To evaluate the association of intimate partner violence during the gestational period and the development of externalizing and internalizing behavioral problems in children and adolescents.
Source of dataA meta-analysis of cohort and case–control studies was performed, using studies selected from electronic databases. Eligible studies included women who experienced intimate partner violence during pregnancy and their children's behavioral problems. These problems encompass two groups: externalizing problems (expressed by hyperactivity, aggressive and challenging behavior, and delinquency) and internalizing problems (represented by depressive moods, anxiety, and somatic symptoms). The risk of bias was assessed by the Newcastle-Ottawa Quality Assessment Scale (NOS) and the quality of evidence by the Grading of Recommendations, Assessment, Development and Evaluation (GRADE). RevMan 5.3 software was used for the meta-analysis.
Data synthesisOf the 687 eligible articles, only seven met all inclusion criteria and consisted of 12,250 mother/child pairs. The age range of the assessed children varied from 10 months to 16 years. The odds of internalizing problems in children exposed to prenatal violence were two-fold higher (OR=2.10, 95% CI: 1.17–3.76) and that of externalizing problems were 1.9-fold higher (95% CI: 1.28–2.83), when compared to children of unexposed mothers.
ConclusionThe results of this study are consistent with the hypothesis that women's exposure to intimate partner violence during pregnancy may be associated with behavioral problems of their children, emphasizing the need for greater understanding about the vulnerability of children to adversity in early ages.
Avaliar a associação da violência por parceiro íntimo durante o período gestacional e o desenvolvimento de problemas comportamentais externalizantes e internalizantes de crianças e adolescentes.
Fontes dos dadosFoi realizada metanálise de estudos de coorte e caso-controle, selecionados em bases de dados eletrônicas. Os estudos elegíveis incluíram: mulheres que sofreram violência pelo parceiro íntimo durante a gravidez e problemas comportamentais de seus filhos. Esses problemas englobam dois grupos: os problemas externalizantes (que se expressam por hiperatividade, comportamento agressivo e desafiante e delinquência) e os internalizantes (representados por humor depressivo, ansiedade e sintomas somáticos). O risco de viés foi avaliado pela Newcastle - Ottawa Quality Assessment Scale (NOS) e a qualidade da evidência pelo “Grading of Recommendations, Assessment, Development and Evaluation” (GRADE). O software RevMan 5.3 foi usado para a metanálise.
Síntese dos dadosDos 687 artigos elegíveis, apenas sete apresentaram todos os critérios de inclusão e formaram 12.250 pares de mães e filhos. A faixa etária das crianças analisadas variou de 10 meses a 16 anos. A chance de problemas internalizantes das crianças, expostas à violência pré-natal, foi duas vezes maior (OR = 2,10; IC 95%: 1,17-3,76) e de problemas externalizantes, foi 1,90 vezes maior (IC 95%: 1,28-2,83), quando comparada com filhos de mães não expostas.
ConclusãoOs resultados deste estudo são consistentes com a hipótese que a exposição da mulher a violência por parceiro íntimo na gestação pode estar associada a problemas comportamentais dos filhos, destacando a necessidade de maior compreensão sobre vulnerabilidade das crianças a adversidades precoces.
Intimate partner violence (IPV) during pregnancy is a global issue with high prevalence rates among low-income women of reproductive age,1,2 with serious consequences for health of women, the fetus, and the child.3,4 The consequences for women, in addition to physical injuries5 and homicide,6 includes psychiatric morbidity, with a higher risk of common mental disorders,7 post-traumatic stress disorder,8 and postpartum depression.8 Regarding the children, most of the studies show the physical consequences, including low birth weight, prematurity, miscarriage, and neonatal and perinatal mortality.1 Reviews published to date on IPV exposure during pregnancy4,9 have shown physical consequences, but have not reported the association with behavioral problems of children and adolescents.
While there is a growing body of research on children's exposure to IPV suffered by their mothers,10–12 little is known about the long-term consequences of prenatal exposure to violence regarding the child's mental development.
Studies have been conducted to understand how IPV, a proven stressful event during pregnancy, hinders the development of children's emotional and behavioral regulation systems.13 Prenatal stress has been shown to be mediated by maternal and fetal cortisol levels, which alter the programming of fetal neurons,14 and may play an important role in the child's social and emotional development.15,16 There is evidence that exposure to IPV may predispose to externalizing problems that include antisocial behavior, conduct and impulse control disorders, which can be expressed by hyperactivity, aggressive and defiant behavior, and delinquency.17–20 The internalizing symptomatology is represented by depression, anxiety, introspection, and somatic symptoms.17–19
The objective of this review was to assess whether IPV during pregnancy is associated to the development of behavioral problems of children and adolescents in the long term.
MethodsThe description of this review followed the parameters of the Meta-analysis of Observational Studies in Epidemiology (MOOSE)21 and the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA),22 recommended by the international literature for the reporting systematic reviews of observational studies. The previously established protocol was registered in an international database of systematic review protocols: International Prospective Register of Systematic Reviews (PROSPERO) under No: CRD42015026382, accessible by the link: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=26382.
Eligibility criteriaThe studies were eligible if they met the criteria: (a) type of study: cohort or case–control studies; (b) population: pregnant women in any trimester of pregnancy, regardless of age group (c) exposure: clear definition (given by the authors) of physical, sexual, or psychological violence perpetrated by the intimate partner during pregnancy; (d) outcome: behavioral, externalizing, and/or internalizing problems in children and adolescents, evaluated with validated tools. Studies that assessed violence against women perpetrated by men other than their intimate partners, and studies that assessed the child's direct exposure to violence were excluded.
Sources of informationThe search strategy included references, until June 2017, from the following electronic databases: MEDLINE/PubMed (1966–2017), LILACS (1982–2017), CINAHL (1981–2017), Web of Science (1945–2017), Scopus (1950–2017), and PsycINFO (1887–2017). The Medical Subject Headings (MeSH) terms and entries were used for MEDLINE/PubMed, Web of Science and Scopus; the Descriptors in Health Sciences (DeCS) for LILACS; the CINAHL titles for CINAHL and the Thesaurus of Psychological Index Terms for PsycINFO. The search included the terms: “domestic violence” OR “family violence” OR “spouse violence” OR “spouse abuse” OR “partner violence” OR “intimate partner violence” OR “intimate partner abuse” OR “violence against women” OR “partner abuse” OR “verbal abuse” OR “psychological abuse” OR “physical abuse” OR “sexual abuse” OR “antenatal domestic violence” AND “prenatal” OR “antenatal” OR “pregnant women” OR “pregnancy” OR “pregnant” AND “child* behavior disorders” OR “child* behavior problems” OR “child behavior” OR “child development” OR “child development disorders” OR “maltreatment” OR “behavior disorders” OR “behavior problems” OR “conduct disorder”. A specific search strategy was used for each database.
Study selection and data extractionIn the first phase, the study selection was carried out by two researchers (E.P.S. and C.H.S.A.), who independently evaluated the titles and abstracts of the articles retrieved by the search strategy, with no language or date restriction. At this phase, articles inclusion was carried out according to the established eligibility criteria. Articles that raised questions and were potentially eligible were retained for subsequent full-text review. At the second phase, the full-text articles were evaluated. The reference lists of the included articles were also evaluated to verify whether any potentially eligible article was not present in the initial search carried out in the databases. Articles were excluded when they did not meet the eligibility criteria. At the third phase, the data were extracted according to a previously established form. Disagreements were resolved by consensus and by consultation and supervision of a third researcher (A.B.L.).
Risk of bias assessment of articlesThe risk of bias of the included studies was independently analyzed by two reviewers (E.P.S. and C.H.S.A.) using the Newcastle-Ottawa Quality Assessment Scale (NOS), which evaluates the design and quality of cohort and case–control studies.23 This scale facilitates the incorporation of quality assessments in the interpretation of meta-analysis results and is not used as an inclusion or exclusion criterion for articles. It consists of eight items, divided into three dimensions: selection, comparability, and outcome (for cohort studies) or exposure (for case–control studies). Each article is assigned a number of stars: (a) selection (maximum: four stars); (b) comparability (maximum: two stars); and (c) results (maximum: three stars). Therefore, during the processing of the article quality analysis, high-quality studies can achieve a maximum of nine stars. However, the final evaluation should not be made by counting the number of stars but qualitatively, by the individual component of each item.
The definition of externalizing and internalizing problems17 and the evaluation of children and adolescents by validated scales were considered to score the outcome items (in the cohort studies) and exposure (for case–control studies).
As some characteristics of the mothers (mental health, alcohol, and drug use) are considered risk factors for the children's mental health,24,25 these factors must be assessed through structured interviews or reliable reports for the exposure analysis item. Studies that controlled for one or more of these risk factors received one or two stars in the comparability item.
Quality of evidence assessment of the articlesThe evaluation of the quality of evidence of the studies was carried out by two reviewers (E.P.S. and C.H.S.A.), using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) method. The classification of evidence is described in four levels, which represent the reliability in the estimation of the observed effects: high (confidence that the true effect is close to the estimated is strong), moderate (confidence in the estimated effect is moderate), low (confidence in the effect is limited), and very low (confidence in the estimated effect is very limited, and there is a significant degree of uncertainty in the findings).26
The initial classification of the quality of evidence is defined based on the study design. The criteria are defined, and the assessment of these aspects allows reducing or increasing the level of evidence. The factors responsible for the reduction in the level of evidence are: risk of bias, inconsistency, indirect evidence, inaccuracy, and publication bias. If the level is not lowered, the evidence from observational studies can have the confidence in the estimated effect increased, considering three factors: high magnitude of effect, dose-response gradient, and confounding factors.27
Data analysisData analysis was performed using RevMan software (Review Manager [Computer program]. Version 5.3. Copenhagen, Denmark: The Nordic Cochrane Centre). Study homogeneity was evaluated through the heterogeneity test, being considered homogeneous when a p-value>0.05 was found. The heterogeneity index (I2) was classified as low heterogeneity with values up to 30% and as moderate, with values ranging from 30 to 60%. The magnitude of the effect was calculated by the odds ratio (OR), with its 95% confidence interval. Due to the heterogeneity of the study populations and the time of outcome evaluation, a random effect meta-analysis was performed. For a study that showed the number zero for events in the control group, a fixed-effect analysis was performed using the Peto's method. A subgroup analysis by age groups (<1 to 4 years and 5 to 16 years) was performed.
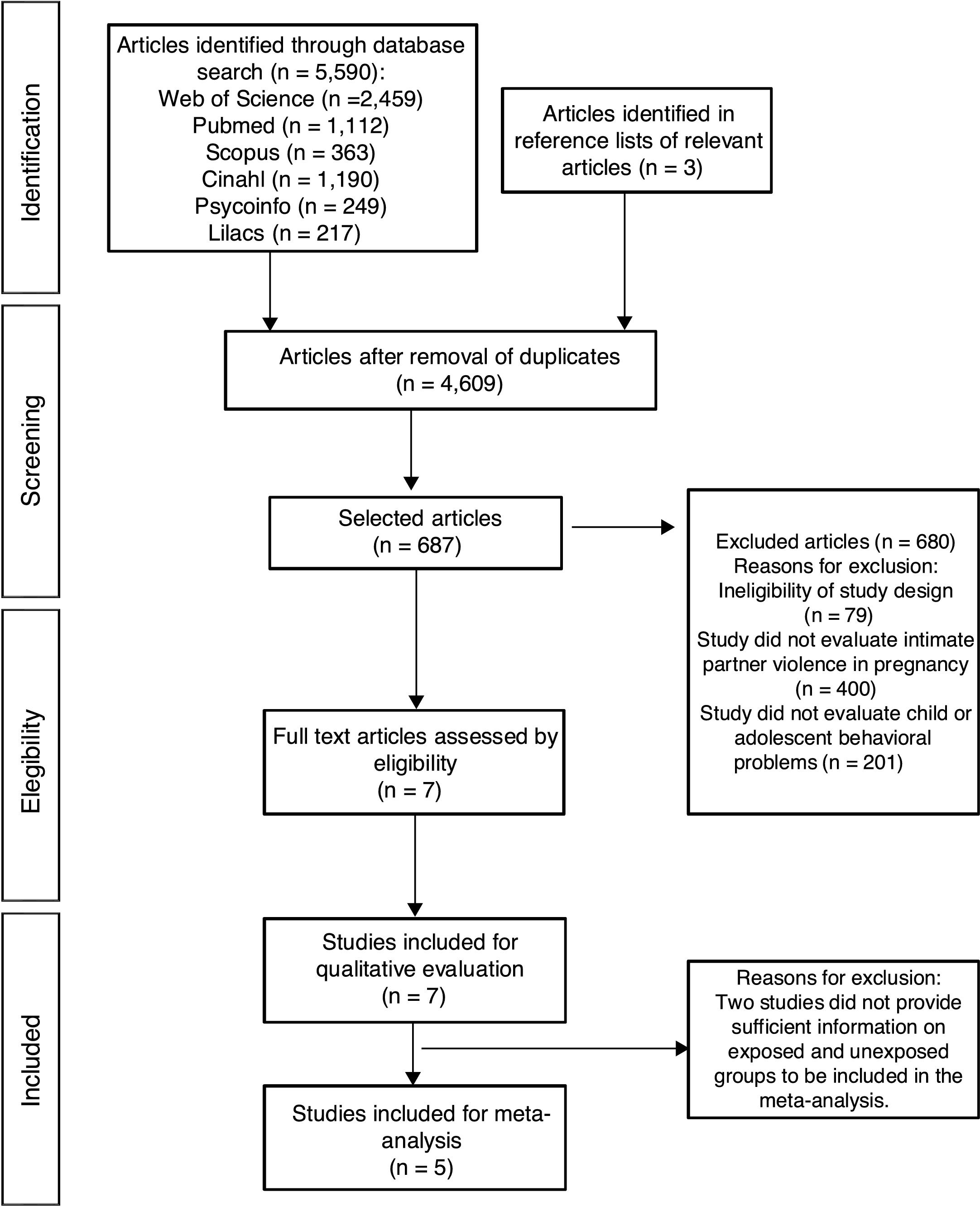
ResultsStudy selectionThe database search retrieved a total of 5593 studies, of which 687 were selected for a more detailed evaluation. After the study selection and application of the eligibility criteria, seven studies3,5,16,20,28–30 were included (Fig. 1).
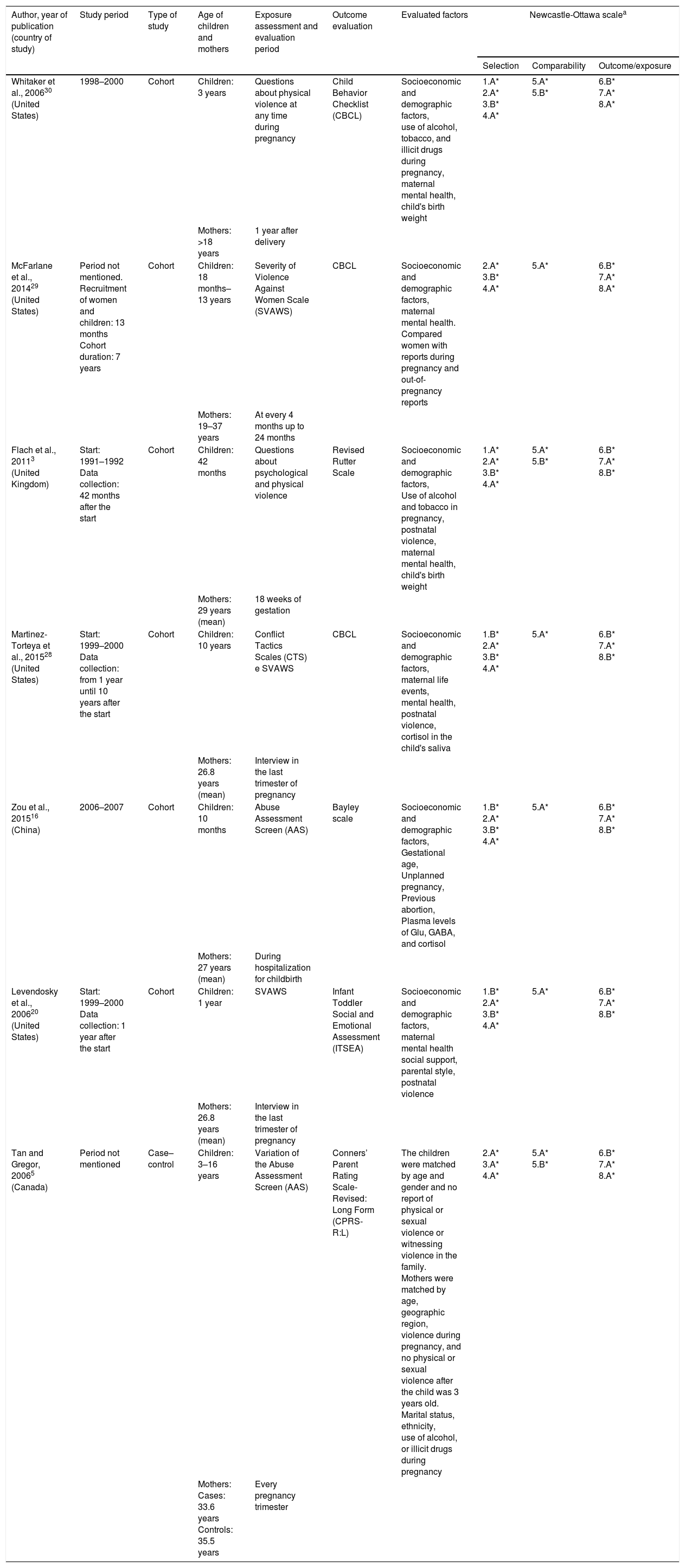
Study characteristicsTable 1 shows the characteristics of the included studies, published in four countries between 2006 and 2015, of which four20,28–30 were carried out in the United States. There was a predominance of cohort studies and only one study5 had a case–control design. Two studies described population-based samples3,30 and the other five studies included samples from shelters and legal services,29 health services,16 and several community services.5,20,28
Characteristics of studies on exposure to intimate partner violence in pregnancy and behavioral problems of children, 2006–2015.
| Author, year of publication (country of study) | Study period | Type of study | Age of children and mothers | Exposure assessment and evaluation period | Outcome evaluation | Evaluated factors | Newcastle-Ottawa scalea | ||
|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome/exposure | |||||||
| Whitaker et al., 200630 (United States) | 1998–2000 | Cohort | Children: 3 years | Questions about physical violence at any time during pregnancy | Child Behavior Checklist (CBCL) | Socioeconomic and demographic factors, use of alcohol, tobacco, and illicit drugs during pregnancy, maternal mental health, child's birth weight | 1.A* 2.A* 3.B* 4.A* | 5.A* 5.B* | 6.B* 7.A* 8.A* |
| Mothers: >18 years | 1 year after delivery | ||||||||
| McFarlane et al., 201429 (United States) | Period not mentioned. Recruitment of women and children: 13 months Cohort duration: 7 years | Cohort | Children: 18 months–13 years | Severity of Violence Against Women Scale (SVAWS) | CBCL | Socioeconomic and demographic factors, maternal mental health. Compared women with reports during pregnancy and out-of-pregnancy reports | 2.A* 3.B* 4.A* | 5.A* | 6.B* 7.A* 8.A* |
| Mothers: 19–37 years | At every 4 months up to 24 months | ||||||||
| Flach et al., 20113 (United Kingdom) | Start: 1991–1992 Data collection: 42 months after the start | Cohort | Children: 42 months | Questions about psychological and physical violence | Revised Rutter Scale | Socioeconomic and demographic factors, Use of alcohol and tobacco in pregnancy, postnatal violence, maternal mental health, child's birth weight | 1.A* 2.A* 3.B* 4.A* | 5.A* 5.B* | 6.B* 7.A* 8.B* |
| Mothers: 29 years (mean) | 18 weeks of gestation | ||||||||
| Martinez-Torteya et al., 201528 (United States) | Start: 1999–2000 Data collection: from 1 year until 10 years after the start | Cohort | Children: 10 years | Conflict Tactics Scales (CTS) e SVAWS | CBCL | Socioeconomic and demographic factors, maternal life events, mental health, postnatal violence, cortisol in the child's saliva | 1.B* 2.A* 3.B* 4.A* | 5.A* | 6.B* 7.A* 8.B* |
| Mothers: 26.8 years (mean) | Interview in the last trimester of pregnancy | ||||||||
| Zou et al., 201516 (China) | 2006–2007 | Cohort | Children: 10 months | Abuse Assessment Screen (AAS) | Bayley scale | Socioeconomic and demographic factors, Gestational age, Unplanned pregnancy, Previous abortion, Plasma levels of Glu, GABA, and cortisol | 1.B* 2.A* 3.B* 4.A* | 5.A* | 6.B* 7.A* 8.B* |
| Mothers: 27 years (mean) | During hospitalization for childbirth | ||||||||
| Levendosky et al., 200620 (United States) | Start: 1999–2000 Data collection: 1 year after the start | Cohort | Children: 1 year | SVAWS | Infant Toddler Social and Emotional Assessment (ITSEA) | Socioeconomic and demographic factors, maternal mental health social support, parental style, postnatal violence | 1.B* 2.A* 3.B* 4.A* | 5.A* | 6.B* 7.A* 8.B* |
| Mothers: 26.8 years (mean) | Interview in the last trimester of pregnancy | ||||||||
| Tan and Gregor, 20065 (Canada) | Period not mentioned | Case–control | Children: 3–16 years | Variation of the Abuse Assessment Screen (AAS) | Conners’ Parent Rating Scale-Revised: Long Form (CPRS-R:L) | The children were matched by age and gender and no report of physical or sexual violence or witnessing violence in the family. Mothers were matched by age, geographic region, violence during pregnancy, and no physical or sexual violence after the child was 3 years old. Marital status, ethnicity, use of alcohol, or illicit drugs during pregnancy | 2.A* 3.A* 4.A* | 5.A* 5.B* | 6.B* 7.A* 8.A* |
| Mothers: Cases: 33.6 years Controls: 35.5 years | Every pregnancy trimester | ||||||||
Glu, glutamine; GABA, Gamma aminobutyric acid.
Newcastle-Ottawa scale (the score is calculated by the number of *).
Case–control studies: Selection: 1. Is the case definition adequate? 2. Case representativeness; 3. Control selection; 4. Control definition. Comparability: 5. Comparability of cases and controls based on study design or analysis. Exposure: 6. Exposure assessment; 7. Same evaluation method for cases and controls; 8. Non-response rate.
Cohort studies: Selection: 1. Representativeness of the exposed cohort; 2. Selection of the unexposed cohort; 3. Exposure determination; 4. Demonstration that the outcome of interest was not present at the start of the study. Comparability: 5. Comparability of cohorts based on study design or analysis. Outcome: 6. Outcome evaluation; 7. The follow-up was long enough for the results to occur; 8. Adequacy of cohort follow-up.
The studies included children and adolescents aged 10 months to 16 years, whereas maternal age ranged from 18 to 37 years. Male children were more frequent in five studies.3,5,16,20,28 The salivary and plasma cortisol levels of children were evaluated in two studies.16,28
The summary of the risk of bias analysis for the cohort studies3,16,20,29,30 and the case–control study5 included in this review, is described in Table 1.
Exposure was evaluated by standardized tools in five studies5,16,20,28,29 and the other two3,30 used their own questionnaires. Three studies16,20,29 assessed the three types of violence (psychological, physical, and sexual), and physical violence was evaluated by all of them. Studies that did not use a standardized tool to assess exposure3,30 contributed with the highest percentages in the meta-analysis to behavioral3 (44.7%), externalizing30 (60.8%), and internalizing30 problems (57.6%), due to the large sample size, in addition to the small percentage of losses.
The evaluation interval during pregnancy varied among the studies. Four studies3,16,20,28 carried out only one evaluation, one study5 evaluated every trimester, and another study29 assessed every four months. Only one study carried out an interview one year after delivery.30 Therefore, the establishment of exposure, i.e., IPV during pregnancy, was considered adequate.
The outcome (behavioral problems) was assessed using standardized tools in all studies. Four studies evaluated internalizing and externalizing problems,5,28–30 one study evaluated only externalizing problems20 and two studies3,16 assessed the total of the problems. The follow-up of the cohort studies3,16,20,29,30 indicates that the time was sufficient for the outcome to occur.
The number of losses at follow-up was higher than 10% in five studies3,5,20,28,30; in three of them,3,20,28 the data input technique was used to minimize loss bias.
All studies selected exposed and unexposed individuals from the same sample. The assessment of confounding factors varied among the studies and included socioeconomic and demographic factors and mental health,3,20,28–30 use of alcohol, tobacco and illicit drugs during pregnancy,3,5,30 postnatal violence,3,5,20,28,29 social support and parental style,20 unplanned pregnancy,16 stressful life events,3 child's gender and gestational age,3,16 and birth weight.16,30
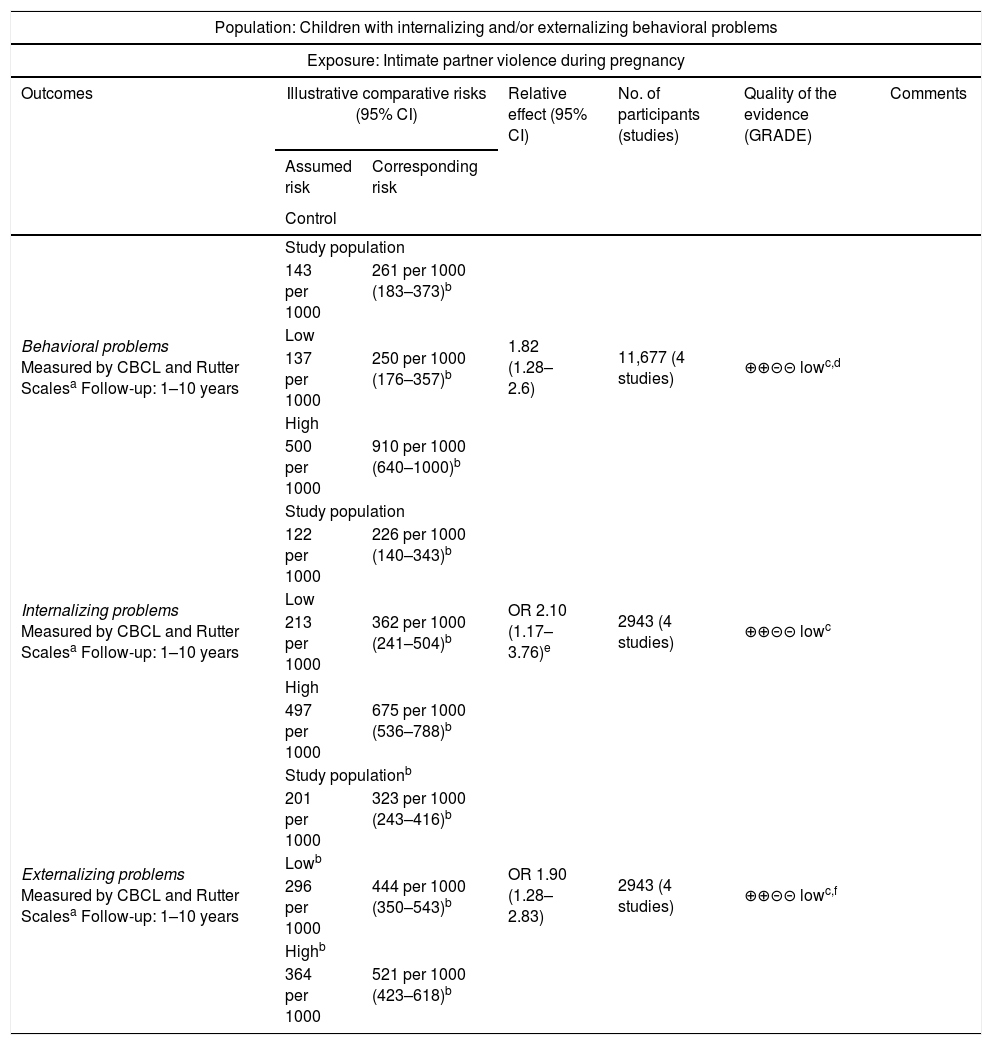
The quality of evidence of the outcomes (behavioral, externalizing and/or internalizing problems) evaluated by GRADE was classified as low (Table 2).
Grading of the Recommendations, Assessment, Development and Evaluation Evidence Profile (GRADE) for violence during pregnancy as a risk factor for behavioral problems in children, 2006–2016.
| Population: Children with internalizing and/or externalizing behavioral problems | ||||||
|---|---|---|---|---|---|---|
| Exposure: Intimate partner violence during pregnancy | ||||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | ||||||
| Behavioral problems Measured by CBCL and Rutter Scalesa Follow-up: 1–10 years | Study population | 1.82 (1.28–2.6) | 11,677 (4 studies) | ⊕⊕⊝⊝ lowc,d | ||
| 143 per 1000 | 261 per 1000 (183–373)b | |||||
| Low | ||||||
| 137 per 1000 | 250 per 1000 (176–357)b | |||||
| High | ||||||
| 500 per 1000 | 910 per 1000 (640–1000)b | |||||
| Internalizing problems Measured by CBCL and Rutter Scalesa Follow-up: 1–10 years | Study population | OR 2.10 (1.17–3.76)e | 2943 (4 studies) | ⊕⊕⊝⊝ lowc | ||
| 122 per 1000 | 226 per 1000 (140–343)b | |||||
| Low | ||||||
| 213 per 1000 | 362 per 1000 (241–504)b | |||||
| High | ||||||
| 497 per 1000 | 675 per 1000 (536–788)b | |||||
| Externalizing problems Measured by CBCL and Rutter Scalesa Follow-up: 1–10 years | Study populationb | OR 1.90 (1.28–2.83) | 2943 (4 studies) | ⊕⊕⊝⊝ lowc,f | ||
| 201 per 1000 | 323 per 1000 (243–416)b | |||||
| Lowb | ||||||
| 296 per 1000 | 444 per 1000 (350–543)b | |||||
| Highb | ||||||
| 364 per 1000 | 521 per 1000 (423–618)b | |||||
The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI, confidence interval; OR, odds ratio.
GRADE Working Group grades of evidence.
High quality: Further research is very unlikely to change the confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on the confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on the confidence in the estimate of effect and is likely to change the estimate.
Very low quality: The authors are very uncertain about the estimate.
It was adopted as assumed risk in the control, the second highest and second lowest risk of the control group in the included studies.
There was inconsistency in the results. p-Value=0.08 and heterogeneity index of 50%.
Source: Created by GRADE working group – http://www.gradeworkinggroup.org.
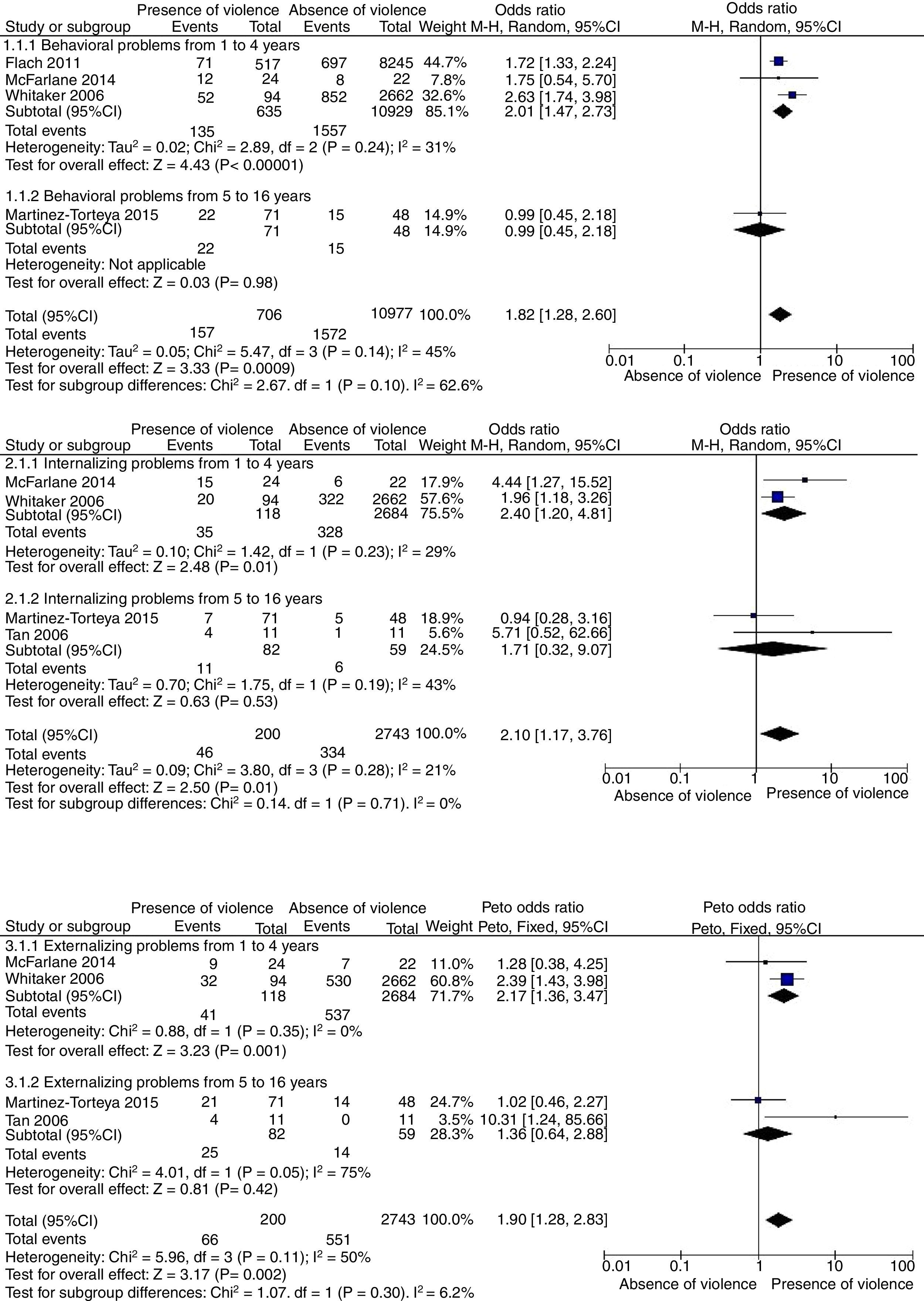
Three meta-analyses were performed (Fig. 2) to assess whether the mother's exposure to IPV during pregnancy increases the child's chance of showing behavioral, externalizing and/or internalizing problems, with analysis of two age range subgroups (<1 to 4 years and 5 to 16 years) compared to children of unexposed mothers.
Four studies3,28–30 allowed a meta-analysis to be performed, which identified a 1.82-fold higher chance of the child having behavioral problems (11,683 participants, OR=1.82, 95% CI: 1.28–2.60, p=0.0009; random effect, p=0.14, I2=45%). The other studies5,16,20 did not provide sufficient information on the exposed and unexposed groups to be included in the meta-analysis and are described individually in Table 1.
For the internalizing problems, data from four studies5,28–30 were analyzed and the meta-analysis showed a 2.10-fold higher chance (2943 participants; OR=2.10; 95%CI: 1.17–3.76; p=0.01, random effect, p=0.28, I2=21%). The same studies analyzed the externalizing problems, and the chance was 1.9-fold higher (2943 participants; OR=1.90, 95% CI: 1.28–2.83, p=0.002; Peto's fixed effect, p=0.11, I2=50%). Table 1 describes the studies3,16,20 that were not included in the meta-analysis due to insufficient information on the exposed and unexposed groups.
DiscussionThe results of this review indicate that women's exposure to IPV during pregnancy during pregnancy increases the chance of children exhibiting behavioral problems when compared to the children of unexposed mothers, both in the analysis of behavioral problems and in the internalizing and externalizing problems, analyzed separately. However, this evidence should be interpreted with caution, since it has low quality. The GRADE method26 initially classifies the observational studies with low quality of evidence; the possible factors that could increase this quality were not met by the included studies, demonstrating a low confidence in the estimated observed effect.
Regarding the outcome of behavioral problems, although the result shows a risk increase of 82%, the support for this evidence is low, mainly due to the inconsistency of the results and study limitations. Moreover, the included studies did not meet the criteria recommended by GRADE to increase the level of evidence, which would be a large effect size and dose-response gradient.27 However, it is important to highlight that confounders that the literature indicate that could interfere in this association12 were controlled, highlighting postnatal violence,3,5,20,28,29 which would be a factor that depicts family dysfunction and the possibility of continuing violence in the child's life.
Although the meta-analysis for the externalizing problem outcome showed a 90% risk, the quality of evidence was also low. However, although the studies did not show homogeneity and one of the studies30 did not use a standardized tool to assess women's exposure to IPV during pregnancy, this result is consistent with a study13 that demonstrated the harmful effects of the prenatal environment on behavioral problems in childhood and adolescence.
The meta-analysis showed that the children of mothers exposed to IPV during pregnancy had a 2-fold higher chance of internalizing problems. The studies showed homogeneity, consistency and direct evidence, but one of the studies30 did not use a standardized tool to evaluate the woman's exposure to IPV during pregnancy, and it was not possible to increase the level of evidence.
The children's age at the time of assessment showed great variation in the five included studies3,5,28–30; consequently, the authors decided to perform a subgroup analysis for two age groups. The results were more consistent in the age range of <1 to 4 years. A probable explanation is the contribution of the sample size from the studies that evaluated this age range. Another aspect that should be considered is that, despite cerebral plasticity in the early stages of development, neural circuits are more vulnerable to prenatal environment disorders than in other developmental periods,14 and the fact that younger children process emotional experiences and traumatic events in different ways at each age.15
Most studies were carried out in developed and Western countries. However, studies carried out in developing countries, such as in Latin America and the Caribbean regions,1 show a high frequency of IPV during pregnancy, indicating that the consequences for children in these and other regions may be even worse. Therefore, the results show the need for studies that assess the effects of prenatal exposure to IPV on the development of children from developing countries and also from eastern culture countries, where IPV is underreported.16
Another important aspect is that the studies did not assess whether different types of violence (physical, psychological, and sexual) had a different impact on the children's behavior. It is already well established in the literature that psychological violence in pregnancy increases the chance of maternal depression.7,8 Although most studies controlled for maternal mental health as a confounding factor, it would also be important to assess what type of violence has the greatest impact on children's behavior.
Possible limitations of this review were the lack of access to the EMBASE database and the database of theses and dissertations. In spite of the diverse databases researched for the study, for any systematic review, there will always be the possibility of failing to include a study difficult to be found in a certain database due to the non-inclusion of the study in the search strategy. It is also necessary to consider the time-lag bias (studies are being carried out, but have not yet been published).
Although the search strategy was comprehensively and carefully performed, an important finding of this review is the scarcity of studies analyzing the association between children's behavioral problems and their mothers’ exposure to IPV during pregnancy, despite its high frequency.1,2
To the best of the authors’ knowledge, to date, no systematic reviews have been conducted on the association between behavioral problems in children whose mothers were exposed to IPV during pregnancy. The strengths of this review also comprise the inclusion of articles that assessed confounding factors and the quality of evidence evaluation using the GRADE method. However, it is important to emphasize that the results are based on a low quality of evidence and that, therefore, it is necessary to consider that for their interpretation.
ConclusionThe results of this study show, based on a low quality of evidence, that prenatal IPV increases the chance of the child presenting behavioral, internalizing, and/or externalizing problems, with more consistent results in the age group of 1 to 4 years.
This study also indicates the need for future research, with high methodological thoroughness, using standardized tools in well-defined age groups (for instance, infants, preschoolers, schoolchildren, and adolescents) and evaluating different types and frequency of violence. Moreover, it is important to control for the confounding factors (such as the child's gender, birth weight and gestational age, social support, and stressful life events) and perform the analysis of stress biomarkers.
It is necessary to analyze the associations between reactions to early adversity and contextual factors, so that the environmental influences and biological susceptibilities that put the child's functioning at risk at the different stages of child development can be identified.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Silva EP, Lemos A, Andrade CHS, Ludermir AB. Intimate partner violence during pregnancy and behavioral problems in children and adolescents: a meta-analysis. J Pediatr (Rio J). 2018;94:471–82.
Study carried out at Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil.