To analyze gastroschisis annual incidence, mortality rates, and trends in the Brazilian state of Rio Grande do Sul from the year 2000 to the year 2017.
MethodPopulation-based study with the analysis of the temporal trend of gastroschisis annual incidence and mortality rates. Data were obtained from the Live Birth Information System and the Mortality Information System, with the analysis performed by polynomial regression modeling.
ResultsThere were 2,612,532 live births, 705 hospitalizations, and 233 deaths due to gastroschisis. The annual incidence of gastroschisis was 2.69 per 10,000 live births. The annual incidence rate increased by 85% in the total period (p = 0.003), and mortality was 33% in the 2000-2017 period. Maternal age < 25 years was a risk factor for gastroschisis (p < 0.001). Children were more likely to be born weighing < 2,500 g (p < 0.001) and with a gestational age < 37 weeks (p < 0.001). The annual incidence trend was to increase, and the mortality trend was to decrease.
ConclusionSimilar to what has been described in several regions/countries, there was a trend showing an 85% increase in the annual incidence of gastroschisis (p = 0.003) and the mortality was 33% with a trend of decreasing (p = 0.002).
Gastroschisis is a malformation of the abdominal wall, almost always to the right of the umbilical cord, which probably results from the rupture of the physiological hernia in the embryonic period.1
Although the annual incidence of most congenital anomalies is constant across geographies, gastroschisis shows an increased annual incidence in several regions/countries worldwide.2-4 Its prevalence ranges from 1 to 5 per 10,000 live births and has increased three times in the past 10 years.5 Some studies predict a possible gastroschisis pandemic, with an increased rate of up to 300% in about 20 years.4,6
Gastroschisis mortality has decreased in the past 60 years in both developed and developing countries but not in underdeveloped countries. Developed countries have gastroschisis mortality rates below 10%,7 while developing countries have intermediate results, and underdeveloped countries may have mortality rates ranging from 75% to 100%.8
The morbidity of patients with gastroschisis remains high.7 They are frequently reoperated upon and require long hospital stays.7,9
Studies on gastroschisis conducted in Brazil have frequently presented a relatively small number of cases, with populations localized to a specific hospital and almost always with fewer than 50 cases.10,11
To the best of the authors’ knowledge, only one study on gastroschisis prevalence and trend analysis with a large population database was found that used data from the state of São Paulo, Brazil.12 The authors were unable to find a study on gastroschisis annual incidence, temporal trend analysis, and mortality with population data from the state of Rio Grande do Sul, Brazil.
The objective of this study was to evaluate gastroschisis annual incidence and mortality and conduct a temporal trend analysis in extreme Southern Brazil.
Material and methodsStudy design, location, and periodThis is a population-based study with a temporal trend analysis using data from children born alive with the diagnosis of gastroschisis, in the state of Rio Grande do Sul and its health macro-regions, from 2000 to 2017.
Data on live births, hospitalizations, and mortality related to gastroschisis were obtained from the electronic address of the Health Department of the state of Rio Grande do Sul, Epidemiological Surveillance Tabulation,13 and the Informatics Department of the Unified Health System.14 The systems accessed were: Live Birth Information System (Sistema de Informações sobre Nascidos Vivos - SINASC) and Mortality Information System (Sistema de Informações sobre Mortalidade - SIM). The data were surveyed in 2019.
Population and inclusion and exclusion criteriaThis study analyzed data on the hospitalization of newborns diagnosed with gastroschisis (ICD Q79.3), which was coded according to the standards of the International Classification of Diseases 10th revision (ICD-10).15
The variables analyzed were sex, race/color of the children, maternal age (< 20 years, 20 to 24 years and ≥ 25 years), weight (< 2500 g and ≥ 2500 g), duration of pregnancy (22 to 36 weeks and 37 to 42 weeks), hospitalization rate (annual incidence), and mortality rate. As gastroschisis is a congenital disease, the patients were on their first day of life.
Study protocolRates were calculated based on hospitalizations due to gastroschisis, selected using the “SINASC” database of the state of Rio Grande do Sul.13 Mortality was determined based on a survey of the “SIM” database of Rio Grande do Sul, using Q79.3 gastroschisis as the basic cause of death.13 Rates (sex, race/color of the children, maternal age, weight, duration of pregnancy, annual incidence, and mortality) were calculated as the ratio between the number of events observed and the population of live-born children in that year and location multiplied by 10,000 live births.
Statistical analysisMortality and annual incidence rate trends were analyzed using polynomial regression modeling, considering the rates as dependent variables (y) and the year of birth as an independent variable (x). The “year” variable was transformed into the year-centered variable (x-2008), and the series were smoothed using a three-point moving average. Linear (y=β0+β1x1), quadratic (y=β0+β1x1+β2x2), and cubic (y=β0+β1x1+β2x2+β3x3) polynomial regression models were assessed. Trends were considered significant when the estimated model obtained a p-value <0.05. The dispersion diagram, determination coefficient (R2), and residue analysis were also considered while choosing the best model. When all criteria were significant for more than one model and the determination coefficient was similar, the simplest model was chosen. The chi-square test was used to analyze some variables, with a significance level of 5% and confidence intervals (95% CI). The analyses were performed using the Microsoft Excel software version 1912 and the Epi Info software version 7.2.3.1.
Ethical aspectsSince the authors used secondary public domain data, this study did not require an evaluation by the Human Research Ethics Committee, according to resolution number 510/April 7, 2016, of the National Health Council.16
ResultsA total of 2,612,532 live births were analyzed. Of these, 705 patients were born with gastroschisis from 2000 to 2017. In the same study period, 233 (33.2%) deaths occurred due to gastroschisis as the basic cause (Tables 1 and 2).
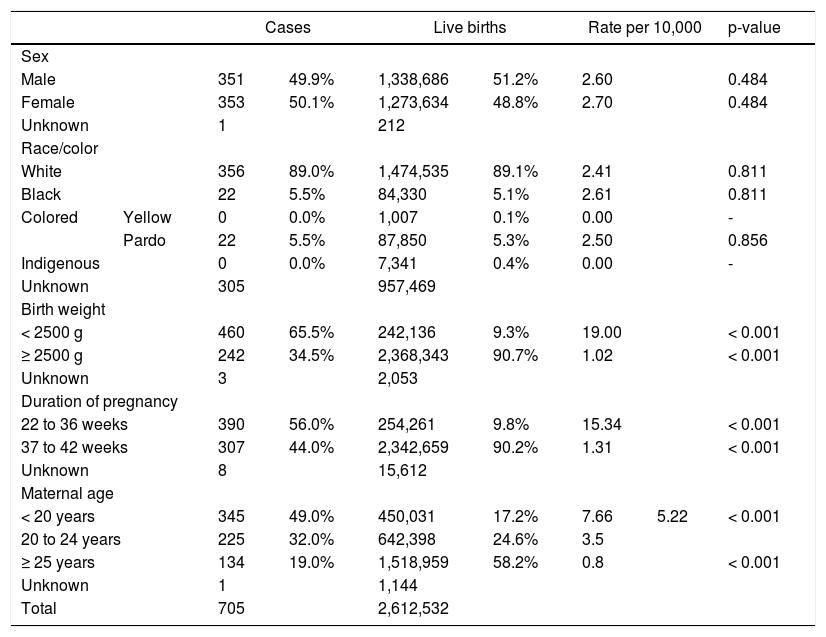
Maternal and infant characteristics regarding sex, race/color, birth weight, duration of pregnancy, and maternal age in Rio Grande do Sul, Brazil, 2000-2017 (Maringá, 2020).
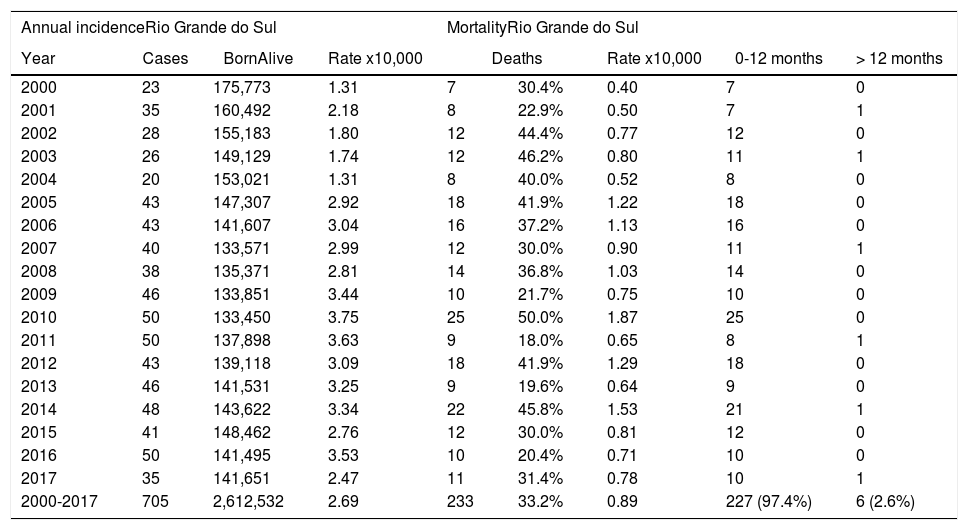
Annual incidence, mortality rates, trends and overall mortality of gastroschisis in Rio Grande Do Sul (2000 – 2017).
The incidence of gastroschisis in the 2000 to 2017 period in Rio Grande do Sul was 2.69 cases per 10,000 live births (Table 2). When considering mothers aged < 25 years, the incidence increased to 5.22 cases per 10,000 live births, and when considering mothers aged < 20 years, the incidence increased to 7.66 cases per 10,000 (Table 1). The chi-square test comparing the maternal age < 25 years with maternal age > 25 years showed a relative risk of 5.9 and p < 0.001; that is, the chance of having a child with gastroschisis was 5.9 times higher for mothers aged < 25 years than for mothers aged > 25 years (Table 1).
The analysis of birth weight showed that 65.5% of the children with gastroschisis weighed < 2500 g, a higher percentage than that of the population of live births, which was 9.3% (Table 1). The comparison between children with and without gastroschisis weighing < 2500 g at birth showed a relative risk of 7.0; that is, the chance of a child with gastroschisis weighing < 2500 g at birth was 7 times higher than that of a child without gastroschisis (Table 1).
Children with gastroschisis had a gestational age of < 37 weeks at birth in 56% of the cases, and 9.8% of the cases were live births. The chi-square test comparing children with and without gastroschisis aged < 37 weeks showed a relative risk of 5.7; that is, the chance of a child with gastroschisis being born aged < 37 weeks was 5.7 times higher than that of a child without gastroschisis (Table 1).
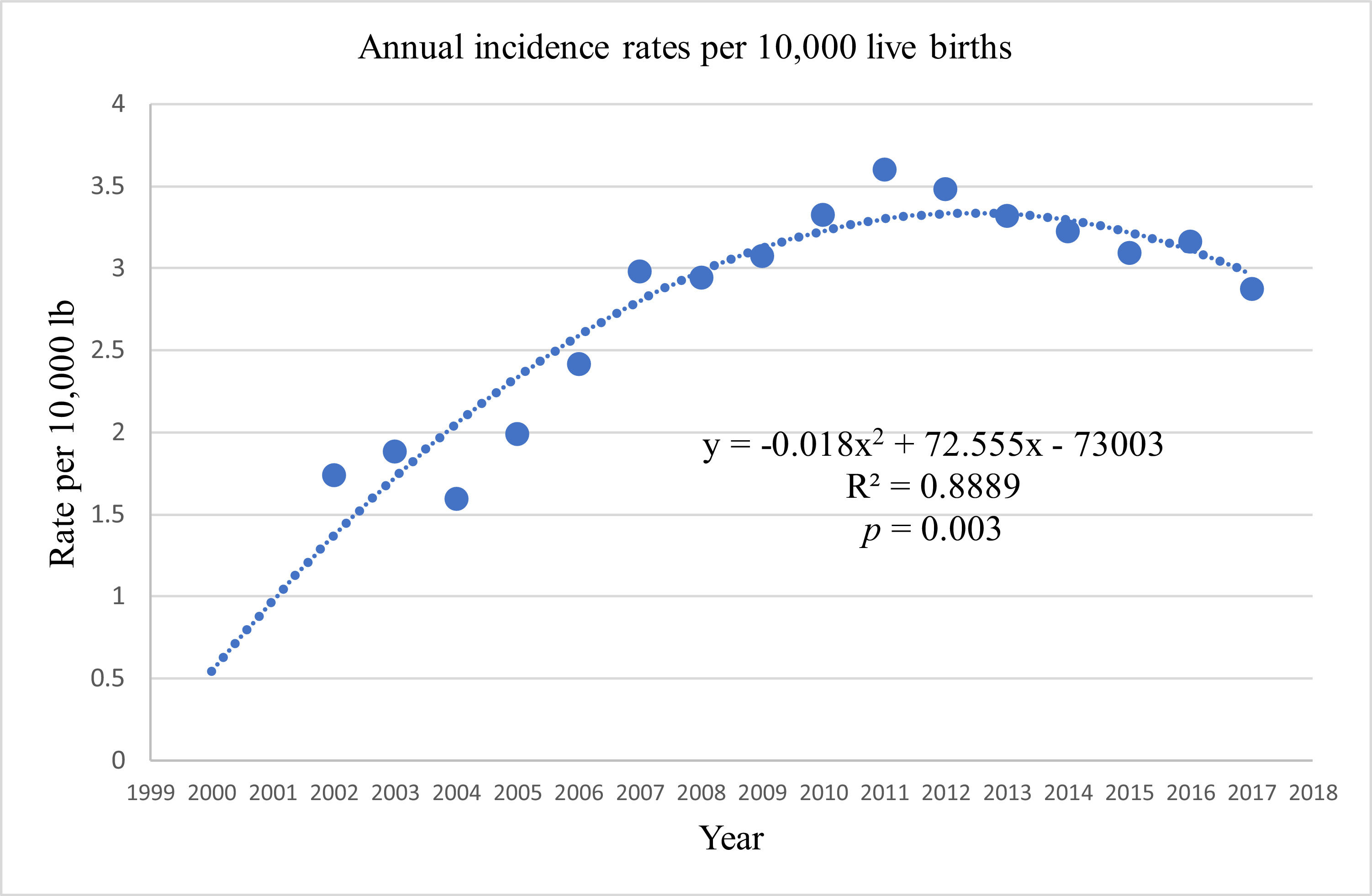
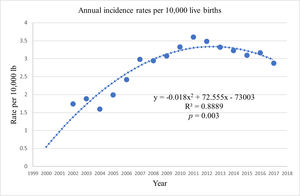
The annual incidence rate of gastroschisis in the population of Rio Grande do Sul ranged from 1.31 in 2000 to 3.75 in 2010 (Table 2), showing an increase of 184% (Table 2). Polynomial regression analysis showed an increasing gastroschisis annual incidence trend in Rio Grande do Sul from 2000 to 2010 and a decreasing trend from 2010 to 2017. The total period (2000 to 2017) showed an increasing annual incidence rate of 85% with a p-value = 0.003 (Table 2 and Fig. 1).
Polynomial regression analysis also showed that all macro-regions (MSs1) in Rio Grande do Sul initially had an increase in the annual incidence trend, with five out of the seven MSs showing a decreasing trend after 2011. In all regions, the increasing trend was greater than the decreasing one. Although there was an increasing trend, the p-value was significant for the entire state of Rio Grande do Sul (p = 0.003) and for three MSs (p < 0.05) (Table 2).
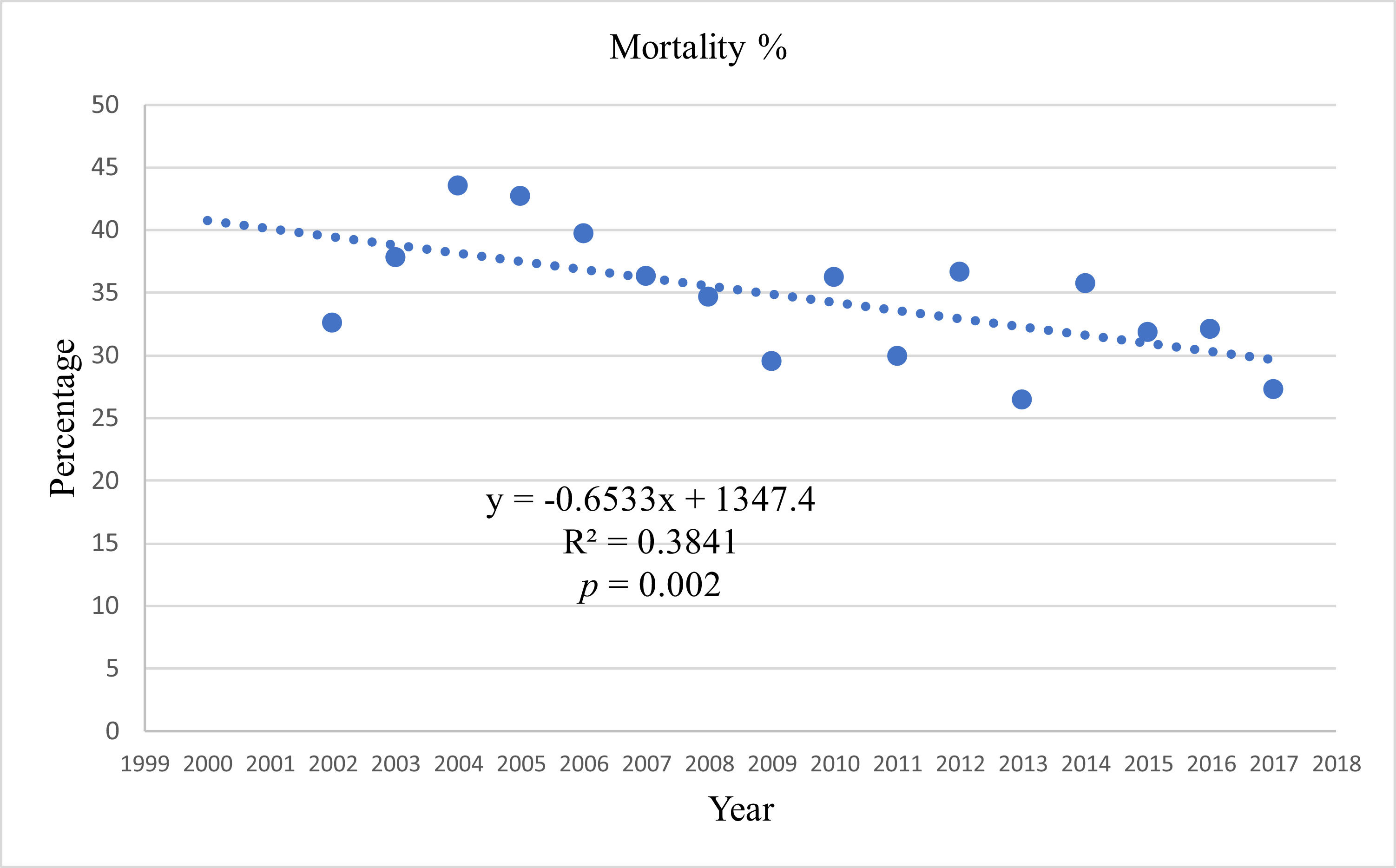
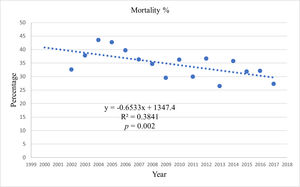
The polynomial regression analysis of mortality comparing the percentage of deaths and the number of cases per year showed a decreasing trend with statistical significance (p = 0.002) (Table 2 and Fig. 2).
The total mortality of patients diagnosed with gastroschisis in Rio Grande do Sul from 2010 to 2017 was 33.2%, ranging from 18% to 50% depending on the year analyzed (Table 2).
DiscussionTo the best of the authors’ knowledge, only one study on gastroschisis prevalence and trend analysis with a large population database was found that used data from the state of São Paulo, Brazil.12
The authors of the present study were unable to find a study on gastroschisis annual incidence, temporal trend analysis, and mortality with populational data from the state of Rio Grande do Sul, Brazil, this is probably the first study.
This study identified an increasing trend in the annual incidence rate of gastroschisis from 2000 to 2010 and a decreasing trend from 2010 to 2017, although with a less marked curve than the increase. It is important to highlight that the modification from the increasing trend curve from 2000 to 2010 to the decreasing trend curve from 2010 to 2017 did not revert the initial increase, resulting in a statistically significant increased incidence of gastroschisis in the total study period. Similar gastroschisis prevalence changes have been previously described by Allman.7
In the present study, the annual incidence of gastroschisis was higher in younger mothers, corroborating a Center for Disease Control (CDC) report by Colombani (1977) and other studies.17-20 Mothers under 25 years of age had a higher annual incidence of children with gastroschisis, and mothers under 20 years of age presented an even higher annual incidence, which is in line with previous studies.17,18,21 The increased annual incidence of gastroschisis in children of young mothers can be a disease characteristic without a clear cause. However, this increased annual incidence cannot be related to a higher number of teenage pregnancies since several authors, including Ventura, Rasmussen, and Loane, have already demonstrated that the number of pregnant teenagers is decreasing.19,22,23
The analysis of the seven MSs in Rio Grande do Sul showed an initially increasing gastroschisis rate trend in all and a decreasing gastroschisis rate trend in five in the second period. North, Hill, and Valley MSs presented statistically significant changes. It is not possible to explain the causes of the trend variations seen in the observed periods, though similar gastroschisis rate trend variations were reported in several regions of the world by Herrera, Allman, and other authors, probably due to unclear environmental factors.6,7,24 A study on gastroschisis in São Paulo, Brazil, described the prevalence and seasonality changes by suggesting that pesticide exposure could have an influence on these changes.12
In the present study, the mortality of children with gastroschisis was 33%, and almost all (97%) deaths occurred within the first year of life. This mortality rate is in line with a state in a developing country like Brazil, where rates ranging from 14.9% to more than 50% have already been reported by Alves, Bilibio, and other authors.10,25,26 Gastroschisis-related mortality varies widely according to the country in which the study is conducted. In Uganda, the mortality rate, described by Wesonga (2020), was 98%, contrasting with the mortality rate of less than 10%, described by Allman, Anderson, and Lao in the United States of America and by Bradnock in the United Kingdom and Ireland.7,8,18,27,28 The decreased mortality trend was statistically significant in the studied period (Fig. 2).
This study analyzed data from large population databases that represent the studied population very accurately, thus presenting representative annual incidence and mortality rates. The analyzed children with gastroschisis had a higher frequency of low birth weight and prematurity compared with children without gastroschisis. Low weight and gestational age < 37 weeks confirmed an association between intrauterine growth difficulties, prematurity, and gastroschisis, corroborating previous studies by Anderson, Overcash, and others.9,17,18
Unlike a report published by the CDC in 2016 and the description by Anderson, who reported an increased prevalence in relation to race/color, the present study found no statistically significant differences in the analysis of children born with gastroschisis in terms of race/color.17,18,29 In Brazil, it is difficult to analyze race/color due to the great miscegenation of the Brazilian population, and evaluations by race/color can be inaccurate. Analysis by sex showed no statistically significant differences, as reported by Bilibio and other authors.17,25,30
Study limitationsThe study has some limitations, especially concerning the use of secondary data, which is subject to diagnosis coding errors. Another limitation is the fact that children born dead were not counted because they do not appear in the database. However, the results are valid when considering population data, which reduces these errors in the database. Therefore, the limitations are minimized for this sample and type of study.
In conclusion, this study on gastroschisis using population databases from the state of Rio Grande do Sul, shows a tendency to increase the annual incidence of gastroschisis. With an increase of 184% between 2000 and 2010 and a decrease in the period from 2010 to 2017. The annual incidence rate increased 85% in the total period of the study.
The mortality of patients with gastroschisis as the underlying cause was around one-third, in the study period. Almost all children who died were less than a year old. The trend showed a decreased mortality in the study period.
Gastroschisis was confirmed to occur more in children of mothers aged under 25 years. Children with gastroschisis had a higher prematurity rate and presented low birth weight.
Further studies are needed to monitor gastroschisis trends and mortality and to identify the probable etiology and risk factors related to the disease.
Work linked to the Universidade Estadual de Maringá, Centro de Ciências da Saúde, Maringá, PR, Brazil.