To review the screening, diagnosis, evaluation, and treatment of intoxication by alcohol and other drugs in children and adolescents in the emergency scenario.
Data sourceThis was a narrative literature review.
Data summaryThe detection of this problem in the emergency room can be a challenge, especially when its assessment is not standardized. The intentional and episodic use of large amounts of psychoactive substances by adolescents is a usual occurrence, and unintentional intoxication is more common in children younger than 12 years. The clinical picture in adolescents and children differs from that in adults and some particularities are important in the emergency scenario. After management of the acute condition, interventions targeting the adolescent at risk may be effective.
ConclusionThe diagnosis and treatment of intoxication by alcohol and other drugs in adolescents and children in the emergency scenario requires a systematic evaluation of the use of these drugs. There are few specific treatments for intoxication, and the management comprehends support measures and management of related clinical complications.
Revisar o rastreamento, diagnóstico, abordagem e tratamento das intoxicações por álcool e outras drogas de crianças e adolescentes no contexto de emergência.
Fontes dos dadosFoi realizada uma revisão narrativa da literatura.
Síntese dos achadosA detecção desse problema na sala de emergência pode ser um desafio, especialmente quando sua avaliação não é padronizada. O uso intencional e em grandes quantidades episódicas de substâncias psicoativas é o padrão em adolescentes e a intoxicação não intencional é mais comum em crianças menores de 12 anos. O quadro clínico em adolescentes e em crianças difere dos adultos e algumas particularidades são importantes no contexto de emergência. Após o manejo do quadro agudo, intervenções visando o adolescente de risco podem ser efetivas.
ConclusãoO diagnóstico e tratamento das intoxicações por álcool e outras drogas em adolescentes e crianças em emergência requer uma avaliação sistemática do uso dessas drogas. Há poucos tratamentos específicos para intoxicação e o manejo é de suporte e das complicações clínicas relacionadas.
The use of psychoactive substances (PAS) among adolescents is a worldwide problem. In Brazil, heavy episodic drinking is still higher among boys (24%), but has increased among girls (from 11% to 20%).1 Drug use, except for alcohol and tobacco, was reported by 24% of elementary and high school students; energy drinks combined with alcohol (15%), marijuana (6%), inhalants (9%), anxiolytic drugs (5%), and cocaine (2.5%) were the most prevalent.2 In pediatric emergencies, a higher proportion of adolescents using PAS is expected; patients present due to intoxication symptoms, complications of preexisting diseases, and traumatic injuries.
The challenge in the care of these patients starts at problem detection. When there is no established protocol for the assessment of PAS use in the emergency unit, the frequency and severity of use are usually underestimated.3 The delay in the diagnosis or non-diagnosis of a disorder caused by PAS use in the emergency room may increase hospitalization time, costs, and the risk of rehospitalization.4
The treatment of PAS-related intoxication among adolescents initially involves the diagnosis and symptomatic treatment and/or approach of the other consequences of their use. After the acute condition is managed, the emergency unit is an important place of referral for treatment and for preventive approaches in cases of disorders related to PAS use. The aim of this article was to describe the assessment, diagnosis, symptoms, and initial approach of PAS intoxication, as well as brief interventions for at-risk adolescents.
DiagnosisSubstance use surveillanceA good screening tool to be used in the emergency room should be brief, easy to implement, and have adequate sensitivity and specificity to complement patient clinical evaluation and to provide subsidies for the therapeutic intervention. The literature is quite controversial in the indication of screening instruments to detect the use or diagnosis of problems involving PAS, and there is no specific guideline for the assessment of young individuals.5 Currently, there are some validated questionnaires, as well as some biochemical analysis tests that evaluate the presence of PAS in biological matrix.
Several tools have already been tested for this population, but the care, relax, alone, family, friends, trouble (CRAFT) and the alcohol use disorder identification test (AUDIT) are the tools with the best performance.6 The advantage of CRAFT is that it also assesses consumption of multiple drugs with a moderate sensitivity and specificity. For alcohol issues, the AUDIT showed the highest sensitivity and specificity (95% and 77%, respectively), and it can be applied in approximately 2min. The most appropriate cutoff to determine problems related to alcohol consumption is 3.7 It is also worth noting that the question “How often did you drink in the previous month?” when the answer was equal to or greater than three episodes, showed a sensitivity of 90% and specificity of 84% to detect this problem.7
The biochemical tests to detect substance use have a practical usefulness in several clinical situations. The ethyl alcohol and rapid urine tests were shown to be interesting alternatives in the emergency unit, due to the fast results and their ability to identify the recent PAS intake.8 Testing the air expired through the ethyl alcohol meter is low cost, noninvasive, and has a good correlation with alcohol consumption, being very useful for the assessment of recent alcohol intoxication.
Urine tests are performed using a test tape that can measure the presence of metabolites of the most varied PAS classes that have been recently consumed. The detection time is variable for each substance: marijuana from one to 30 days (depending on whether the use is acute or chronic), cocaine from one to three days, amphetamines from two to four days, benzodiazepines and barbiturates up to seven days.9
Urine screening tests may show false-negative results due to high cut-off points, but a false-positive test is unlikely, especially in an emergency environment, where the pretest probability is already high if the test is performed due to clinical suspicion.8
Drug testing in adolescents always includes important ethical and confidentiality issues with parents. Generally, the adolescent should always consent to the test. In serious situations, such as accident victims, suicide attempts, seizures, or other risk situations in which the patient's consent cannot be obtained, it is justified to perform them without his/her consent.8 Regarding confidentiality, the adolescent should authorize the parents’ access to the result, which should only be informed to the parents against the patient's wishes if an acute risk situation is identified.8
Evaluation and management of substance useWhen an adolescent that uses PAS is identified, a more detailed assessment of this use becomes necessary. In an emergency context, information on the concomitant use of other PAS, amounts, and time since the last intake are essential for the management. Based on these data, it should be estimated whether the intoxication symptoms will increase or decrease in the next few hours. If possible, it is important to obtain information on the age of onset and progression for the use of each PAS, frequency and variability of use, as well as the direct and indirect consequences of use in relation to the domains: family, educational, social, psychological, and medical. The use of adult diagnostic criteria is strongly debated in this context, since the abstinence and tolerance criteria do not adequately apply to adolescents.10 Thus, the focus is to identify the adolescent at risk for the development of PAS abuse.
Alcohol intoxicationAlcohol intoxication is common among adolescents, and approximately 15% of users ages 15 and older engage in heavy episodic drinking. The main mechanism of the pharmacodynamics of alcohol is the facilitation of inhibitory transmission of the central nervous system (CNS). The symptoms of acute alcohol intoxication are dose-dependent, related to the serum level that is reached, but there is great individual variability in the dose needed to produce them.11 The most common symptoms are: mood or behavior change, slurred speech, lack of coordination, unstable gait, nystagmus, attention or memory deficit and, in more severe cases, stupor or coma. It is important to emphasize that the effects on the consciousness level follow a continuum according to the blood alcohol concentration, ranging from mild sedation to coma.11 Additionally, alcohol can cause several potentially lethal metabolic effects. Hypoglycemia is a rare effect in adults, but children and adolescents are at greater risk of developing it.12 Other metabolic effects are acidosis, hypokalemia, hypomagnesemia, hypoalbuminemia, hypocalcemia, and hypophosphatemia. Cardiovascular effects may also occur: tachycardia, peripheral vasodilation, and volume depletion, which may contribute to the induction of hypothermia and hypotension.11
In young individuals, alcohol intoxication tends to be more severe than in adults, as they usually do not show tolerance to the effects developed by repeated exposures.13 Adolescents present a higher probability of intentional intoxication, especially in a pattern known as heavy episodic drinking (binge drinking), which consists in the intake of large amounts in a short period of time. There are cultural factors that even stimulate this and other practices such the “warming up,” as it is known in Brazil, which is the consumption of alcohol when getting ready to go out to parties.
The pattern of repeated binge drinking is related to brain disorders that may develop into alcoholism in adulthood.14
Management of alcohol intoxicationBefore starting treatment, it is important to estimate the blood alcohol content (BAC). If the meter is available, it is a good option, because the expired air has a good correlation with the alcohol levels. If BAC is increasing, the adolescent should be closely monitored for CNS depression. When this objective measure is not available, it can be estimated by the amount consumed and how long the last consumption was made. For a rough estimate in older adolescents, the metabolization of one dose (14g of ethanol) per hour can be calculated.
The management of acute intoxication for all individuals should be focused on the clinical complications present, such as correction of hypoglycemia, hypomagnesaemia, or management of restlessness. For severe restlessness, typical antipsychotics, such as haloperidol, should be preferred because of a lower chance of alcohol interaction. Gastric content aspiration should be prevented with the administration of antiemetics, as well as maintaining airway patency, depending on the degree of patient sedation. Venous access is obtained, if necessary, to ensure fluid administration.
In children and adolescents, the treatment follows the same guidelines, with special attention to hypoglycemia and hypothermia.12 Some studies have shown a beneficial effect of metadoxine in accelerating alcohol metabolism and decreasing the time of intoxication with a single dose of 900mg IV in adults.15 There are no studies on metadoxine use for this purpose in the pediatric population.
Marijuana intoxicationMarijuana is the second most commonly used drug by adolescents. The usual presentation of intoxication involves the following effects16: euphoria, pleasurable feelings, decreased anxiety, depression, and attention. Some users who are more anxious, psychologically vulnerable, or inexperienced with the drug may present with increased anxiety, dysphoria, and panic attacks. Vasodilation and redness of the conjunctivae (one of the most characteristic signs of marijuana use) are common, and postural hypotension and syncope may also occur. In some cases, there is an increase in blood pressure, dry mouth, increased appetite, nystagmus, and slurred speech.16 Changes in sensory perception may occur: colors become clearer and music more vivid. Perception of space, reaction time, attention, concentration, memory, and risk assessment are also altered. The latter remain altered for much longer than the subjective intoxication sensation and these effects may persist for 12–24h after use.
Marijuana increases heart rate to as much as 160 beats per minute for a few minutes after use,16 a dose-dependent effect that is probably not relevant in young individuals, unless they have a previous cardiovascular problem. However, cases of marijuana-associated arrhythmias have been reported. Its use increases the relative risk of myocardial infarction by 4.8-fold in the one-hour period after its use.17 Among patients admitted to general hospitals in France due to marijuana use, 29% of patients had some cardiovascular complications, of whom 3.5% had myocardial infarction, and 2% had a stroke, with no apparent cause other than marijuana use.18 Additionally, 31% of the patients had respiratory complaints (dyspnea or hemoptysis), of whom 3.5% had spontaneous pneumothorax.
The occurrence of psychotic outbreaks associated with the use of marijuana when utilized in large amounts or in preparations with higher concentrations is not infrequent.16,19 Up to 9.5% of users may experience psychotic episodes that last longer than the intoxication.19
Management of marijuana intoxicationThe management of cannabinoid intoxication is predominantly support therapy. Most cases of mild intoxication resolve themselves within a few hours, and may be better comforted by accommodating patients in dimly-lit rooms, fewer stimuli and, in very agitated cases, benzodiazepines such as diazepam at a dose of 5mg by oral route. In cases with cardiac or respiratory complications, these should be managed according to the underlying etiology. The use of activated charcoal is not recommended for cases of marijuana ingestion.20 Cases with psychosis should be treated with antipsychotics, preferably atypical drugs, due to the lower incidence of adverse effects.
Ecstasy intoxication3,4-Methylenedioxymethamphetamine (MDMA), popularly known as ecstasy, is a substance commonly consumed by individuals attending raves. There is a considerable upward trend in prevalence, and its use is associated with potentially fatal complications. The acute effects of MDMA intoxication are a mix of the effects of hallucinogens and stimulants. Its most common physiological effects are hyperthermia, hypertension, tachycardia, sweating, hyponatremia (due to inappropriate secretion of antidiuretic hormone), muscle tension, bruxism, and insomnia.
The psychological symptoms are euphoria and changes in sensory perception (increased tactile stimulation, hallucinations, and increased perception of colors and sounds); panic attacks and toxic psychoses can also occur. The peak of action occurs around 2h after consumption, with a half-life of around 8h. It is important to note that the pharmacokinetics of MDMA are non-linear, i.e., small increases in the oral dose can greatly increase serum concentration.
Ecstasy intoxication managementAcute intoxication management is mainly supportive, directed to the symptoms shown by the patients. The most concerning symptom is hyperthermia, potentiated by the context in which the drug is used, in a warm environment and with intense physical activity.21 Restlessness and seizures should be controlled with benzodiazepines, cardiovascular effects with beta-blockers, and temperature with external cooling measures. Attention must be paid to water-electrolyte imbalance due to the intense water consumption, which is common among these users. Antipsychotics should be avoided, due to the decrease in the convulsive threshold.22
Cocaine intoxicationThe administration route of cocaine will influence its onset of action, intensity, and duration of effects. Crack smoking and injectable routes will have more intense, short-lived effects, but with a post-effect of craving and dysphoria. As for the inhaled route, the effects are less intense, but have a longer duration. Emergency care is generally sought due to psychological or cardiac effects. The common effects are excitement, euphoria, and high self-esteem, but high doses lead to anxiety, restlessness, irritability, paranoid symptoms, and intense craving. Regarding cardiac effects, cocaine results in a dose-dependent effect of increased heart rate, blood pressure, and vasoconstriction. There is an increase in cardiac demand, and ischemia, ventricular and supraventricular arrhythmia may occur (either due to the direct effect or ischemia).
The drug use causes an increase in temperature, decreased perspiration and peripheral circulation, and may result in severe hyperthermia.23 Complications that occur in the CNS are seizures, cerebral ischemia or hemorrhage, headache, and focal neurological symptoms. Seizures may occur after the use of large amounts, even without previous epileptic focus. From the pulmonary point of view, pneumothorax, pneumomediastinum, or pneumopericardium can occur as a consequence of Valsalva practice to prevent drug exhalation. Vasoconstriction and increased coagulation can lead to ischemia and infarction of several organs in addition to the heart and brain, such as the lungs, kidneys, spleen, and intestines.
Concomitant alcohol intoxication increases the risk and severity of complications. Another important factor are the adulterants present in powdered cocaine, with levamisole being the most important. This can lead to agranulocytosis and cutaneous vasculitis with skin necrosis.24
Management of cocaine intoxicationThe diagnosis is clinical and may be aided by urinalysis or exams to assess complications, such as electrocardiogram, cardiac enzymes, and cranial tomography, among others. Initial management is supportive and the treatment of restlessness, hypertension, and hyperthermia, or the present complications should be prioritized. The use of benzodiazepines, such as diazepam, is the treatment of choice for restlessness and to relieve cardiovascular symptoms. Patients with hyperthermia should be cooled quickly, ideally within 30min. Routine treatment should be adopted in case of complications, but some care must be taken. Beta-blockers should not be used, as they may aggravate vasoconstriction and hypertension.
Accidental intoxication in childrenRecently, accidental consumption of PAS by children has become more common. When the ingestion has not been observed by an adult, it takes a high degree of suspicion to make the diagnosis. The presentation of psychiatric and neurological symptoms in children without an identifiable pathology should indicate the possibility of accidental intoxication by some PAS. Children tend to present with ethanol intoxication when there is accidental consumption of any product that contains it in their composition, such as mouthwashes, cosmetics, cleaning products, or beverages left by their parents at home. Making such substances inaccessible to children significantly reduces the likelihood of accidents.25
In particular, there are reports of increased frequency of marijuana poisoning in children in the United States, concentrated in states in which it has been decriminalized.26 Marijuana legalization has made it possible to market several edible presentations of this drug, including some forms of candy and sweets, which may inadvertently be consumed by children.27
The main symptoms seen in the emergency room in children under 3 years who consumed marijuana include sinus tachycardia (58.6%), mydriasis (48.3%), decreased level of consciousness (34%, Glasgow Scale <12), somnolence (24%, Glasgow Scale 12–14), hypoventilation (20.6%), restlessness (10.3%), and seizures (23.53%).27 In older children, neurological symptoms, especially sedation, are also more common, but they may also present with ataxia, restlessness, irritability, or gastrointestinal symptoms. Cardiorespiratory symptoms are rarer.26
Accidental exposure to marijuana usually does not lead to serious consequences, but can result in significant morbidity due to the need for treatment and emergency care, such as exams and procedures.28 Unintentional exposures to cocaine are rare in children (6%), but result in a more serious clinical picture than exposure to other substances.29 A retrospective study with children under the age of 3 years admitted to the emergency unit with confirmed exposure to cocaine29 showed that the most common symptoms are tachycardia (50%) and seizures (33%), followed by restlessness (25%), decreased level of consciousness (22%), gastrointestinal symptoms (17%), fever (14%), hypertension (14%), respiratory depression (11%), cyanosis (8%), mydriasis (8%), and ataxia (8%). Approximately 40% may require intensive care, and 27% have more severe events, such as multiple seizures, need for intubation, renal failure, and rhabdomyolysis.23 Respiratory symptoms (especially when exposed to crack cocaine) and fever may occur.30
Management is predominantly supportive: patients with cardiac manifestations should be monitored for ECG and cardiac enzymes for 8–12h in the absence of complications, which should be treated according to current protocols. The use of activated charcoal for detoxification at a dose of 0.5–1mg/kg body weight may be required.31 In children, accidental intoxication by MDMA is an important differential diagnosis of seizures with hyperthermia, and parents usually deny substance use.32
Brief interventionAdmission to an emergency room after PAS intoxication, as well as being treated for a complication of such an event, is a window of opportunity to use an intervention directed at the adolescent and parents/guardians, aiming to make them ponder on the use of these substances. The brief intervention (BI) is based on motivational interview (MI) techniques and thus comprises an empathetic, non-judgmental, and non-confrontational approach aimed at counseling and the development of motivation for a change in behavior.33
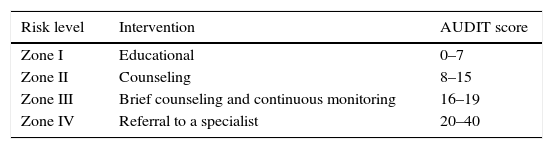
One of the most preeminent manuals on BI for alcohol users suggests evaluating the risk zone for alcohol use before applying the intervention, according to the AUDIT score. Based on that, the most recommended conduct should be applied, according to Table 1. The educational conduct is to provide information about the risks associated with alcohol use and, whenever possible, to provide a brochure. The counseling means providing feedback on the AUDIT result, educating the individuals about the risks, and advising them on how to change this behavior.
BI, in addition to providing risk education and feedback, also supports the idea of engaging young individuals in behavior changes by setting goals for these changes. In this situation, it is important to also counsel the family to monitor these objectives and to provide information on where to seek help, if necessary. Individuals with AUDIT scores above 20 are those who already have a pattern of alcohol dependence and should therefore be referred to a specialist for treatment of the disorder.33
Most randomized clinical trials involving BI in the emergency room for young individuals with acute alcohol intoxication (AAI) were carried out in the United States and Europe, and only one study was conducted in Brazil.34 The largest study that is still being developed is being carried out in Germany. HaLT (stop – close to the limit) is a BI-based prevention project for young individuals with AAI in the emergency room that has already been implemented in more than 170 locations.35
Most studies sought to evaluate, as primary outcome, the reduction in alcohol consumption after a BI. However, many studies did not find a significant difference in relation to the control groups. This result is explained, for the most part, by the fact that the control group itself also decreased alcohol consumption after the emergency admission. Overall, the studies used a BI based on MI techniques, lasting approximately 45min, and some studies also used approaches with parents.33,36
Although the findings were inconclusive in relation to the total amount of alcoholic beverages ingested after the BI in emergencies, it was observed that young individuals who were submitted to a BI had a significant reduction in secondary outcomes, such as number of ingested doses and number of drinks per week, days on which alcoholic beverages were ingested, and number of heavy drinking episodes in a follow-up of up to 12 months.37,38 Another interesting finding was a decrease in car accidents related to alcohol consumption in those who were submitted to a BI.38
The only study developed in Brazil showed a predominantly male population (90.3%) and a high prevalence of alcohol dependence (37.9% in the BI group; 35.2% in the control group), demonstrating that, in this country, interventions aimed at the treatment may be as important as interventions focused solely on prevention. In that study, there was no significant difference between the groups, but there was an overall decrease in alcohol consumption in the three-month follow-up.34
The BI is well established for adults that seek emergency care after intoxication episodes, however this intervention has not shown superiority over control conditions in adolescents. This might be related to the importance of integrated approaches including the family in these cases.
ConclusionCases of PAS intoxication, whether accidental or intentional, are common and should have a high level of suspicion. It is important for the clinician to be aware of intoxication signs, as the clinical picture can be easily mistaken as other problems. Emergency treatment is predominantly supportive, but it should be remembered that most cases will require care for the underlying causes of intoxication. Moreover, getting to emergency care due to PAS intoxication is a window of opportunity for the implementation of prevention measures.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Pianca TG, Sordi AO, Hartmann TC, von Diemen L. Identification and initial management of intoxication by alcohol and other drugs in the pediatric emergency room. J Pediatr (Rio J). 2017;93:46–52.