To investigate whether breastfeeding in early life affects blood pressure of preschoolers.
MethodsCross-sectional study nested in a cohort from a municipality in the state of Minas Gerais, Brazil. All children in the cohort were invited for this study. Thus, between 2009 and 2010, blood pressure of 230 preschool children and their mothers, in addition to anthropometric variables, previous history, and socioeconomic status were evaluated. Blood pressure measurement was assessed in the morning, using automatic Omron® HEM-714INT and HEM-781INT devices to measure the blood pressure of preschool children and their mothers, respectively. Logistic regression was used to study the association between breastfeeding and blood pressure. The significance level was set at 5%.
ResultsThis study identified 19 (8.26%) preschool children with high blood pressure (values above the 90th percentile). High systolic blood pressure was associated with low birth weight (OR=5.41; 95% CI=1.45–20.23) and total breastfeeding duration of less than six months (OR=4.14; 95% CI=1.40–11.95). High diastolic blood pressure was not associated with any variable, whereas high systolic blood pressure/diastolic blood pressure ratio was associated with breastfeeding duration of less than six months (OR=3.48; 95% CI=1.34–9.1).
ConclusionThe results of this study indicate that preschoolers breastfed for a period of less than six months were more likely to have high blood pressure when compared to those breastfed for a longer period, suggesting a protective effect of breastfeeding against high blood pressure in this population.
Investigar se aleitamento nos primeiros meses de vida tem influência sobre a pressão arterial de pré-escolares.
MétodosEstudo transversal aninhado numa coorte de nascidos num município mineiro. Foram convidadas para este estudo todas as crianças da coorte. Desse modo, entre 2009 e 2010, foram avaliados pressão arterial (PA) de 230 pré-escolares e de suas mães, além de variáveis antropométricas e pregressas e condição socioeconômica. A medida da PA foi feita de manhã, com os monitores automáticos de braço Omron® modelo HEM-714INT e HEM-781INT para medir a pressão arterial dos pré-escolares e de suas mães, respectivamente. Para o estudo da relação entre aleitamento materno e pressão arterial usou-se a regressão logística. O nível de significância adotado foi 5%.
ResultadosForam identificados 19 (8,26%) pré-escolares com pressão arterial elevada (valores acima do percentil 90). A pressão arterial sistólica (PAS) elevada se associou ao baixo peso ao nascimento (OR=5,41; IC 95%= 1,45-20,23) e ao período total de aleitamento materno inferior a seis meses (OR=4,14; IC 95%= 1,40-11,95). Elevada pressão arterial diastólica (PAD) não se associou a qualquer variável e a PAS/PAD elevadas se associaram ao período de aleitamento materno inferior a seis meses (OR=3,48; IC 95%= 1,34-9,1).
ConclusãoOs pré-escolares amamentados por um período inferior a seis meses, quando comparados com os que amamentaram por um período superior, apresentaram maior chance de estar com pressão arterial elevada, o que sugere efeito protetor do aleitamento materno contra elevação da pressão arterial na população estudada.
Some diseases that are usually observed in adults have been affecting children at an alarming rate; among them, excess weight and high blood pressure (BP) should be highlighted. Excess weight – overweight/obesity – has been considered a worldwide epidemic. The Household Budget Survey 2008–20091 disclosed that this problem affected approximately 33.5% of Brazilian children aged 5–9 years. According to Friedman et al.,2 excess weight often accompanies an increase in BP.
High BP levels in childhood increase the chance of systemic arterial hypertension (SAH) in adults, and also contribute to cardiovascular disease.2 Thus, the identification and early treatment of hypertension in childhood can prevent future adverse outcomes.
The Brazilian Society of Cardiology3 recommends that BP should be measured after three years of age, annually, or before that, when there are risk factors. However, the complex methodology established to verify BP in children makes many professionals exclude it from the routine examination or incorrectly interpret the measured values, which may result in underdiagnosis and undesirable consequences for these individuals.4 Thus, likely due to these factors, the prevalence of high BP in the pediatric group has long been considered irrelevant. However, several studies have identified that this condition has been common at this stage of life.5–11
As with most chronic, noncommunicable diseases, the risk factors for hypertension include genetic components, lifestyle,3,12 and inadequate feeding practices.3,10 Some studies have suggested that breastfeeding may also be an important protective factor against cardiovascular diseases, hypertension, dyslipidemia, and obesity during childhood.13
However, the protective effect of breastfeeding against high BP is still controversial; while some studies have identified this effect,11,14 others have not.9,15
For Balaban and Silva,16 nutritional experiences occurring during infants’ first months of life can affect their susceptibility to chronic diseases in adulthood; this has been called metabolic imprinting, a term that describes a phenomenon by which an early nutritional experience that acts during a critical and specific period of development, which could lead to regulatory mechanism programming, such as BP regulation throughout life.17
In this sense, Horta et al.17 mention that different biological mechanisms can have an effect on this programming, among them the high concentration of long-chain polyunsaturated fatty acids, which are important structural components of cell membrane including the vascular endothelium.
Considering the abovementioned aspects, this study aimed to determine whether breastfeeding in the first months of life influences the BP of preschoolers.
MethodsStudy subjects and settingThis was a cross-sectional study nested in a cohort of individuals born in the municipality of Diamantina, state of Minas Gerais, Brazil.18 Details about the cohort formation and of the cross-sectional study were previously reported in another publication.19 In the present study, the children from the aforementioned cohort were 5 years old, ranging from 4 months older or younger, and were submitted to anthropometric, socioeconomic, and BP assessments.
Diamantina is a municipality located in Vale do Jequitinhonha, in Minas Gerais, Brazil. It has a literacy rate of 83.4% and a human development index of 0.748. Among households, 90.76% are supplied with treated water, 70.7% have a sewage system, and 69.67% have garbage collection services.20
The data collection for this study took place between 2004 and 2005 and between 2009 and 2010. In the first period, data were collected by a nutritionist and students of the Nutrition Course of Universidade Federal dos Vales do Jequitinhonha e Mucuri (UFVJM), and in the second period, by four nutritionists and one student of the aforementioned University Nutrition Course. Before the start of the study, the researchers were trained to standardize the measures.
The children were visited at their homes in both study periods; in the first period all variables were assessed at home, while in the second stage of the study a home visit was conducted in which a questionnaire was applied to the child's parent or guardian, followed by a scheduled day and time for anthropometric and BP measurements of the children and their mothers.
Assessed variablesAmong the assessed variables, the ones used in this study include the following: body mass index (BMI), waist circumference (WC), household income, number of household members, and BP of the children at the age of 5, as well as of their mothers. Additionally, information on body weight at birth and duration of breastfeeding in the first months of life was also collected.
The children's weight was measured using a portable electronic Kratos® digital scale (Kratos®, SP, Brazil), with a maximum capacity of 150kg and precision of 50g; as for the height, it was measured using an Altura Exata® stadiometer (Alturexata®, MG, Brazil) with precision of 0.1cm. WC measurement was carried out with a measuring tape at midpoint between the iliac crest and the last rib.21 These measures were taken according to protocols recommended by Jelliffe,22 on the premises of UFVJM, in the morning.
The cutoff point >1 z-score identified children with excess weight according to BMI/age.23 The World Health Organization's (WHO) Anthro 2005 version 2.0.1 and Anthro 2009 Plus version 3 were used to identify the children's z-scores. It is worth mentioning that the two software programs were used, considering that the children's age during data collection was 5 years, ranging from 4 months older to 4 months younger. For analysis of the variable WC, the risk category values were defined as those above the 75th percentile.
The per capita income of the child's family was calculated based on information about total family income and number of household members. During the study period, the minimum wage was R$ 540.00 in Brazil. This information was obtained through a structured questionnaire administered to the child's mother or guardian during the household interview.
BP was measured on a single occasion, with three measurements made with a 5-min interval between them, preceded by 10min of rest. The average of the three measurements was used for the analysis. Automatic HEM-arm Omron® 714INT and 781INT (Omron®, Netherlands) monitors were used to assess the BP of preschool children and their mothers, respectively. These measurements were obtained according to the manufacturer's recommendations.
BP classification followed the criteria of the VI Guidelines on Arterial Hypertension,3 which considers BP values for children and adolescents according to the percentiles of height for both genders below the 90th percentile as normotensive, as long as they are <120/80mmHg; between 90th and 95th percentiles as borderline, and greater than or equal to the 95th percentile, as hypertension. In this study, for preschool children, “high BP” values were considered when >the 90th percentile, and for the mothers, values greater than or equal to 140/90mmHg.
Maternal breastfeeding was defined according to the recommendations of the WHO.24 Thus, children who were breastfed up to six months, regardless of the introduction of other foods, were considered as receiving breastfeeding. Data on breastfeeding were obtained prospectively from the cohort study, when the children were visited, as well as at home, on a monthly basis.
This study used data from two larger studies entitled “Food and growth in the first year of life: a cohort study”18 and “Determinants of nutritional status of children at five years of age in the city of Diamantina: study of a cohort assessed in the first year of life.”25 Both studies were approved by the Research Ethics Committees of UFVJM, with protocol numbers 011/05 and 039/08, respectively. The children's parents or guardians signed the informed consent to participate in the study.
Statistical analysisLogistic regression analysis was used to determine the influence of breastfeeding on the presence of high BP in preschoolers. Initially, a bivariate analysis was performed and those variables with p-value <20% were selected for the multivariate analysis. The level of significance set to reject the null hypothesis was 95%.
The power of the sample was calculated retrospectively using the statistical software G* Power.26 For this analysis, the parameters used were the odds ratio (OR) of 2.6 for high BP (SBP/DBP) according to the breastfeeding duration obtained at the unadjusted logistic regression analysis, with a maximum probability of error of 5%. The power identified was 99, with the sample being considered adequate.
ResultsThis was a cross-sectional study nested in a birth cohort and, as previously mentioned, the cohort formation and the children's follow-up have been previously published.19 Thus, in search of children for this study, it was decided to study the eligible preschoolers for the cohort and not only those who were followed in the first year of life, in order to avoid significant losses that would invalidate the present study, as there was loss of some children during the follow-up. Therefore, there was a loss of 49 preschoolers in this study.
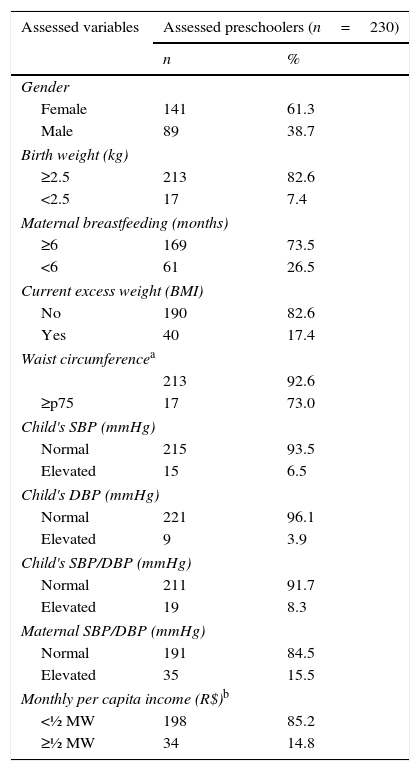
A total of 230 children were evaluated, of whom 19 (8.2%) were classified as having high BP, i.e., SBP/DBP >the 90th percentile, with 6.5% and 3.9% showing elevated SBP and DBP, respectively. The prevalence of breastfeeding in the sixth month of life was approximately 74% (Table 1).
Socioeconomic, maternal, and current and former characteristics of preschoolers. Diamantina, MG-2010.
| Assessed variables | Assessed preschoolers (n=230) | |
|---|---|---|
| n | % | |
| Gender | ||
| Female | 141 | 61.3 |
| Male | 89 | 38.7 |
| Birth weight (kg) | ||
| ≥2.5 | 213 | 82.6 |
| <2.5 | 17 | 7.4 |
| Maternal breastfeeding (months) | ||
| ≥6 | 169 | 73.5 |
| <6 | 61 | 26.5 |
| Current excess weight (BMI) | ||
| No | 190 | 82.6 |
| Yes | 40 | 17.4 |
| Waist circumferencea | ||
| 213 | 92.6 | |
| ≥p75 | 17 | 73.0 |
| Child's SBP (mmHg) | ||
| Normal | 215 | 93.5 |
| Elevated | 15 | 6.5 |
| Child's DBP (mmHg) | ||
| Normal | 221 | 96.1 |
| Elevated | 9 | 3.9 |
| Child's SBP/DBP (mmHg) | ||
| Normal | 211 | 91.7 |
| Elevated | 19 | 8.3 |
| Maternal SBP/DBP (mmHg) | ||
| Normal | 191 | 84.5 |
| Elevated | 35 | 15.5 |
| Monthly per capita income (R$)b | ||
| <½ MW | 198 | 85.2 |
| ≥½ MW | 34 | 14.8 |
MW, minimum wage.
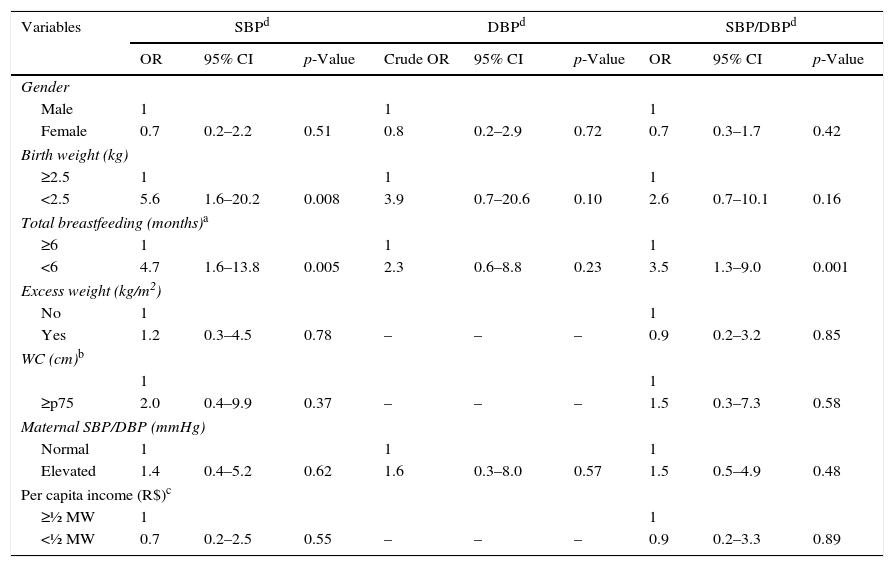
The results of the bivariate analysis of variables associated with elevated systolic and diastolic BP; both are shown in Table 2. It can be observed that birth weight and duration of breastfeeding were associated with SBP levels. No variable was associated with DBP; however, birth weight and duration of breastfeeding were associated with SBP/DBP (Table 2).
Crude odds ratios (OR) and respective confidence intervals (CI) of the analysis of variables associated with blood pressure in preschoolers. Diamantina, MG-2010.
| Variables | SBPd | DBPd | SBP/DBPd | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | Crude OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Gender | |||||||||
| Male | 1 | 1 | 1 | ||||||
| Female | 0.7 | 0.2–2.2 | 0.51 | 0.8 | 0.2–2.9 | 0.72 | 0.7 | 0.3–1.7 | 0.42 |
| Birth weight (kg) | |||||||||
| ≥2.5 | 1 | 1 | 1 | ||||||
| <2.5 | 5.6 | 1.6–20.2 | 0.008 | 3.9 | 0.7–20.6 | 0.10 | 2.6 | 0.7–10.1 | 0.16 |
| Total breastfeeding (months)a | |||||||||
| ≥6 | 1 | 1 | 1 | ||||||
| <6 | 4.7 | 1.6–13.8 | 0.005 | 2.3 | 0.6–8.8 | 0.23 | 3.5 | 1.3–9.0 | 0.001 |
| Excess weight (kg/m2) | |||||||||
| No | 1 | 1 | |||||||
| Yes | 1.2 | 0.3–4.5 | 0.78 | – | – | – | 0.9 | 0.2–3.2 | 0.85 |
| WC (cm)b | |||||||||
| 1 | 1 | ||||||||
| ≥p75 | 2.0 | 0.4–9.9 | 0.37 | – | – | – | 1.5 | 0.3–7.3 | 0.58 |
| Maternal SBP/DBP (mmHg) | |||||||||
| Normal | 1 | 1 | 1 | ||||||
| Elevated | 1.4 | 0.4–5.2 | 0.62 | 1.6 | 0.3–8.0 | 0.57 | 1.5 | 0.5–4.9 | 0.48 |
| Per capita income (R$)c | |||||||||
| ≥½ MW | 1 | 1 | |||||||
| <½ MW | 0.7 | 0.2–2.5 | 0.55 | – | – | – | 0.9 | 0.2–3.3 | 0.89 |
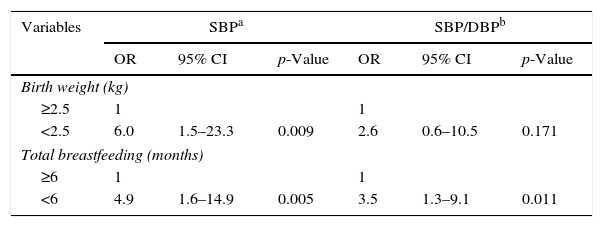
In the adjusted model, birth weight and duration of breastfeeding remained associated with elevated SBP and time of breastfeeding with SBP/DBP (Table 3).
Adjusted odds ratio (OR) and respective confidence intervals (CI) of the analysis of variables associated with blood pressure in preschoolers. Diamantina, MG-2010.
| Variables | SBPa | SBP/DBPb | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Birth weight (kg) | ||||||
| ≥2.5 | 1 | 1 | ||||
| <2.5 | 6.0 | 1.5–23.3 | 0.009 | 2.6 | 0.6–10.5 | 0.171 |
| Total breastfeeding (months) | ||||||
| ≥6 | 1 | 1 | ||||
| <6 | 4.9 | 1.6–14.9 | 0.005 | 3.5 | 1.3–9.1 | 0.011 |
Significance level used: 5% of probability.
Among the assessed preschoolers, the prevalence of high BP was within the national statistics. The findings indicate that children with low birth weight and those who were breastfed for less than six months were more likely to have elevated systolic BP at 5 years of age. Elevated SBP was not associated with any measured variable, and children who were breastfed for less than six months, when compared to those breastfed for longer periods, had higher SBP/DBP.
In Brazil, there are no national statistics on the prevalence of high BP in the pediatric population, which hinders the knowledge of the real problem faced by children. Furthermore, it is believed that high BP is rare in childhood and, thus, its incidence ends up being underestimated due to the difficulty of diagnosis, which requires adequate technique, material, and an appropriate environment for BP measurement.4,27 In addition to being considered as having low prevalence, the measurement of BP is not performed during routine consultations in the pediatric group.
However, it is worth mentioning that the aforementioned studies5–11,28 that assessed high BP in children and/or adolescents identified prevalence rates ranging from 1.7% to 19.9%. None of these studies mentioned the time when the BP was measured, and there was also variation regarding the measurement method, i.e., the equipment used ranged from automatic devices to aneroid sphygmomanometers and the number of measurements and time between the measurements also varied; therefore, these variations may explain differences in these statistics. Additionally, the cutoff points used for high BP classification ranged from values above the 90th or 95th percentiles.
An important aspect that should be mentioned is the possibility that the BP measurement may be the result of white coat syndrome, as in this research BP was measured on a single occasion and, for most children, it was the first time that BP was being measured. This complicating factor, however, must be shared by most of the cross-sectional studies.
It is worth mentioning, however, that careful adherence to the measurement methodology may have minimized this problem. In this research the BP was measured in the morning; three pressure measurements were performed with a 5-min interval between each and the average was used for the analysis. Moreover, the device used for this measurement has an automatic system that detects arrhythmia and a body motion sensor that warns the researchers about the possibility of this syndrome.
Regarding the association between duration of breastfeeding and BP levels, the findings corroborate other studies that have identified an association between shorter duration of breastfeeding and increased BP in childhood.9,11,14,28,29 In the present study, the children who were breastfed for less than six months showed a four-fold increased risk of high SBP, and three-fold higher risk of elevated SBP/DBP ratio, when compared with those who were breastfed for longer periods.
It is worth mentioning that this was cross-sectional study nested in a cohort and, thus, this fact gives greater consistency to the findings, considering that the breastfeeding data collection was performed prospectively, i.e., it was assessed monthly in the first year of life of the children, reducing an important bias, which is the mothers’ recall of their children's eating habits.
As in the present study, Amorin et al.11 and Naghettini et al.28 observed a higher mean SBP in children with shorter breastfeeding duration when compared to those with longer periods. Martin et al.14 also observed similar results in a cohort of children from the United Kingdom. These researchers observed that at 7.5 years of age, children who were breastfed showed 1.2mmHg-lower systolic and 0.9mmHg-lower diastolic BP when compared with those who were never breastfed.
In the study by Lawlor et al.29 with students aged 9–15 years, researchers identified a significant association between time of breastfeeding and BP, with a dose-response effect, i.e., greater reductions in BP occurred among those with longer exclusive breastfeeding time.
In the present study, the prevalence of elevated DBP was lower than elevated SBP, which explains the lack of association with the studied variables. This result was expected, as the studied group consists of preschool children, without any diagnosis of diseases that could affect the circulatory system. And considering that BP measurement evaluates cardiac contraction (SBP) and subsequent blood flow to extra-cardiac body parts (DBP), which is indicative of the strength of blood flow in the arteries, it is not common to find this type of alteration in children considered otherwise healthy, as in this research.
From the perspective of the aforementioned mechanisms proposed in this study about the effect of breastfeeding on BP,16 Forsyth et al.30 developed a study in which babies were fed in the neonatal period with milk formula supplemented with long-chain polyunsaturated fatty acids. These researchers observed that at the end of childhood, these children had a 3mmHg decrease in BP when compared with children who received formula without fatty-acid supplementation.
Although the study developed by Yi et al.,8 with Chinese children, identified that a family history of high BP, waist circumference values, and body mass index were associated with BP of the assessed children, in this study these variables were not associated with BP of the studied preschool children. In the present study, these variables were control variables for the main investigated association.
One limitation of this study is its cross-sectional design, making it difficult to identify a causal association. Randomized clinical trials and cohort studies are more appropriate for causal identification. Additionally, other variables such as diet and paternal hypertension were not studied; these can have a confounding effect on the observed association.
The results of this research show that preschool children who were breastfed for less than six months, when compared to those breastfed for a longer period, were more likely to have with high BP, suggesting a protective effect of breastfeeding against high BP in the studied population.
FundingFundação de Amparo à Pesquisa do Estado de Minas Gerais – Fapemig (Process n.: APQ-00428-08).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Nobre LN, Lessa AC. Influence of breastfeeding in the first months of life on blood pressure levels of preschool children. J Pediatr (Rio J). 2016;92:588–94.