To associate intra-abdominal fat thickness measured by ultrasonography to the factors related to metabolic syndrome and to determine cutoff points of intra-abdominal fat measurement associated with a greater chance of metabolic syndrome in adolescents.
MethodsThis was a cross-sectional study, with 423 adolescents from public schools. Intra-abdominal fat was measured by ultrasonography. Anthropometric data were collected, and biochemical analyses were performed.
ResultsIntra-abdominal fat was measured by ultrasonography, showing a statistically significant association with the diagnosis of metabolic syndrome (p=0.037), body mass index (p<0.001), elevated triglyceride levels (p=0.012), decreased plasma HDL levels (p=0.034), and increased systemic blood pressure values (p=0.023). Cutoff values of intra-abdominal fat thickness measurements were calculated by ultrasound to estimate the individuals most likely to develop metabolic syndrome. In the logistic regression models, the cutoff values that showed the highest association with metabolic syndrome in males were 4.50, 5.35, 5.46, 6.24, and 6.50cm for the ages of 14, 15, 16, 17, and 18/19 years, respectively. In the female gender, the cutoff values defined for the same age groups were 4.46, 4.55, 4.45, 4.90, and 6.46cm. In an overall analysis using the ROC curve, without gender and age stratification, the cut-off of 3.67cm showed good sensitivity, but low specificity.
ConclusionUltrasonography is a useful method to estimate intra-abdominal adipose tissue in adolescents, which is associated with the main factors related to obesity and metabolic syndrome.
Relacionar a espessura da gordura intra-abdominal medida pela ultrassonografia aos fatores ligados à síndrome metabólica. Determinar pontos de corte da medida da gordura intra-abdominal associados a uma maior chance de síndrome metabólica em adolescentes.
MétodosEstudo seccional, com 423 adolescentes de escolas públicas. A gordura intra-abdominal foi medida pela ultrassonografia. Foram coletados dados antropométricos e feitas análises bioquímicas.
ResultadosAs medidas da gordura intra-abdominal por ultrassonografia apresentaram associação estatisticamente significativa com o diagnóstico de síndrome metabólica (p=0,037), índice de massa corporal (p<0,001), níveis elevados de triglicerídeos (p=0,012), redução dos níveis plasmáticos de HDL (p=0,034) e aumento da pressão arterial sistêmica (p=0,023). Calcularam-se pontos de corte da medida da espessura da gordura intra-abdominal por ultrassom, para estimar os indivíduos com mais chance para o desenvolvimento de síndrome metabólica. Em modelos de regressão logística, os pontos de corte que apresentaram maior associação com a síndrome metabólica no sexo masculino foram de 4,50, 5,35, 5,46, 6,24 e 6,50cm para as idades de 14, 15, 16, 17 e 18/19 anos, respectivamente. No sexo feminino, os pontos de corte definidos para as mesmas faixas etárias foram de 4,46, 4,55, 4,45, 4,90 e 6,46cm. Em análise global por meio da curva ROC, sem estratificações por sexo e idade, o ponto de corte de 3,67cm teve boa sensibilidade, porém apresentou baixa especificidade.
ConclusãoA ultrassonografia é um método útil para a estimativa do tecido adiposo intra-abdominal em adolescentes, está associada com os principais fatores relacionados à obesidade e à síndrome metabólica.
Metabolic syndrome (MS) was first described in 1988 and is understood as a group of metabolic disorders associated with central fat accumulation and insulin resistance, resulting in increased cardiovascular risk.1,2 Among adolescents, the prevalence of MS varies depending on the used criteria and characteristics of the assessed population.3 The set of diseases acquired during childhood/adolescence tends to persist into adult life.4
The diagnostic structuring of MS started in the 1980s and comprised several criteria, including the International Diabetes Federation (IDF) classification, proposed in 2005.5 That includes as criteria for MS the presence of glycemic, lipid, and blood pressure alterations, and considers central obesity, determined by the waist circumference (WC) measurement, the most important marker.6–8
Central obesity assessment through WC measurement is a simple and noninvasive test. However, its disadvantage is the intra- and inter-examiner variability, as well as the inability to differentiate intra-abdominal from the subcutaneous adipose tissue.9 New methods have been proposed for the measurement of the adipose component, such as skin fold measurement10 and imaging tests.
Imaging tests are appropriate tools for the differentiation and quantification of intra-abdominal fat (IAF) and subcutaneous fat (SCF). The accuracy in the characterization of these tissues provides support for the risk quantification of chronic diseases, feasible through ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI).11
Abdominal CT is considered the “gold standard” for abdominal fat quantification. MRI can also estimate intra-abdominal fat with good accuracy, but it is subject to greater variability and to a greater number of artifacts.12,13
Armellini et al. highlighted the good correlation between intra-abdominal adipose tissue measurements performed by ultrasonography and by computed tomography.14 Stolk et al.15 detected a strong correlation between measurements by ultrasonography, computed tomography, and ultrasonography with the WC measurement of intra-abdominal adipose tissue.
The presence of MS in the pediatric age group and in adolescents is associated with an increased risk of metabolic and cardiovascular disorders in adult life. Ultrasonography examinations constitute a useful tool for health professionals in the early diagnosis of MS. Even though it is a simple, non-invasive, and low-cost examination, as well as free from the risks of ionizing radiation, ultrasonography has been infrequently used for central obesity evaluation and, consequently, for MS. To the best of the authors’ knowledge, there are no cutoff points for intra-abdominal fat thickness measured by ultrasonography that can be used to predict MS in adolescents. Therefore, the aims of this study were to correlate the intra-abdominal fat thickness measured by ultrasonography with clinical and laboratory indicators used in the diagnosis of MS, as well as to indicate possible cutoff points that could identify individuals with a higher probability of having MS.
Patients and methodsThis was a cross-sectional study carried out between March and June of 2016, with adolescents aged 14–19 years, enrolled in state schools in the central region of the municipality of Divinópolis, state of Minas Gerais, Brazil. The study was carried out within a larger study, which aimed to estimate factors associated with excess weight in adolescents. The sample estimated for the base study (330 adolescents) considered the prevalence of excess weight in adolescents (27.47%) recorded in the Food and Nutrition Surveillance System of the municipality,16 in addition to a sampling error and a significance level of 5%. To define the sample of the present study, considering that the prevalence of MS in adolescents is approximately 7%,3 a lower absolute sampling error (1.5%) was chosen, which resulted in a sample of 1100 students. Of these, 563 refused to participate and 114 met the exclusion criteria, resulting in a population of 423 participants at the end of the investigation. To attain the representativeness of the student population of the central region of the municipality, each stratum was proportionally determined in relation to the number of students enrolled in each school.
The study was approved by the Research Ethics Committee of Universidade Federal de São João Del-Rei (No. 938.058). The participants’ parents or guardians were informed about the study. Students interested in participating in the study received the terms of assent and informed consent forms to be signed by their parents or guardians.
Laboratory tests, anthropometric measurements, and questionnairesLaboratory tests were collected at the school where the adolescents were enrolled, after a minimum of 12h of fasting, by a trained professional, at a previously scheduled date.
Levels of glycemia, high-density lipoprotein (HDL), and triglycerides were interpreted according to the parameters of the specific criteria for MS diagnosis,5 recommended by the IDF, which determine as alterations: for individuals aged 10–16 years old: levels of triglycerides>150mg/dL; HDL-cholesterol<40mg/dL; fasting blood glucose≥100mg/dL. For those older than 16 years, the criteria used to evaluate adults were used (levels of HDL-cholesterol≤35mg/dL for men and ≤40mg/dL for women, triglycerides>150mg/dL, and fasting blood glucose≥100mg/dL). The MS diagnosis is considered positive in the presence of central adiposity associated with the alteration of two or more parameters.5
Anthropometry and blood pressure measurements were performed following a pre-established examination routine, carried out in triplicate by the same examiner and using the mean value of the three measurements. Waist circumference was measured with an inelastic tape, using as reference the midpoint between the last costal arch and the iliac crest, on uncovered skin. The waist circumference data were evaluated according to those provided by in 2001 McCarthy et al.17 and indicated in a previous study.18
Weight was measured using a digital electronic scale (Tanita Corporation of America, Inc, Tanita® HD 313, IL, USA), whereas height was measured using an portable vertical stadiometer (Alturexata, Alturexata®, MG, Brazil).
Blood pressure was measured with an adequate cuff, using an automatic blood pressure device (Omron Healthcare, Omron® HEM711, Netherlands), after five minutes of resting, according to the technique recommended by the Brazilian Society of Cardiology.19 Blood pressure values higher than 130mmHg for systolic and 85mmHg for diastolic blood pressure were considered elevated.5
Ultrasonography examinationMeasurements of intra-abdominal fat thickness were obtained with portable ultrasonography equipment (Samsung, Samsung Medson® model PICO, South Korea) using a 3.5–5MHz convex transducer and the technique described by Stolk et al.15 The measurements were performed in triplicate, always by the same investigator, with prior technical standardization and statistical comparison by means of a pilot study conducted with two different investigators. For all images, the transducer was positioned on the midline, over a transversal straight line drawn from the midpoint between the last costal arch and the iliac crest.
Statistical analysesData were analyzed using the MedCalc program (MedCalc Software, version 18.2.1, Belgium). The Shapiro–Wilks normality test was applied to test for the normality of quantitative variables. The comparison of intra-abdominal fat values between the groups of sociodemographic variables was evaluated by the Mann–Whitney test. The ratio of abdominal fat to quantitative variables was analyzed using Spearman's correlation. Logistic regression models were constructed, adjusted for gender, age, ethnicity, and socioeconomic level, aiming to analyze the association between quantitative measures of abdominal fat in relation to MS and the presence of alterations in levels of triglycerides, blood glucose, blood pressure, HDL, and waist circumference and body mass index (BMI) measurements. Logistic regression models were used to analyze the association between the intra-abdominal fat cutoff points (80th, 85th, 90th, and 95th percentiles) and the occurrence of MS. In this case, the models were stratified by gender and into different age groups. The intra-abdominal fat percentiles were obtained by ordering the values in each age group (ages of 14, 15, 16, 17, or >18 years), separately for the male and female genders. The validity of the data obtained through the cutoff points in relation to the MS diagnosis was analyzed by calculating the sensitivity and specificity. A global ROC curve (not stratified by gender and age) of the intra-abdominal fat cutoff points was also constructed for MS prediction. The best cutoff point was the one with the highest arithmetic mean of sensitivity and specificity values. The regression models to the data was verified using the Hosmer and Lemeshow test. The level of statistical significance was set at 5% for all procedures.
Pilot studyA previous pilot study was developed in a smaller municipal school for the procedures of data collection, questionnaire application, anthropometric measurements, and blood pressure measurements. A total of 66 adolescents were evaluated within the age range of the study.
As for the ultrasonography assessment, measurements of intra-abdominal fat were performed in triplicate by two blinded radiologists, members of the Brazilian College of Radiology, who had more than ten years of experience. Intraobserver agreement was obtained for the first examiner, with a value of 0.941 (0.913, 0.962). The intraobserver agreement for the second examiner showed a value of 0.961 (0.943; 0.975). The interobserver agreement obtained a value of 0.976 (0.961; 0.985), showing high intra- and interobserver reproducibility in intra-abdominal fat measurements by ultrasonography.
ResultsA total of 423 students participated in this study, of which 284 (67.1%) were females. The mean age was 16.1 years (SD±1.11). Individuals who self-reported as black/mixed-race/native Brazilian accounted for 222 (56.1%) of the adolescents and 174 (43.9%) self-reported as white. The prevalence of MS was 1.9%.
As for the intra-abdominal fat thickness evaluated by ultrasonography assessment, the median was 3.3cm (25th percentile=2.8 and 75th percentile=3.9), being 4.03cm in the male individuals and 3.10cm in females. The intra-abdominal adipose tissue thickness was significantly higher in males when compared to females (4.06 vs. 3.1, p<0.001) and in the non-white population (3.51 vs. 3.1, p<0.001).
The intra-abdominal fat measurement by ultrasonography showed a positive and statistically significant correlation with diastolic blood pressure (p=0.023), levels of triglycerides (p=0.012), BMI (p<0.001), and waist circumference (p<0.001). There was an inverse association between intra-abdominal fat and HDL levels (p=0.034).
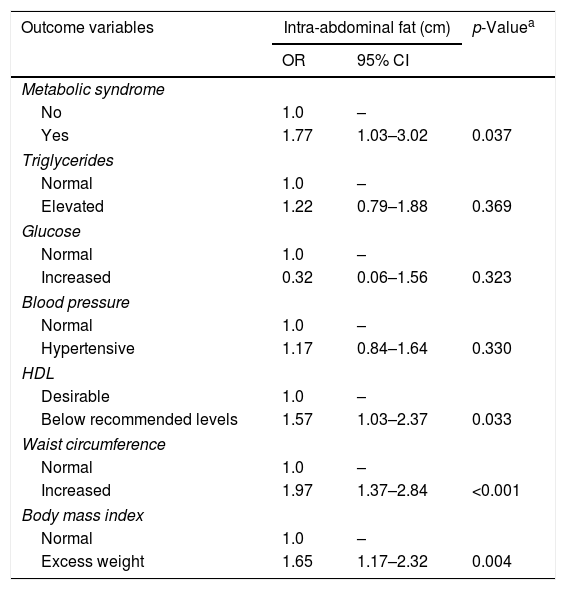
In the logistic regression models, it was verified that the intra-abdominal fat measurement was associated with MS diagnosis (p=0.037), and with changes in HDL levels (p=0.033), waist circumference (p<0.001), and BMI measurements (p=0.004). Table 1 shows the odds ratios and the respective confidence intervals of all analyzed variables.
Logistic regression model for predicting metabolic syndrome and its components based on intra-abdominal fat (cm).
| Outcome variables | Intra-abdominal fat (cm) | p-Valuea | |
|---|---|---|---|
| OR | 95% CI | ||
| Metabolic syndrome | |||
| No | 1.0 | – | |
| Yes | 1.77 | 1.03–3.02 | 0.037 |
| Triglycerides | |||
| Normal | 1.0 | – | |
| Elevated | 1.22 | 0.79–1.88 | 0.369 |
| Glucose | |||
| Normal | 1.0 | – | |
| Increased | 0.32 | 0.06–1.56 | 0.323 |
| Blood pressure | |||
| Normal | 1.0 | – | |
| Hypertensive | 1.17 | 0.84–1.64 | 0.330 |
| HDL | |||
| Desirable | 1.0 | – | |
| Below recommended levels | 1.57 | 1.03–2.37 | 0.033 |
| Waist circumference | |||
| Normal | 1.0 | – | |
| Increased | 1.97 | 1.37–2.84 | <0.001 |
| Body mass index | |||
| Normal | 1.0 | – | |
| Excess weight | 1.65 | 1.17–2.32 | 0.004 |
OR, odds ratio; CI, confidence interval; HDL, high-density lipoprotein.
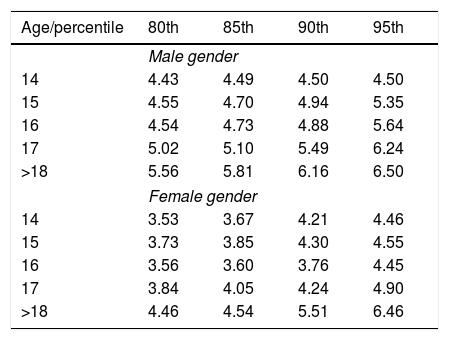
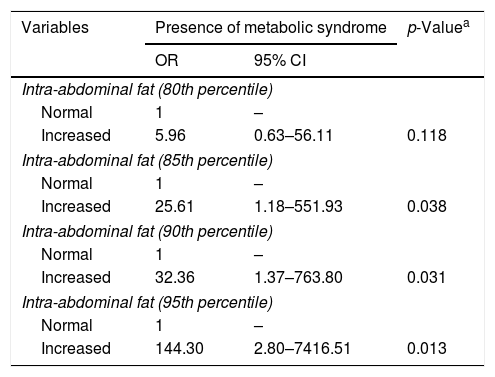
A positive correlation was found between intra-abdominal fat and the adolescents’ age (r=0.167, p<0.001). The cutoff points were constructed using the intra-abdominal fat percentiles (Table 2). Those established in the 85th, 90th, and 95th percentiles showed a statistically significant association with MS, and it was possible to observe a gradual increase in the odds ratio for each percentile increase. The best predictor of MS was the 95th percentile (Table 3).
80th, 85th, 90th, and 95th percentiles of intra-abdominal fat measures (cm) by gender and age of the adolescents.
| Age/percentile | 80th | 85th | 90th | 95th |
|---|---|---|---|---|
| Male gender | ||||
| 14 | 4.43 | 4.49 | 4.50 | 4.50 |
| 15 | 4.55 | 4.70 | 4.94 | 5.35 |
| 16 | 4.54 | 4.73 | 4.88 | 5.64 |
| 17 | 5.02 | 5.10 | 5.49 | 6.24 |
| >18 | 5.56 | 5.81 | 6.16 | 6.50 |
| Female gender | ||||
| 14 | 3.53 | 3.67 | 4.21 | 4.46 |
| 15 | 3.73 | 3.85 | 4.30 | 4.55 |
| 16 | 3.56 | 3.60 | 3.76 | 4.45 |
| 17 | 3.84 | 4.05 | 4.24 | 4.90 |
| >18 | 4.46 | 4.54 | 5.51 | 6.46 |
Logistic regression models for predicting metabolic syndrome (IDF) based on intra-abdominal fat increase according to cutoff points of different percentiles.
| Variables | Presence of metabolic syndrome | p-Valuea | |
|---|---|---|---|
| OR | 95% CI | ||
| Intra-abdominal fat (80th percentile) | |||
| Normal | 1 | – | |
| Increased | 5.96 | 0.63–56.11 | 0.118 |
| Intra-abdominal fat (85th percentile) | |||
| Normal | 1 | – | |
| Increased | 25.61 | 1.18–551.93 | 0.038 |
| Intra-abdominal fat (90th percentile) | |||
| Normal | 1 | – | |
| Increased | 32.36 | 1.37–763.80 | 0.031 |
| Intra-abdominal fat (95th percentile) | |||
| Normal | 1 | – | |
| Increased | 144.30 | 2.80–7416.51 | 0.013 |
OR, odds ratio; CI, confidence interval; IDF, International Diabetes Federation.
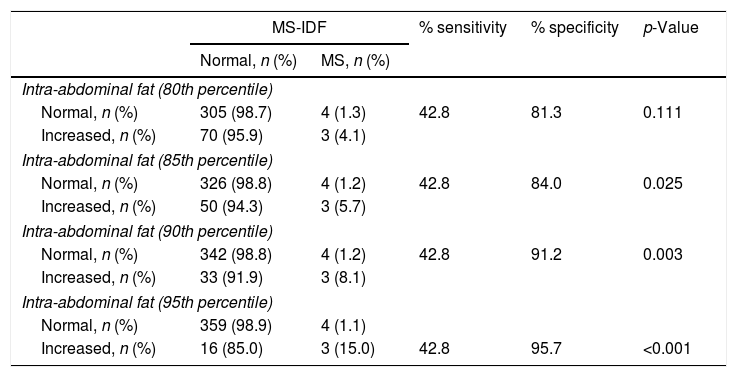
Table 4 shows the validity analysis of the information obtained through intra-abdominal fat categorized according to percentile cutoff points for the diagnosis of MS. In all cases, the calculated sensitivity remained the same (42.8%), but the 95th percentile showed better specificity (95.7%). The ROC curve, constructed with data on the intra-abdominal fat of all participants, showed a significant ability in predicting MS (p=0.034), with an area under the curve of 0.73. The best cutoff point was 3.67cm, with sensitivity of 85.7% and specificity of 68.3%. The cutoff point of 3.93cm was considered the second best and showed a good association between sensitivity (71.4%) and specificity (75.5%). The cutoff point of 4.47cm showed the same sensitivity obtained with the percentile method (42.8%) but had lower specificity (86.17%). The other cutoff points above this one, which showed superior specificities, had low sensitivity values (<0.15).
Analysis of agreement between intra-abdominal fat categorized according to different percentile cutoff points and the diagnosis of metabolic syndrome (IDF).
| MS-IDF | % sensitivity | % specificity | p-Value | ||
|---|---|---|---|---|---|
| Normal, n (%) | MS, n (%) | ||||
| Intra-abdominal fat (80th percentile) | |||||
| Normal, n (%) | 305 (98.7) | 4 (1.3) | 42.8 | 81.3 | 0.111 |
| Increased, n (%) | 70 (95.9) | 3 (4.1) | |||
| Intra-abdominal fat (85th percentile) | |||||
| Normal, n (%) | 326 (98.8) | 4 (1.2) | 42.8 | 84.0 | 0.025 |
| Increased, n (%) | 50 (94.3) | 3 (5.7) | |||
| Intra-abdominal fat (90th percentile) | |||||
| Normal, n (%) | 342 (98.8) | 4 (1.2) | 42.8 | 91.2 | 0.003 |
| Increased, n (%) | 33 (91.9) | 3 (8.1) | |||
| Intra-abdominal fat (95th percentile) | |||||
| Normal, n (%) | 359 (98.9) | 4 (1.1) | |||
| Increased, n (%) | 16 (85.0) | 3 (15.0) | 42.8 | 95.7 | <0.001 |
MS, metabolic syndrome; IDF, International Diabetes Federation.
The present study demonstrated an association between intra-abdominal fat thickness measured by ultrasonography and factors related to MS, and identified cutoff points for the intra-abdominal fat measurement associated with a higher chance of MS in adolescents.
In Brazil, the prevalence of MS varies among different studies and depends on the diagnostic criteria used.3,20,21 In the present study, the prevalence of MS was lower than that observed in previous studies.3 The non-agreement between the diagnostic criteria of MS, in turn, emphasizes the need to use standardized methods for MS detection.
One advantage of using ultrasonography for central obesity assessment, as well as other imaging tests, is the possibility of differentiating which adipose tissue reservoir results in an increase of abdominal volume. The commonly used method to assess central obesity, the measurement of abdominal circumference, invariably measures the sum of all compartments of adipose tissue deposition in the abdomen, which is undesirable, since they have different roles in the metabolism and pathophysiology of MS. Authors22 have demonstrated that BMI and waist circumference may not accurately represent intra-abdominal fat.
Considering the current health scenario, with an increasing number of individuals with excess weight and the benefits of imaging tests, the present study evaluated the intra-abdominal fat measurement using ultrasonography. The method demonstrated to be quite reproducible for central obesity evaluation in adolescents, showing high intra- and interobserver correlation coefficients, as previously verified by Diniz et al.23 and Mauad et al.24 The accuracy of the agreement measures obtained in the present study is closely related to the use of standardized techniques.15
Leite et al.25 showed the ability of IAF measurements to predict cardiovascular risk factors, such as blood pressure, lipids, and glycemic levels. In the present study, a significant association of intra-abdominal fat with levels of diastolic blood pressure, HDL, triglycerides, waist circumference, and BMI measurements was demonstrated. Considering the ability of intra-abdominal fat measurement to predict not only the diagnosis of MS and cardiovascular risk but also its association with the isolated factors that comprise MS, its use in clinical practice is justified, as well as its possible inclusion in imaging examination protocols.
The increase in intra-abdominal adipose tissue with increasing age was discussed by Maurovich-Horvat et al.,26 who determined that the subcutaneous/intra-abdominal fat (SCF/IAF) ratio decreases through the age groups, indicating a more significant participation of intra-abdominal adiposity in MS. These authors found this association to be lower in males, noting that men have relatively higher amounts of intra-abdominal fat. The present study corroborates such information, indicating an increase in abdominal fat and, consequently, of cutoff points found with increasing age in both genders.
The controversial influence of subcutaneous fat on the establishment of MS in children seems to lose importance in adulthood, a period in which intra-abdominal fat is more significant. Adolescence, as a moment when important body changes occur, could then be considered as a transition point regarding the influence of these different adipose tissue reservoirs.25–29
The present study indicated intra-abdominal fat cutoff points that were possibly associated with MS in different age groups. Leite et al.,25 when evaluating adults, found the value of 8cm of intra-abdominal fat thickness as the cutoff point for predicting cardiovascular risk in women and 9cm in men. Eifler,30 also evaluating adults, found the thickness of 9cm in women and 10cm in men as the cutoff points for intra-abdominal fat thickness associated with a greater chance of developing hepatic steatosis. No studies were found in the literature that evaluated intra-abdominal fat cutoff points in adolescents.
In the present study, when determining a cutoff value associated with MS in adolescents, the 80th, 85th, 90th, and 95th percentiles of intra-abdominal fat stratified by gender and age were calculated. The 95th percentile showed the highest strength of association with the occurrence of MS and a higher specificity value.
According to the cutoff points showed in this study, the chance of developing MS increases significantly when the individual is at the 95th percentile of different ages. The high specificity value of this percentile is a favorable argument for its use, even with moderate sensitivity. In the analysis of the ROC curve, the cutoff point of 3.67cm showed good sensitivity, but low specificity. Thus, its use could cause a relevant negative effect on clinical practice, considering the high number of false positive cases. The 3.93cm cutoff, which showed a sensitivity of 71.4% and a specificity of approximately 75.5%, although less intensely, would also result in a high number of false positive cases.
It is important to emphasize that the present study may have been limited due to the quantitative sample assessed. There were a significant number of refusals, which reduced the accuracy of the obtained estimates and prevented the construction of stratified ROC curves. As a positive factor, a classification of AF based on percentiles stratified by gender and age was used, which allowed specific cutoff points to be obtained for these groups and attained a high specificity. Additionally, it was observed that refusals were not influenced by factors such as gender, age, class, and school of the adolescents.
The easy performance of intra-abdominal fat measurement through ultrasonography favors its inclusion in routine abdominal examinations, as well as its association with biochemical parameters of MS and the possibility of early detection. The cutoff points indicated in the present study, when analyzed considering the local epidemiological contexts and together with data from other physical and laboratory tests, may be useful tools for decision-making in clinical practice. It should be emphasized that new studies in different socio-demographic situations that seek to confirm or improve the identified cutoff points should be mandatory in future investigations.
FundingFundação de Amparo à Pesquisa de Minas Gerais (FAPEMIG).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Novais RL, Café AC, Morais AA, Bila WC, Santos GD, Lopes CA, et al. Intra-abdominal fat measurement by ultrasonography: association with anthropometry and metabolic syndrome in adolescents. J Pediatr (Rio J). 2019;95:342–9.
Study carried out at Universidade Federal de São João Del-Rei, São João Del-Rei, MG, Brazil.