, Canada, and Europe – nevertheless, evidence about this topic is scarce in developing countries.4 In these countries, social difficulties are related to large inequities in health services. Additionally, geographic characteristics could limit the provision of health services, including primary care.5
To address these problems with geographic accessibility, countries such as the United States have developed policies directed toward efforts to improve access and eliminate disparities in health care, with efficiency as the priority.6 Examples like this are not suitable for Colombia. In this country, three mountain ranges run through country, making the distances between the regions longer than in other nations when traveled by ground. In addition, a recent study of roadway conditions in Colombia reported the existence of 128,000km of roads in the country (75% paved), only 35% of which were found to be in good condition.7 Furthermore, during the rainy season roadways are frequently blocked by landslides and floods. It was especially problematic during 2010 and 2011 when La Niña caused a great deal of deterioration in roadway infrastructure,8 making it difficult to transport some patients who required specialized medical care at more complex hospitals. All these reasons favor the option of air transportation. In health services, the air transportation of patients to main cities (Bogotá and Medellín) is relatively frequent in commercial airlines,9 but specialized air ambulances are scarce.
To improve health indicators, the mode of transport and the expertise of the transport team need to be considered as a means to shorten transport time and optimize the clinical stability of patients. In Colombia, at the moment of this study, ground and air transportation did not have contractual relationships with receiving hospitals, and specialized physicians and nurses were available exclusively in air transportation. The mode of transport is more relevant for critical neonatal patients referred to hospitals with a high level of complexity. Moreover, data from around the world indicate that neonatal mortality has decreased more slowly than the mortality of mothers and of children between 1 month and 5 years of age, and is even more problematic in countries with higher burden of disease. Therefore, the evaluation of factors that determine survival, such as mode of transport, is a variable that should be explored in developing countries.
In a previous study the authors explored the clinical variables associated with intra-hospital mortality, but did not investigate factors related to access.10 The present study explores whether air or ground transport and distance traveled between the referring location and the specialized hospital are associated with the hospital survival of critically-ill neonates in Northeastern Colombia. Given its geographical characteristics, this region is a good example of limited access.11
MethodsAn observational study was performed to compare hospital survival of all ill neonates transported to the Fundación Cardiovascular de Colombia (FCV, Spanish acronym) by ground and air over a period of six months. This was a convenience sample adequate to explore large differences between types of ambulance transportation. The data collected and included in the study were obtained from electronic institutional records and a file with additional variables, designed ad hoc. All the participating neonates were hospitalized in the Neonatal Intensive Care Unit. The FCV is a private institution which provides highly complex services to patients with cardiovascular, neurological, and perinatal illnesses, or who require transplants. This institution is accredited by the Joint International Commission. The study was approved by the Ethics Committee of the FCV.
VariablesThe outcome variable was discharge from the hospital alive (yes/no). The independent variables included clinical and sociodemographic data and information related to the municipality from which the neonates were referred. The clinical variables were: gestational age (weeks), weight (g), sex (male/female), Apgar score, heart rate (beats/min), blood pressure (mmHg) and acid–base status (pH) at the time of admission. Other variables evaluated were congenital defects (yes/no), cardiopathies (yes/no), brain hemorrhage (yes/no), kidney failure (yes/no, ≥1.5mg/dL), and degree of severity after transport according to the Transport Risk Index of Physiologic Stability (TRIPS).12 These data were obtained from the analysis performed in the hospital.
Information was also obtained about the type of social security (contributory, subsidized, or uninsured), human resources in the ambulance (general practitioner, rural, specialist physician, registered nurse, auxiliary nurse, or other), type of ventilation support (hood chamber, nasal cannula, ventilator, or not required), use of vasopressors in the ambulance during transport (yes/no), adverse events during transport (yes/no, type of event), and originating municipality. The latter was used to calculate driving distance (km) to the hospital with the free tool http://distancescalculator.com/. Data related to age, clinical background, and prenatal maternal controls were also obtained.
Statistical methodsFirst, variables were described with percentages or central tendency and dispersion measures, according to the distribution observed for each variable. Then, for each of the independent variables, the chi-squared, Fisher's exact, or Mann–Whitney tests were used to compare patients discharged alive with those who had died. The modification effect of the interaction between type of ambulance (ground/air) and distance from the referring hospital to the FCV was evaluated, considering values of p<0.15 as statistically significant.13 Finally, Poisson regression with robust variance14 was used to estimate the association (prevalence ratios) between independent variables and the status (alive/dead) when discharged from the FCV. All analyses were performed with the statistical software Stata 13 (Stata Corporation, College Station, TX, EUA).
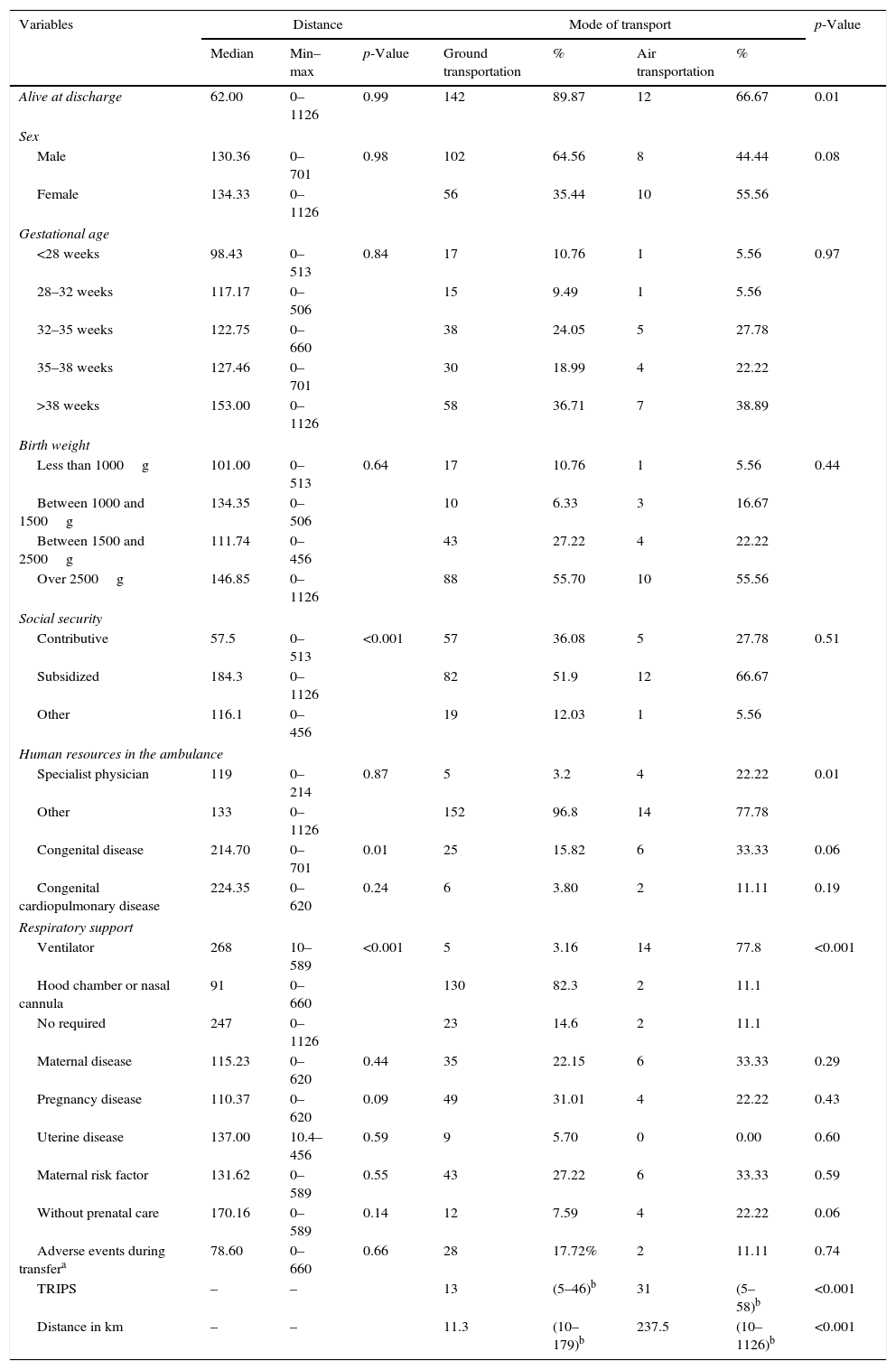
ResultsA total of 176 patients participated, 154 (87.5%) of whom were discharged alive. Of the total, 158 (89.87%) were transported via ground, with an outcome of 92.21% discharged alive. Of the 18 patients transported by air, 66.67% were discharged alive. Table 1 shows the characteristics of the patients according to the distances traveled in ambulance and the mode of transport. A difference was found in the distances traveled from the referring location to the FVC between patients with and without congenital diseases: ∼179km (Q25=10.4 and Q75=344) for the former and 11.3km (Q25=10.4 and Q75=214) for the latter. There was no difference for patients with congenital heart disease (p=0.19). Larger distances were observed among neonates with subsidized social security and those who did not require respiratory support.
Main characteristics of neonates included in the study, according mode of transport and distance between referring hospital to the Cardiovascular Foundation of Colombia.
| Variables | Distance | Mode of transport | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| Median | Min–max | p-Value | Ground transportation | % | Air transportation | % | ||
| Alive at discharge | 62.00 | 0–1126 | 0.99 | 142 | 89.87 | 12 | 66.67 | 0.01 |
| Sex | ||||||||
| Male | 130.36 | 0–701 | 0.98 | 102 | 64.56 | 8 | 44.44 | 0.08 |
| Female | 134.33 | 0–1126 | 56 | 35.44 | 10 | 55.56 | ||
| Gestational age | ||||||||
| <28 weeks | 98.43 | 0–513 | 0.84 | 17 | 10.76 | 1 | 5.56 | 0.97 |
| 28–32 weeks | 117.17 | 0–506 | 15 | 9.49 | 1 | 5.56 | ||
| 32–35 weeks | 122.75 | 0–660 | 38 | 24.05 | 5 | 27.78 | ||
| 35–38 weeks | 127.46 | 0–701 | 30 | 18.99 | 4 | 22.22 | ||
| >38 weeks | 153.00 | 0–1126 | 58 | 36.71 | 7 | 38.89 | ||
| Birth weight | ||||||||
| Less than 1000g | 101.00 | 0–513 | 0.64 | 17 | 10.76 | 1 | 5.56 | 0.44 |
| Between 1000 and 1500g | 134.35 | 0–506 | 10 | 6.33 | 3 | 16.67 | ||
| Between 1500 and 2500g | 111.74 | 0–456 | 43 | 27.22 | 4 | 22.22 | ||
| Over 2500g | 146.85 | 0–1126 | 88 | 55.70 | 10 | 55.56 | ||
| Social security | ||||||||
| Contributive | 57.5 | 0–513 | <0.001 | 57 | 36.08 | 5 | 27.78 | 0.51 |
| Subsidized | 184.3 | 0–1126 | 82 | 51.9 | 12 | 66.67 | ||
| Other | 116.1 | 0–456 | 19 | 12.03 | 1 | 5.56 | ||
| Human resources in the ambulance | ||||||||
| Specialist physician | 119 | 0–214 | 0.87 | 5 | 3.2 | 4 | 22.22 | 0.01 |
| Other | 133 | 0–1126 | 152 | 96.8 | 14 | 77.78 | ||
| Congenital disease | 214.70 | 0–701 | 0.01 | 25 | 15.82 | 6 | 33.33 | 0.06 |
| Congenital cardiopulmonary disease | 224.35 | 0–620 | 0.24 | 6 | 3.80 | 2 | 11.11 | 0.19 |
| Respiratory support | ||||||||
| Ventilator | 268 | 10–589 | <0.001 | 5 | 3.16 | 14 | 77.8 | <0.001 |
| Hood chamber or nasal cannula | 91 | 0–660 | 130 | 82.3 | 2 | 11.1 | ||
| No required | 247 | 0–1126 | 23 | 14.6 | 2 | 11.1 | ||
| Maternal disease | 115.23 | 0–620 | 0.44 | 35 | 22.15 | 6 | 33.33 | 0.29 |
| Pregnancy disease | 110.37 | 0–620 | 0.09 | 49 | 31.01 | 4 | 22.22 | 0.43 |
| Uterine disease | 137.00 | 10.4–456 | 0.59 | 9 | 5.70 | 0 | 0.00 | 0.60 |
| Maternal risk factor | 131.62 | 0–589 | 0.55 | 43 | 27.22 | 6 | 33.33 | 0.59 |
| Without prenatal care | 170.16 | 0–589 | 0.14 | 12 | 7.59 | 4 | 22.22 | 0.06 |
| Adverse events during transfera | 78.60 | 0–660 | 0.66 | 28 | 17.72% | 2 | 11.11 | 0.74 |
| TRIPS | – | – | 13 | (5–46)b | 31 | (5–58)b | <0.001 | |
| Distance in km | – | – | 11.3 | (10–179)b | 237.5 | (10–1126)b | <0.001 | |
TRIPS, Transport Risk Index of Physiologic Stability.
A difference was also found between the distances traveled by patients transported via ground vs. air, with a median of 11.3km (Q25=10.4 and Q75=174) for the former group and 237 (Q25=214 and Q75=506) for the latter (Fig. 1). This difference was related with geographic accessibility problems overcome only with air transportation. A TRIPS of 13 (Q25=6 and Q75=29) was observed for patients who traveled by ground and 31 (Q25=22 and Q75=39) for those who traveled by air, with significant differences. This was related to the fact that respiratory support was more utilized in air transport, where specialized physicians are more frequent. In general, more severe cases tended to be transported by air. Note that hospital survival was more frequently observed among patients transported by ground.
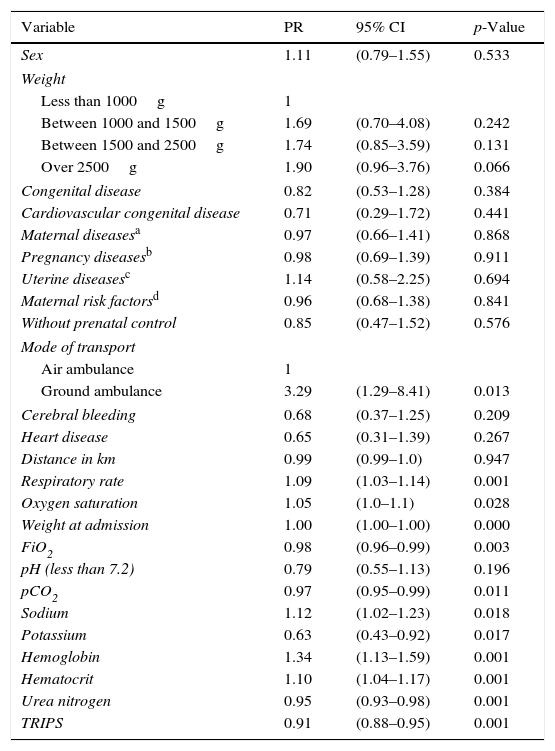
In the bivariate analysis (Table 2), associations were found between being discharged alive and birth weight, weight when admitted, respiratory frequency, oxygen saturation when admitted, respiratory acidemia, anemia, hypernatremia, hypokalemia, TRIPS, and kidney failure. The other variables studied (sociodemographic as well as clinical) were not significant. Normal potassium level upon admittance was also identified as a predictor of survival. In this sample, the median potassium level was 4mmol/L, while a value over 5mmol/L was found in only 10% of the patients, which was a population at risk of death.
Prevalence ratios (PR) between hospital survival discharge and independent variables.
| Variable | PR | 95% CI | p-Value |
|---|---|---|---|
| Sex | 1.11 | (0.79–1.55) | 0.533 |
| Weight | |||
| Less than 1000g | 1 | ||
| Between 1000 and 1500g | 1.69 | (0.70–4.08) | 0.242 |
| Between 1500 and 2500g | 1.74 | (0.85–3.59) | 0.131 |
| Over 2500g | 1.90 | (0.96–3.76) | 0.066 |
| Congenital disease | 0.82 | (0.53–1.28) | 0.384 |
| Cardiovascular congenital disease | 0.71 | (0.29–1.72) | 0.441 |
| Maternal diseasesa | 0.97 | (0.66–1.41) | 0.868 |
| Pregnancy diseasesb | 0.98 | (0.69–1.39) | 0.911 |
| Uterine diseasesc | 1.14 | (0.58–2.25) | 0.694 |
| Maternal risk factorsd | 0.96 | (0.68–1.38) | 0.841 |
| Without prenatal control | 0.85 | (0.47–1.52) | 0.576 |
| Mode of transport | |||
| Air ambulance | 1 | ||
| Ground ambulance | 3.29 | (1.29–8.41) | 0.013 |
| Cerebral bleeding | 0.68 | (0.37–1.25) | 0.209 |
| Heart disease | 0.65 | (0.31–1.39) | 0.267 |
| Distance in km | 0.99 | (0.99–1.0) | 0.947 |
| Respiratory rate | 1.09 | (1.03–1.14) | 0.001 |
| Oxygen saturation | 1.05 | (1.0–1.1) | 0.028 |
| Weight at admission | 1.00 | (1.00–1.00) | 0.000 |
| FiO2 | 0.98 | (0.96–0.99) | 0.003 |
| pH (less than 7.2) | 0.79 | (0.55–1.13) | 0.196 |
| pCO2 | 0.97 | (0.95–0.99) | 0.011 |
| Sodium | 1.12 | (1.02–1.23) | 0.018 |
| Potassium | 0.63 | (0.43–0.92) | 0.017 |
| Hemoglobin | 1.34 | (1.13–1.59) | 0.001 |
| Hematocrit | 1.10 | (1.04–1.17) | 0.001 |
| Urea nitrogen | 0.95 | (0.93–0.98) | 0.001 |
| TRIPS | 0.91 | (0.88–0.95) | 0.001 |
TRIPS, Transport Risk Index of Physiologic Stability.
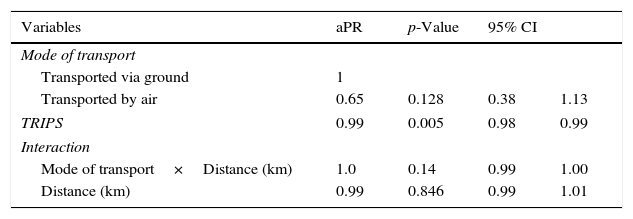
However, confounding could be present in these previous associations, and thus adjustment was required. Interestingly, no associations were found between type of ambulance and condition when discharged after adjusting the multifactorial model by TRIPS, birth weights, maternal hemorrhaging during the third trimester of pregnancy, and potassium concentrations. In addition, the analysis of the interaction between mode of transport and distance found evidence of a loss in the benefit from air transport at a certain distance (Table 3); unfortunately, this was not well defined by the data.
Adjusted prevalence ratios (aPR) for hospital survival discharge and mode of transport.
| Variables | aPR | p-Value | 95% CI | |
|---|---|---|---|---|
| Mode of transport | ||||
| Transported via ground | 1 | |||
| Transported by air | 0.65 | 0.128 | 0.38 | 1.13 |
| TRIPS | 0.99 | 0.005 | 0.98 | 0.99 |
| Interaction | ||||
| Mode of transport×Distance (km) | 1.0 | 0.14 | 0.99 | 1.00 |
| Distance (km) | 0.99 | 0.846 | 0.99 | 1.01 |
TRIPS, Transport Risk Index of Physiologic Stability.
This study did not find differences in the association of live discharge between neonates transported by air vs. ground. Although the bivariate analysis showed that more deaths occurred among those transported by air, no difference was found when adjusted for other variables. This paradox is intriguing, because interpretation requires considering that the original difference between types of ambulance was confounded. Thus, severe-illness neonates transported by air obtained a higher benefit and their risk of death was equal to that of neonates with less complicated diseases transported by ground.
Perinatal risk can be evaluated under ideal conditions, which enables predicting which neonates will require specialized care. Nevertheless, 40% of high-risk conditions will not be predictable and, therefore, a number of neonates may require inter-hospital transport in order to receive initial care or because of the complexity of the care required.15 Safety during transport of neonates has been of concern in developing countries, which can affect infant mortality. This is due to a lack of personnel with experience in neonate transport and can be related to adverse events such as hypothermia, hypoglycemia, and hypoxia.16 In addition, some studies have shown that mortality increases with travel time.17 It is thus important to determine stability conditions using TRIPS, which is a test that evaluates the physiological condition of neonates during transport and identifies the outcomes associated with the different transport teams.18 According to one recent study, temperature was the variable with greatest alterations in the TRIPS scale during transport.19
Nonetheless, other factors may influence the final outcome (mortality), such as the means of transport and travel time, in which distance and travel time may affect adverse outcomes. Although some studies have reported that outcomes depend on the experience of the team responsible for transport and not the distance,17 it is believed that in the case of Colombia, geographic conditions continue to represent an obstacle to obtaining quality of care. For example, in India maximum transport times and distances were 560min and 299km,17 while in the present study maximum transport time by ground was 1044min and maximum distance was 660km. This demonstrates differences in geography and/or the quality of roadways.
Given the distribution of the population and neonatal services in some developed countries, the use of air transport is known to be very uncommon.20 Meanwhile, the benefits in developing countries of transporting neonates by air have not been studied, where it could be considered an option to obtain better medical care. In addition, it may be difficult to receive timely care due to social conditions and differences in the quality of services among regions, as well as geographic conditions.
The above is applicable in a country such as Colombia where services are inequitable and distances are long. Data from developing countries indicate that several risk factors for perinatal mortality are related to poor access to health services and low quality (equity), thereby reinforcing the importance of improving accessibility and the quality of basic obstetric and neonatal care.21 Data also exist that suggest that the implementation of a transport system should be adapted to the geographic conditions of each country.22 While air transport can equalize intra-hospital outcomes, the analysis of the interaction between distance and mode of transport identifies a tendency in which patients referred from longer distances who travel by air are associated with a lower likelihood of being discharged alive.
In addition, the present study evaluated the maternal factors associated with survival, reported from the referring site, and found that hemorrhaging during the third trimester was the only protective factor for live discharge. While it is well known that this is a risk factor for maternal and neonatal morbid–mortality, the risks can be reduced if care is provided in a timely manner.23 Significant differences were observed when exploring the distribution of hemorrhaging according to gestational age. A tendency was found in which hemorrhaging during the third trimester was greater for gestational ages under 32 weeks. Nevertheless, this did not become an adverse factor. Therefore, it is believed that hemorrhaging can be quickly noted by the mother and thereby lead to a rapid search for medical care, resulting in better outcomes in spite of the premature condition.24 A study conducted in Peru about the warning signs that prompted emergency visits found that vaginal bleeding represented the highest percentage (87%) of visits, followed by decreased fetal movement and fever.25
The limitations of the study design should be taken into account when interpreting these findings. This was an observational study, which may contain biased results since clinical and therapeutic variables associated with the intra-hospital care received were not included. In addition, it was not possible to evaluate the clinical conditions at the referring site, preventing the verification of deterioration in conditions during transport. Also, patients were not evaluated by a clinical severity scale when admitted. This could have provided additional data regarding the severity of the condition when admitted and during the first hours in the unit.
It is possible that small sample size in this study did not permit identification of some predictors of hospital survival. However, it is important to remember that the main predictor was type of transportation, and better outcomes were observed during crude analysis among neonates transported by ground. The fact that this association disappeared in the adjusted analysis suggests that sample size was sufficient to explore the association of this variable. Another limitation was the need for long travel times via ground before reaching air transport services, with changes in altitude of as much as 600m, as well as the travel time from the airport to the health institution, which takes 45min in the city studied. Finally, this study did not evaluate adverse factors related with type of transportation, as did previous studies.26
Given the difficulties related to time, it would be worthwhile to perform studies with detailed records of travel time for each mode of transport. One recommendation by the authors is for institutions to consider the first moments of patient transport as the starting point for the provision of care by specialized personnel who are qualified in the field, in order to increase the speed of receiving care by an optimal team.
Differences were not found between air and ground transport in terms of live discharges from the neonatal unit. Transport systems should be established according to the needs of each region and the possibilities of the health system. Although Colombia is a developing country, the health system permits the use of air transportation no matter the type of health insurance or socioeconomic status. Air transport is an option for critical neonates or where geography makes access difficult. As consequence of findings of this study, FCV has implemented its own airplanes with a team of physicians and nurses specialized in air transportation.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Alvarado-Socarras JL, Idrovo AJ, Bermon A. Hospital survival upon discharge of ill-neonates transported by ground or air ambulance to a tertiary center. J Pediatr (Rio J). 2016;92:276–82.