Mucopolysaccharidosis is a rare genetic disease characterized by the intralysosomal deposition of glycosaminoglycans. Cardiovascular impairment is a common feature. Cardiac signs and symptoms are underestimated due to the disease involvement in other organs. Enzyme replacement therapy can be used in mucopolysaccharidosis I, II, IV, and VI. Thus, the knowledge about the use of new echocardiography tools is relevant to improve the care of this population. This study aimed to describe left ventricular function assessment by conventional echocardiography and left ventricular global longitudinal strain analysis and compare the alterations in patients receiving enzyme replacement therapy and who had different ages at the start of therapy.
MethodOutpatient-based descriptive study. The patients were submitted to conventional echocardiography and left ventricular global longitudinal strain measurement.
ResultsSixteen patients were evaluated; median age of 14.2 years (SD=5.2 years). Left ventricular hypertrophy was found in nine patients (56.2%). All patients had preserved left ventricular systolic function (Simpson and Teichholz). Nine (56.2%) patients showed alterations in left ventricular global longitudinal strain. The study showed a positive association between left ventricular hypertrophy and alteration in the left ventricular global longitudinal strain, and late start of enzyme replacement therapy and alteration in the left ventricular global longitudinal strain.
ConclusionEchocardiographic alterations in patients with mucopolysaccharidosis were frequently observed, especially alterations in the left ventricular geometry and subclinical dysfunction. Patients who had a late enzyme replacement therapy start showed an association with worse left ventricular global longitudinal strain values, reinforcing the need for early diagnosis and treatment. The use of new echocardiographic tools may improve the follow-up of these patients.
A mucopolissacaridose é uma doença genética rara, caracterizada por depósito intralisossômico de glicosaminoglicanos. O comprometimento cardiovascular é frequente. Sinais e sintomas cardíacos são subestimados pelo envolvimento da doença em outros órgãos. A terapia de reposição enzimática pode ser usada em mucopolissacaridose I, II, IV e VI. Assim, o conhecimento da aplicação de novas ferramentas de ecocardiografia é relevante para melhorar a assistência dessa população. Este estudo visou descrever a função do ventrículo esquerdo pelo ecocardiograma convencional e pela análise do strain global longitudinal do ventrículo esquerdo e comparar as alterações em pacientes que fazem uso da terapia de reposição enzimática e que tiveram idades distintas de início da terapia.
MétodoEstudo descritivo de base ambulatorial. Os pacientes foram submetidos à ecocardiografia convencional e medida do strain global longitudinal do ventrículo esquerdo.
ResultadosForam avaliados 16 pacientes; mediana de 14,2 anos (desvio: 5,2 anos). Hipertrofia do ventrículo esquerdo foi encontrada em nove pacientes (56,2%). Todos os pacientes tiveram função sistólica do ventrículo esquerdo preservada (Simpson e Teichholz). Nove (56,2%) pacientes apresentaram alteração no strain global longitudinal do ventrículo esquerdo. O estudo mostrou associação positiva entre hipertrofia do ventrículo esquerdo e alteração no strain global longitudinal do ventrículo esquerdo e início tardio da terapia de reposição enzimática e alteração no strain global longitudinal do ventrículo esquerdo.
ConclusãoAlterações ecocardiográficas em pacientes com mucopolissacaridose foram frequentes, especialmente alterações na geometria e disfunção subclínica do ventrículo esquerdo. Pacientes que iniciaram tardiamente a terapia de reposição enzimática apresentaram associação com piores valores de strain global longitudinal do ventrículo esquerdo, o que reforça a necessidade do diagnóstico e tratamento precoces. O uso de novas ferramentas de ecocardiografia pode melhorar o acompanhamento desses pacientes.
Mucopolysaccharidosis (MPS) is a rare genetic disease, with a worldwide incidence rate of 1:25,000 births. It is characterized as a lysosomal deposition disease due to the absence of a specific enzyme that degrades glycosaminoglycans (GAG), polymers that constitute the membrane and extracellular matrix. Thus, its intra- and extracellular accumulation is capable of generating dysfunction in several organs and tissues. There are seven types of MPS, and 11 enzymatic defects have been described, with each type being characterized by the deficiency of a specific enzyme.1
One of the frequently affected systems in MPS is the cardiovascular system. This impairment is progressive and limits patient quality of life, being considered one of the main causes of death in this population due to cardiac alterations caused by the accumulation of GAG in heart structures, such as valvular lesions, myocardial hypertrophy, coronary impairment, pulmonary hypertension, cardiac rhythm disorders, and systolic and diastolic dysfunctions.2 The cardiovascular symptoms and signs are scarce because of the disease involvement in the respiratory and skeletal systems, factors that limit clinical evaluation regarding physical activity tolerance – a sign of heart failure. The cognitive deficit present in some types of MPS also makes it difficult for the patient to perceive cardiac symptoms. Enzymatic Replacement Therapy (ERT) can be used in MPS type I, II, IV, and VI; its effect on cardiac alterations is still being studied. Hence the importance of imaging follow-up through echocardiography aiming to promote the early detection of cardiovascular alterations.3
The measurement of the myocardial strain through 2-Dimensional Speckle-Tracking Echocardiography (2D-STE) has been described in the literature as an accurate tool for detecting incipient myocardial injury, being important in the early diagnosis of subclinical cardiac dysfunction and prognosis in several heart diseases.4
The study aimed to describe left ventricular function through conventional echocardiographic measurements and also by Left Ventricular (LV) Global Longitudinal Strain (GLS) analysis by 2D-STE in patients with MPS, and compared the alterations found in the LV GLS in patients who received ERT and who started the therapy at different ages.
MethodsStudy design and patientsThis was a descriptive, cross-sectional, ambulatory-based study without a comparative group, carried out in patients with MPS (enzymatic diagnosis) followed at the Genetics Outpatient Clinic of Hospital Universitário Professor Edgard Santos of Faculdade de Medicina da Universidade Federal da Bahia (HUPES – UFBA). The inclusion criterion was that the patient must have attended at least one consultation at the Genetics Outpatient Clinic from January 2015 to May 2016. The exclusion criteria were presence of congenital heart disease or complication during the examination. The study was approved by the Research Ethics Committee of Instituto de Ciências da Saúde da UFBA in accordance with the Declaration of Helsinki, and all participants or patients’ legal guardians signed the informed consent.
EchocardiographyAll patients were evaluated by the same echocardiographer, who was blinded to the patients’ clinical condition. The exams were performed using the iE33 (Philips Medical Systems – Andover, MA, USA) apparatus with 5 and 8MHz transducers and following the recommendations of the American Society of Echocardiography. The patients were at rest and without sedation; electrocardiogram recording was performed concomitantly with the examination and all assessed patients were at an adequate heart rate for age, with no episodes of arrhythmia.
Conventional echocardiographyLV mass – it was calculated through the linear method (measurements of the interventricular septum, LV internal diameter, and left ventricular posterior wall thickness were performed at the end of diastole) and indexed by height raised to the exponential power of 2.7 (LVMI). Normal values for indexed mass: boys older than 9 years≤45g/m2.7 and girls older than 9 years≤40g/m2.7. In children younger than 9 years, values above the 95th percentile were considered altered (hypertrophy).5
LV systolic function – it was evaluated by calculating the ejection fraction (EF) using two parameters:
LV global longitudinal strainLeft ventricular (LV) global longitudinal strain (GLS) measurements were performed according to the protocol of the American Society of Echocardiography.6 Videos with good electrocardiographic tracing and approximately 60 to 80 frames per second were acquired in at least three consecutive cardiac cycles (none of the patients had arrhythmia during the examination). Stored videos should have good imaging quality. The analyses were performed offline, using QLAB (Philips Medical Systems – Andover, MA, USA) software. The endocardial borders were demarcated by the equipment, through the sequence of three points defined by the researcher in the endocardium. Fine contour adjustment of the endocardial borders was performed by the researcher. All patients had satisfactory images of the cardiac segments. For the evaluation of the LV GLS, videos were recorded of three echocardiographic windows (four, three, and two chambers). The value obtained through the average of the three slices was considered to be the LV GLS.
Reference values in children (younger than 21 years) followed those recommended by Levy et al. in 2016.8 As for patients older than 21 years, the reference values followed those recommended by Lang et al.6
Statistical analysisAs this is a descriptive study performed in a restricted population, the statistical analysis was performed through descriptive statistics relevant to the level of measurement of constant variables. Spearman's correlation coefficient was used for the constant comparisons.
Inter- and intraobserver reliability assessments were performed for LV GLS measurements. Five patients were randomly selected. The evaluations were performed one month after data collection was completed. For interobserver evaluation, the second investigator performed the LV GLS measurements offline, without prior knowledge of the previous echocardiogram. For the analysis of this evaluation, the Intraclass Correlation Coefficient (ICC) and respective 95% Confidence Intervals (95%CI) were used (for the quantitative variables).9 Inferential statistics were not calculated (except for the ICC), since the sampling plan included the assessment of all patients enrolled in the outpatient clinic and who attended at least one consultation at the genetics outpatient clinic from January 2015 to May 2016. The data were entered into Epidata software and the analyses were performed using the statistical package R, version 3.1.10
ResultsThe present study identified 20 patients with MPS who were followed at the HUPES/UFBA Genetics Outpatient Clinic and who attended at least one consultation from January 2015 to May 2016. Of this total, two patients were not included: one due to refusal to participate in the study and another for not having attended the cardiological evaluation after four attempts to schedule it, due to the presence of upper airway infection on the four scheduled dates.
Eighteen patients were submitted to cardiac evaluation, two of whom were excluded from the study: one due to a diagnosis of congenital heart disease (Patent Ductus Arteriosus – PDA) and another due to the presence of a complication during the examination (seizure). The patient with a PDA diagnosis was referred to a pediatric cardiology referral service in the state of Bahia for heart defect correction. Thus, the present study evaluated 16 patients.
The median age of the group was 14.2 years, with a SD of 5.2 years (1.5–22.6), of whom 12 (75%) were males. Five patients (31.2%) were from the municipality of Salvador and its metropolitan region, and the others from the countryside of the state, mainly from the Monte Santo region (56.2%), a municipality with a high incidence of genetic diseases due to the high rate of consanguineous marriages.11 The median age at the start of ERT was 8 years (SD=4.5 years) (1–14).
The following distribution was observed regarding MPS types: 3 (18.8%) patients with MPS type I, 4 (25%) patients with MPS type II, 1 (6.2%) with MPS type III, and 8 (50%) with MPS type VI.
Patients with MPS types I, II, IV, and VI can receive ERT. Of the 15 patients belonging to one of these four groups (I, II, and VI), 14 used ERT at the time of the echocardiographic evaluation. Only one patient from group I, who underwent the evaluation in the same month in which the MPS diagnosis was attained, did not use ERT at the time of the evaluation.
Left ventricular geometryThe study identified 9 (56.2%) patients with Left Ventricular Mass Increase (LVMI).
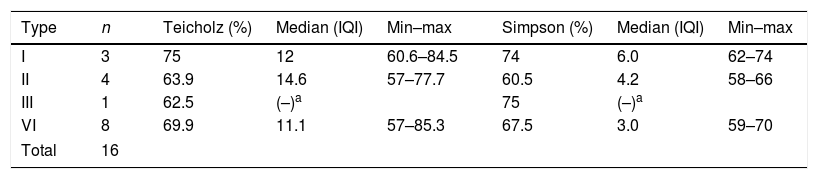
Left ventricular systolic function by conventional echocardiographyThe present study evaluated left ventricular systolic function by conventional echocardiography, considering the following parameters: Simpson and Teichholz methods. All patients evaluated in this series of cases had normal left ventricular systolic function according to these two parameters (Table 1).
Distribution of left ventricular function by conventional echocardiography according to MPS type.
| Type | n | Teicholz (%) | Median (IQI) | Min–max | Simpson (%) | Median (IQI) | Min–max |
|---|---|---|---|---|---|---|---|
| I | 3 | 75 | 12 | 60.6–84.5 | 74 | 6.0 | 62–74 |
| II | 4 | 63.9 | 14.6 | 57–77.7 | 60.5 | 4.2 | 58–66 |
| III | 1 | 62.5 | (–)a | 75 | (–)a | ||
| VI | 8 | 69.9 | 11.1 | 57–85.3 | 67.5 | 3.0 | 59–70 |
| Total | 16 | ||||||
MPS, mucopolysacardiosis; n, number of patients; EF, ejection fraction; IQI, interquartile interval; min–max, minimum–maximum.
Intra- and interobserver reproducibility analysis was performed regarding the LV GLS measurements, through calculation of the ICC, and a high level of agreement was found. For the intraobserver reproducibility analysis, the ICC was found to be 0.95 (95% CI: 0.58–0.99); and the inter-observer ICC was found to be 0.94 (95% CI: 0.66–0.99).
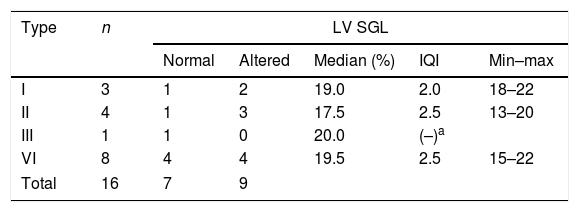
The LV GLS analysis showed that 56.2% of the assessed patients had altered measurements (Table 2). The median value was 19% (SD=2.2, 13%–22%).
Distribution of left ventricular GLS according to MPS type.
| Type | n | LV SGL | ||||
|---|---|---|---|---|---|---|
| Normal | Altered | Median (%) | IQI | Min–max | ||
| I | 3 | 1 | 2 | 19.0 | 2.0 | 18–22 |
| II | 4 | 1 | 3 | 17.5 | 2.5 | 13–20 |
| III | 1 | 1 | 0 | 20.0 | (–)a | |
| VI | 8 | 4 | 4 | 19.5 | 2.5 | 15–22 |
| Total | 16 | 7 | 9 | |||
GLS, global longitudinal strain; MPS, mucopolysacardiosis; n, number of patients; EF, ejection fraction; IQI, interquartile interval; min–max, minimum–maximum.
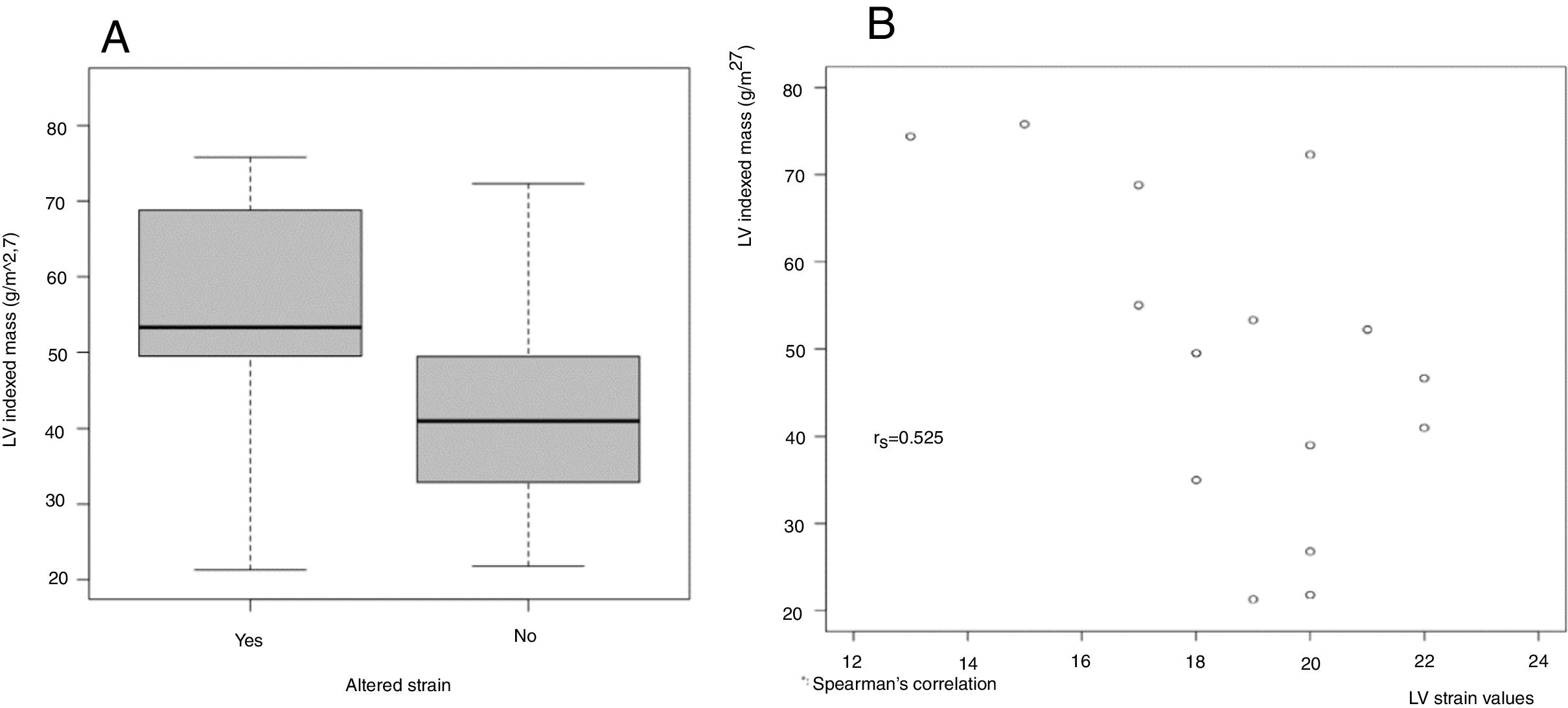
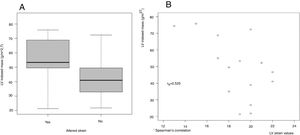
This study showed that patients with altered LV GLS measurements had higher LVMI values than patients with normal LV GLS values. A positive correlation (rs=0.502) was found between these two parameters, as shown in Fig. 1.
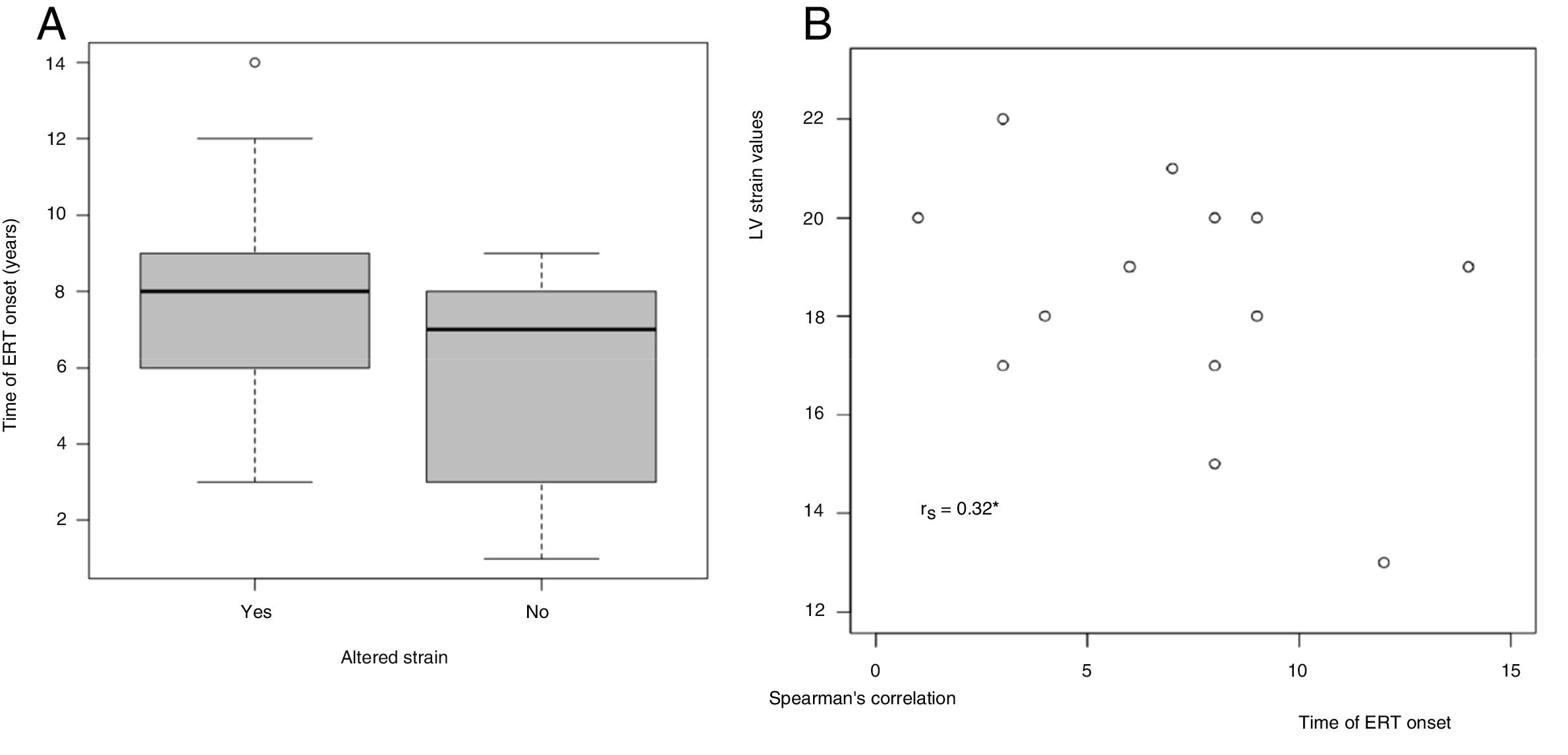
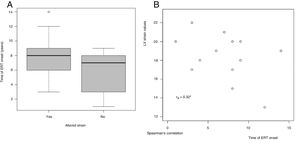
Association between time of enzyme replacement therapy start and left ventricular global longitudinal strainPatients who had altered LV GLS values had a later ERT start (patients with MPS types I, II, and VI).
The study showed a positive correlation (rs=0.320) between time of ERT start and LV GLS values, as shown in Fig. 2.
DiscussionIn 2013, Brands et al. studied the effects of ERT on 24 patients with MPS types I, II, and VI, and found that 70% of those who had left ventricular mass increase (12 patients, i.e., 50% of the assessed individuals), had LVMI normalization after at least one year of ERT.12
Lin et al. studied patients with MPS types I, II, IV, and VI who used ERT. After one year of enzymatic therapy, a statistically significant (p<0.01) reduction of LVMI was observed in patients who started ERT before 12 years of age (74.7g/m2±21 before ERT and 54.4g/m2±18.9 after ERT). This effect was not evident in patients who started ERT after the age of 12 years.13
These studies suggest that ERT is able to reduce left ventricular hypertrophy secondary to MPS by a probable reduction in GAG accumulation in the cardiac muscle, especially if initiated early. The present study showed that 9 (56.2%) patients had left ventricular hypertrophy. Median age at the start of ERT was 8 years. This fact possibly contributed to the high percentage of patients with left ventricular hypertrophy.
The study analyzed left ventricular systolic function using two conventional echocardiographic variables: Simpson and Teichholz. None of the assessed patients had left ventricular systolic dysfunction by any of these parameters. This result was consistent with other studies in the literature: Leal et al., in 2010, studied children with MPS without ERT use and Lin et al., in 2016, studied patients with MPS types I, II, IV, and VI before and after ERT use. A Dutch study, in 2013, showed a reduction in left ventricular systolic function in 3 (12.5%) of 24 patients studied before the start of ERT (MPS types I, II, and VI). After one year of ERT, two patients showed normal function and only one maintained systolic dysfunction, which was the same patient who also maintained diastolic dysfunction in the same study.12–14
The present study evaluated LV GLS and verified that, of the 16 assessed patients, 56.2% had altered GLS measurements. The literature is scarce regarding the evaluation of this parameter in patients with MPS. Few studies to date have used myocardial strain measurement as a parameter of ventricular function in this population.
In 2011, Harada et al. described the case of a 49 year-old woman with MPS type I before and after six months of enzyme replacement therapy with laronidase. There was an improvement in the LV GLS value during the period (13.2%–17.4%), whereas the ejection fraction measured by conventional echocardiography did not change. Additionally, the patient showed left ventricular mass reduction (189–152g), reduction in glycosaminoglycan levels in urine (75–38mg/g of creatinine), and reduction in hepatosplenomegaly (evaluated by computed tomography).15
In 2014, Lee et al. performed an experimental study in genetically modified mice with the model of cardiomyopathy associated with Hunter syndrome (MPS type II), before and after the use of ERT, and observed cardiac function improvement according to the circumferential and radial strain measurements at the end of the analyzed period (9.44%–12.41% and 16.91%–28.91%, respectively).16
In 2013, a Canadian study evaluated left ventricular systolic function through conventional echocardiography and myocardial strain by 2-dimensional speckle tracking in patients with Fabry disease, a multisystemic deposition disease (such as MPS) due to galactosidase A deficiency that can result in sequelae in several organs and systems, such as the kidneys, brain, and heart, due to protein deposition in tissues. All 16 studied patients had been receiving enzyme replacement therapy for a period longer than six years. All patients had normal left ventricular systolic function measured through EF measurement (mean of 63%), but the study reported a reduced mean LV GLS value in this population (16%), suggesting that this measure is more sensitive to the evaluation of systolic function in this group of patients.17
An Italian study in 2017 evaluated conventional echocardiographic aspects and myocardial deformation measures by two-dimensional speckle-tracking in 15 patients with MPS (types I, II, III, IV, and VI) and compared them with healthy controls. Ten patients were receiving ERT (mean: 6.5 years). MPS patients showed increased values of ventricular mass when compared to controls. All patients with MPS had adequate ventricular systolic function measurements by conventional echocardiography (Simpson) without any difference regarding the values found in patients from the control group. Patients with MPS had a reduction in global radial and circumferential strain measurements in relation to controls. Such a difference between the two groups was not observed for the global longitudinal strain. The study does not describe the age at the start of ERT in the studied population, only the average of use. Difference in this parameter could be a protective factor in the longitudinal myocardial fibers. More studies are required to better evaluate the changes in the three types of myocardial fiber deformation (longitudinal, radial, and circumferential strain) in patients with MPS.18
The present study verified a positive association between alterations in the LV GLS and left ventricular mass. Additionally, the late start of ERT also showed a positive association with altered values of LV GLS. Possibly, the late start of the enzyme replacement therapy may lead to increased GAG deposition and further cardiac sequelae, which justifies this subclinical dysfunction finding at the strain.
The present study showed significant cardiac alterations in patients with MPS, corroborating the importance of the cardiological follow-up in this population. Moreover, patients who had a late ERT start showed an association with worse values of LV global longitudinal strain, reinforcing the need for an early diagnosis and treatment.
Because it is a rare genetic disease, the results of the present study are limited to a small number of patients with MPS, and it is not possible to consider all described types of the pathology.
Many patients had thoracic deformities due to the impairment caused by the disease itself, which resulted in greater technical difficulty during the exams. Because the data were collected at a specific time for the study performance, not concomitantly with the echocardiography service routine, the researcher was able to calmly seek the best echocardiographic window in each patient, thus minimizing possible measurement biases.
This study used new echocardiography tools in the assessment of patients with MPS, a systemic disease with progressive cardiac involvement. These techniques have been shown to refine the cardiovascular follow-up of these patients, thus making it possible, together with the traditional and conventional techniques, to improve the diagnosis of cardiac sequelae and to anticipate possible interventions.
Conflicts of interestThe authors declare no conflicts of interest.
To Dr. Gabriela Nunes Leal, whose Master's degree dissertation inspired this study. Thank you for your constant support during the performance of this project.
Please cite this article as: Andrade MF, Guimarães IC, Acosta AX, Leão EK, Moreira MI, Mendes CM. Left ventricular assessment in patients with mucopolysaccharidosis using conventional echocardiography and myocardial deformation by two-dimensional speckle-tracking method. J Pediatr (Rio J). 2019;95:475–81.
This article is part of the Master's Degree dissertation of Dr. Mirela Frederico de Almeida Andrade through the Programa de Pós-Graduação em Processos Interativos dos Órgãos e Sistemas, Instituto de Ciências da Saúde, Universidade Federal da Bahia (UFBA), Salvador, BA, Brazil.