Neonatal mortality rate remains high in Brazil. The aim of the study was to evaluate the factors associated with hospitalization during the neonatal period.
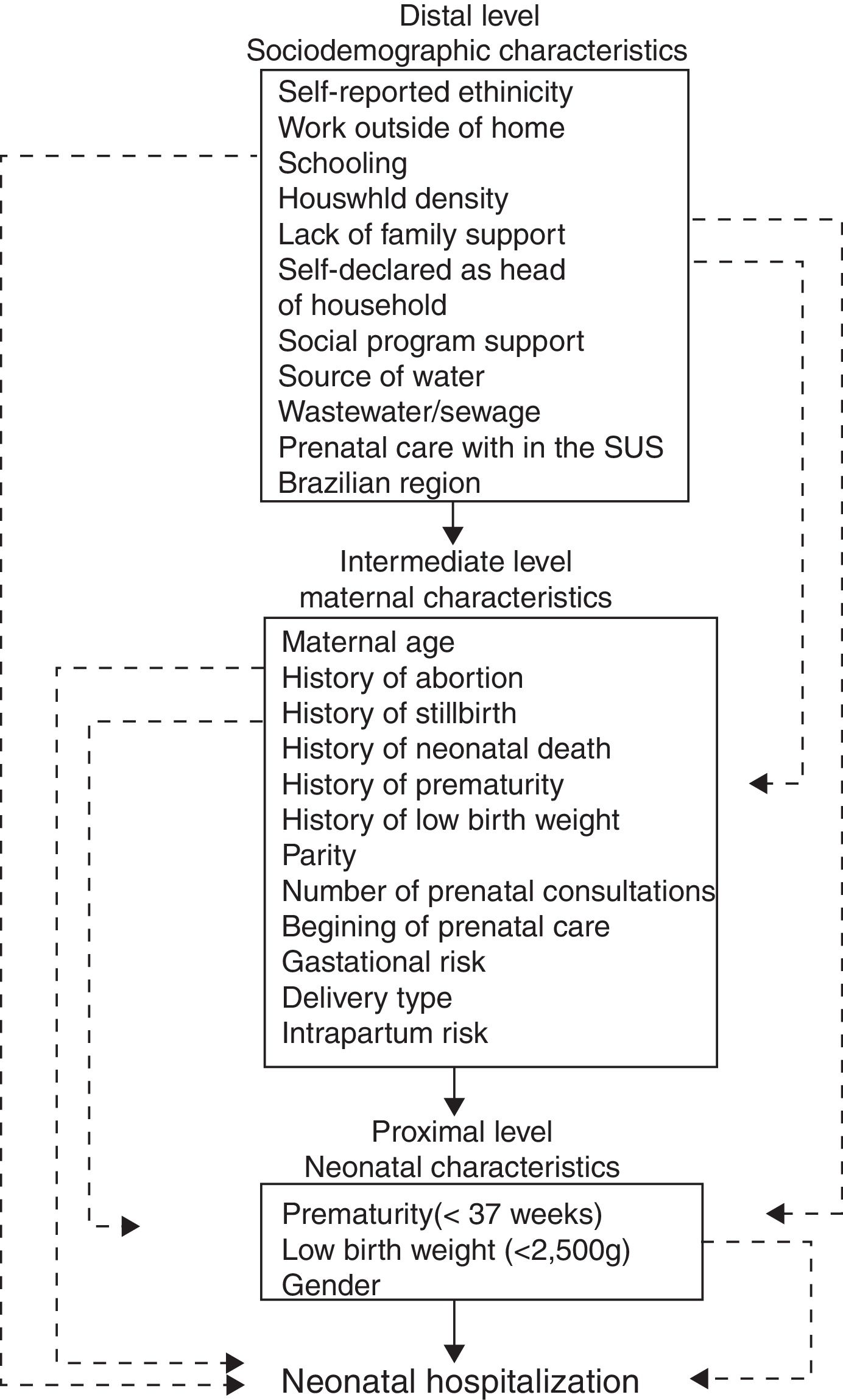
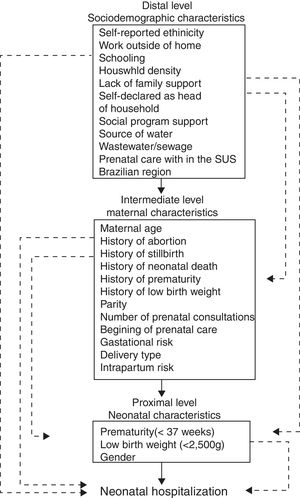
MethodsCross-sectional study conducted in ten randomly-selected Brazilian municipalities. Mothers of children under the age of 6 who were carrying the child's health booklet were interviewed in basic health units. Hierarchical modeling of sociodemographic factors (distal level), maternal variables (intermediate level), and features of the newborns (proximal level) was performed. The variables that presented a value of p≤0.20 in the univariate analysis were included in the multivariate hierarchical modeling process, with block input according to their hierarchical level. The variables with a value of p≤0.05 were considered statistically significant.
Results2022 mothers were included, allowing 258 (12.8%) cases of hospitalization during the neonatal period to be identified, of which 49.7% were male, 8.9% were premature, and 8.4% had low birth weight (<2500g). After analysis by hierarchical approach, factors associated with neonatal hospitalization (prevalence ratio [95% CI]) included: history of prematurity (2.03 [1.25–3.30], p=0.004), gestational risk (2.02 [1.46–2.79], p<0.001); intrapartum risk (3.73 [2.33–5.99], p<0.001); gestational age (32–37 weeks: 13.83 [1.74–110.09], p=0.01; and<32 weeks: 25.03 [3.03–207.12], p=0.003); low birth weight (3.95 [2.56–6.09], p<0.001), and male gender (1.44 [1.09–1.98], p=0.01).
ConclusionFactors associated with maternal and neonatal history are associated with neonatal hospitalization.
A taxa de mortalidade neonatal permanece alta no Brasil. O objetivo do estudo foi avaliar os fatores associados a internação durante o período neonatal.
MétodosEstudo transversal realizado em dez municípios brasileiros aleatoriamente selecionados. As mães das crianças com menos de seis anos de idade que estavam com a caderneta de informações de saúde da criança foram entrevistadas nas unidades básicas de saúde. Foi realizada a modelagem hierárquica dos fatores sociodemográficos (nível distal), das variáveis maternas (nível intermediário) e das características dos recém-nascidos (nível proximal). As variáveis que apresentaram um valor de p ≤ 0,20 na análise univariada foram incluídas no processo multivariado de modelagem hierárquica com entrada em blocos de acordo com seu nível hierárquico. As variáveis com valor de p ≤ 0,05 foram consideradas estatisticamente significativas.
Resultados2022 mães foram incluídas, nos possibilitando identificar 258 (12,8%) casos de internação durante o período neonatal, dos quais 49,7% foram meninos, 8,9% foram prematuros e 8,4% apresentaram baixo peso ao nascer (<2.500g). Após a análise por abordagem hierárquica, os fatores associados a internação neonatal (IP [IC de 95%]) incluíram: histórico de prematuridade (2,03 [1,25-3,30], p=0,004), risco gestacional (2,02 [1,46-2,79], p<0,001); risco intraparto (3,73 [2,33-5,99], p<0,001); idade gestacional (32-37 semanas: 13,83 [1,74-110,09], p=0,01) e (<32 semanas: 25,03 [3,03-207,12], p=0,003); baixo peso ao nascer (3,95 [2,56-6,09], p<0,001) e sexo masculino (1,44 [1,09-1,98], p=0,01).
ConclusãoOs fatores associados a histórico materno e neonatal foram associados a internação neonatal.
Prioritization of children's health is essential for the progress of a population.1–3 Infant mortality reflects the conditions of socioeconomic development, environmental infrastructure, and access to and quality of available resources for maternal and child health care; its reduction is an important health strategy.4 Neonatal mortality, death in the first 28 days of life, accounts for 70% of infant mortality. In Brazil, after social and health policies were implemented, the infant and neonatal mortality rates have decreased in the last decades. However, Brazilian neonatal mortality rates remain very high (8.97 deaths per 1000 live births)5 compared to high-income countries in 2014 (3.94 deaths per 1000 live births in the United States).6 Prematurity and low birth weight are the main factors associated with neonatal mortality.7
Several studies have evaluated factors associated with neonatal mortality8 and prematurity.9 However, few Brazilian studies have evaluated the predictive factors for hospitalization during neonatal period. Factors associated with hospitalization during neonatal period might be similar to those related to neonatal mortality. In addition, understanding the sociodemographic, assistance-related, and biological mother-infant interactions that result in hospitalization during neonatal period may contribute to the identification of strategies to reduce neonatal mortality. The aim of this study was to evaluate the factors associated with hospitalization during neonatal period.
MethodsThis cross-sectional study was conducted in ten municipalities in the five Brazilian macro-regions. Eighty-six Brazilian metropolitan municipalities with at least 5000 live births in 2011 were considered eligible, according to the Information System on Live Births (Sistema de Informação sobre Nascidos Vivos [SINASC]). The study was carried out in randomly selected municipalities and stratified by Brazilian macro-region. Therefore, two municipalities from each macro-region were selected: Santarém and Boa Vista in the North, Campina Grande and Vitória da Conquista in the Northeast, Cuiabá and Anápolis in the Center-West, São Gonçalo and Uberlândia in the Southeast, and Pelotas and Joinville in the South. Previously to data collection, local health authorities were contacted to detail the characteristics of the urban population covered by the basic health units of each selected municipality. Therefore, interviews were carried out in basic health units that contained the largest number of children, aiming at reaching a minimum sample of 150 interviews per municipality. This study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee of IFF/FIOCRUZ, as well as by municipal managers. All mothers signed an informed consent before participating in the study.
Biological mothers of infants up to 6 years of age who had already completed at least one routine visit and were carrying a child health-monitoring tool (health booklet) were interviewed. Questionnaires that did not contain information on hospitalization during neonatal period were excluded from the study. The study estimated a sample size of 1600 mothers to be interviewed, considering a frequency of hospitalization during neonatal period between 10% and 20%, using an α error of 5% with a 95% confidence interval, and an β error of 20%.
The interviews were conducted by means of an electronic questionnaire submitted to previous validation by the IFF/FIOCRUZ pediatric outpatient clinic and in a pilot study conducted in the city of Barueri, SP, Brazil. The field team, which remained in each municipality for six days, was composed of a coordinator, a supervisor, and five senior interviewers, all health professionals. The interviewed mothers were invited to participate in the basic health units while awaiting care for their children, after weighing or vaccination. Hospitalization during neonatal period was defined as length of stay longer than 72h after birth or any hospital re-admission in the first 28 days of life. All pages of the child's health booklet were scanned during the interview. The information provided by the mothers was validated by a single researcher through the revision of the digitized health records.
The proposal of hierarchical modeling for sociodemographic, care, reproductive, and maternal factors of the newborn was recommended, with the purpose of describing the significance of the factors associated with hospitalization during neonatal period that are more proximally controlled by the intermediate and distal factors, respectively. Thus, the variables were divided into different levels (Fig. 1), as described below: distal - sociodemographic level: self-reported ethnicity, prenatal care within the Brazilian public health system, known as Unified Health System (Sistema Único de Saúde [SUS]), family support, mother's schooling, working outside the home, number of inhabitants per domicile, head of household, social support, origin of water, sewage and plumbing, and region of Brazil; intermediate level: maternal age, history of abortion, stillbirth, neonatal death, prematurity and low birth weight, parity, number of prenatal consultations, beginning of prenatal care, gestational risk, type of delivery, intrapartum risk; proximal level - related to the newborn: gestational age (GA), birth weight <2500g, and gender. Gestational risk was defined by presence of condition or health issues that might lead to serious maternal–fetal consequences.10 In addition, intrapartum risk was positive in presence of any high risk condition during delivery, such as bleeding, prolonged labor, low Apgar values, presence of meconium, or neonatal resuscitation, in the absence of gestational risk.
Categorical variables were described as absolute (n) and relative (%) frequencies. Initially, univariate analyzes were performed between the response variable and each explanatory variable, using the prevalence ratio and its 95% confidence interval as a measure of effect. The variables that presented a level of significance with a value of p≤0.20 were maintained in the modeling process. In addition, the degree of multicolinearity was evaluated by the variance inflation factor (VIF), verifying the association of variables.
For the multivariate analysis, a hierarchical approach was used with the block input model, considered a more adequate alternative to estimate the prevalence ratio (PR) in cross-sectional studies with a frequent outcome.11–13 In each hierarchical block, the variables were included in the model one at a time, in decreasing order of degree of association with the response variable, as per the results obtained in the univariate analyzes. In step 1, only the variables from the distal outcome level were introduced. In step 2, the variables of the intermediate level were added, and in step 3, the variables of the proximal level were included. Therefore, the variables of the proximal level were adjusted by the variables of the same block and of the previous hierarchical levels (intermediate and distal). At the end of the inclusion of the variables by blocks, according to the binary logistic regression method with block entry, the final model was determined with the set of those variables that contributed significantly to explain the risk factors for hospitalization during neonatal period. The analyses were performed with the aid of SPSS (IBM SPSS Statistics for Macintosh, version 23.0. NY, USA), and statistical significance was considered with the value of p≤0.05 in bilateral tests.
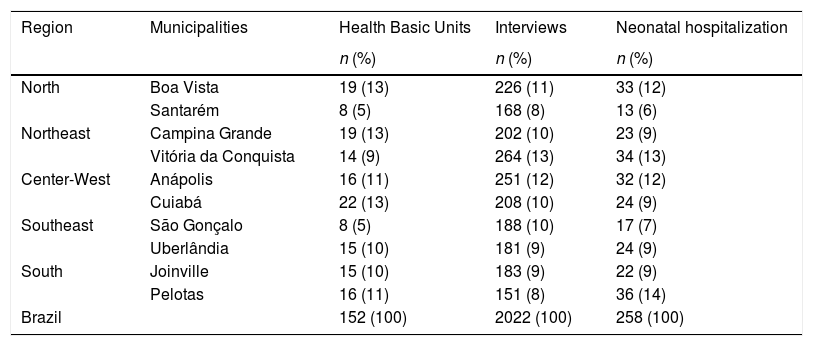
ResultsA total of 2033 interviews were conducted during the study period, of which 11 (0.54%) were excluded due to their lack of information on neonatal hospitalization. Therefore, 2022 interviews were performed in 152 basic health units across the country. Table 1 describes the number of basic health units according to municipalities and macro-regions. This study identified 258 (12.8%) cases of hospitalization during the neonatal period. In the population studied, 65.2% (n=1319) of the mothers interviewed lived in the North, Northeast or Center-West regions. The average age of the mothers interviewed was 27 years (19–39), 20% of mothers were younger than 19 years of age, and 15.2% (n=307) self-defined as of black or indigenous ethnicity. About 90% of mothers had more than four years of schooling, 40% (n=801) considered themselves head of the household, and 70.7% (n=1407) did not work outside the home. A vast majority (89.5%) reported having family support to raise their children and 54.2% declared themselves beneficiaries of an income supplementation program. In addition, 82.4% performed prenatal care within the SUS, 85% had had at least six consultations, and 26% reported facing risk during pregnancy; in 51.3% (n=1035). The delivery was vaginal. In regards to the children, the average age was 20 months (19–21), 49.7% were male; 8.9% were premature (GA<37 weeks); 8.4% were born weighing less than 2500g.
Number (n) and relative frequency (%) of health basic units, interviews, and cases of hospitalization during neonatal period according to Brazilian macro-regions and municipalities.
| Region | Municipalities | Health Basic Units | Interviews | Neonatal hospitalization |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| North | Boa Vista | 19 (13) | 226 (11) | 33 (12) |
| Santarém | 8 (5) | 168 (8) | 13 (6) | |
| Northeast | Campina Grande | 19 (13) | 202 (10) | 23 (9) |
| Vitória da Conquista | 14 (9) | 264 (13) | 34 (13) | |
| Center-West | Anápolis | 16 (11) | 251 (12) | 32 (12) |
| Cuiabá | 22 (13) | 208 (10) | 24 (9) | |
| Southeast | São Gonçalo | 8 (5) | 188 (10) | 17 (7) |
| Uberlândia | 15 (10) | 181 (9) | 24 (9) | |
| South | Joinville | 15 (10) | 183 (9) | 22 (9) |
| Pelotas | 16 (11) | 151 (8) | 36 (14) | |
| Brazil | 152 (100) | 2022 (100) | 258 (100) | |
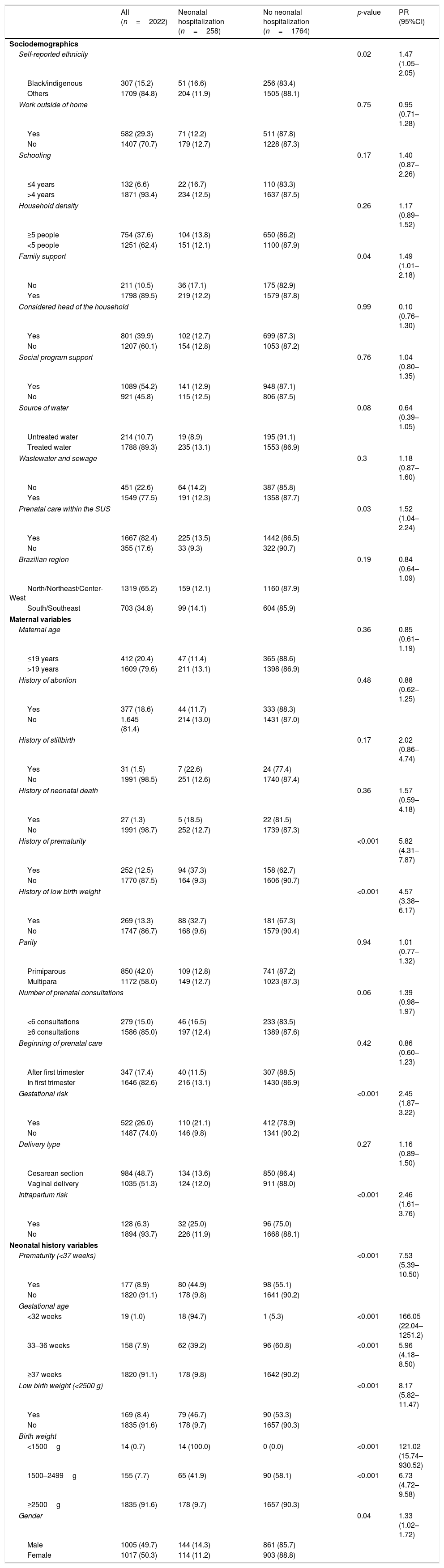
Table 2 shows the results for the univariate analysis of the sociodemographic, maternal reproductive characteristics, and the neonatal history of the child, according to the occurrence of hospitalization during neonatal period. Regarding maternal sociodemographic factors (distal level), black or indigenous ethnicity (p=0.02); maternal schooling below four years (p=0.17); absence of family support (p=0.04), and prenatal care within the SUS (p=0.03) were associated with hospitalization during neonatal period and were included in the hierarchical modeling. Among the maternal reproductive factors (intermediate level), previous history of stillbirth (p=0.17), of prematurity (p<0.001), or of low birth weight (p<0.001) were associated with the outcome. Fewer than six prenatal consultations (p=0.06), presence of gestational risk (p<0.001), and intrapartum risk (p<0.001) were also associated with hospitalization during neonatal period and included in the hierarchical modeling. Finally, factors related to the newborn (proximal level) such as gestational age (p<0.001), low birth weight (p<0.001), and male gender (p=0.04) were associated with hospitalization during neonatal period and included in the hierarchical modeling.
Distribution of sociodemographic, maternal, and neonatal history variables; prevalence ratio (PR) for occurrence of hospitalization during neonatal period.
| All (n=2022) | Neonatal hospitalization (n=258) | No neonatal hospitalization (n=1764) | p-value | PR (95%CI) | |
|---|---|---|---|---|---|
| Sociodemographics | |||||
| Self-reported ethnicity | 0.02 | 1.47 (1.05–2.05) | |||
| Black/indigenous | 307 (15.2) | 51 (16.6) | 256 (83.4) | ||
| Others | 1709 (84.8) | 204 (11.9) | 1505 (88.1) | ||
| Work outside of home | 0.75 | 0.95 (0.71–1.28) | |||
| Yes | 582 (29.3) | 71 (12.2) | 511 (87.8) | ||
| No | 1407 (70.7) | 179 (12.7) | 1228 (87.3) | ||
| Schooling | 0.17 | 1.40 (0.87–2.26) | |||
| ≤4 years | 132 (6.6) | 22 (16.7) | 110 (83.3) | ||
| >4 years | 1871 (93.4) | 234 (12.5) | 1637 (87.5) | ||
| Household density | 0.26 | 1.17 (0.89–1.52) | |||
| ≥5 people | 754 (37.6) | 104 (13.8) | 650 (86.2) | ||
| <5 people | 1251 (62.4) | 151 (12.1) | 1100 (87.9) | ||
| Family support | 0.04 | 1.49 (1.01–2.18) | |||
| No | 211 (10.5) | 36 (17.1) | 175 (82.9) | ||
| Yes | 1798 (89.5) | 219 (12.2) | 1579 (87.8) | ||
| Considered head of the household | 0.99 | 0.10 (0.76–1.30) | |||
| Yes | 801 (39.9) | 102 (12.7) | 699 (87.3) | ||
| No | 1207 (60.1) | 154 (12.8) | 1053 (87.2) | ||
| Social program support | 0.76 | 1.04 (0.80–1.35) | |||
| Yes | 1089 (54.2) | 141 (12.9) | 948 (87.1) | ||
| No | 921 (45.8) | 115 (12.5) | 806 (87.5) | ||
| Source of water | 0.08 | 0.64 (0.39–1.05) | |||
| Untreated water | 214 (10.7) | 19 (8.9) | 195 (91.1) | ||
| Treated water | 1788 (89.3) | 235 (13.1) | 1553 (86.9) | ||
| Wastewater and sewage | 0.3 | 1.18 (0.87–1.60) | |||
| No | 451 (22.6) | 64 (14.2) | 387 (85.8) | ||
| Yes | 1549 (77.5) | 191 (12.3) | 1358 (87.7) | ||
| Prenatal care within the SUS | 0.03 | 1.52 (1.04–2.24) | |||
| Yes | 1667 (82.4) | 225 (13.5) | 1442 (86.5) | ||
| No | 355 (17.6) | 33 (9.3) | 322 (90.7) | ||
| Brazilian region | 0.19 | 0.84 (0.64–1.09) | |||
| North/Northeast/Center-West | 1319 (65.2) | 159 (12.1) | 1160 (87.9) | ||
| South/Southeast | 703 (34.8) | 99 (14.1) | 604 (85.9) | ||
| Maternal variables | |||||
| Maternal age | 0.36 | 0.85 (0.61–1.19) | |||
| ≤19 years | 412 (20.4) | 47 (11.4) | 365 (88.6) | ||
| >19 years | 1609 (79.6) | 211 (13.1) | 1398 (86.9) | ||
| History of abortion | 0.48 | 0.88 (0.62–1.25) | |||
| Yes | 377 (18.6) | 44 (11.7) | 333 (88.3) | ||
| No | 1,645 (81.4) | 214 (13.0) | 1431 (87.0) | ||
| History of stillbirth | 0.17 | 2.02 (0.86–4.74) | |||
| Yes | 31 (1.5) | 7 (22.6) | 24 (77.4) | ||
| No | 1991 (98.5) | 251 (12.6) | 1740 (87.4) | ||
| History of neonatal death | 0.36 | 1.57 (0.59–4.18) | |||
| Yes | 27 (1.3) | 5 (18.5) | 22 (81.5) | ||
| No | 1991 (98.7) | 252 (12.7) | 1739 (87.3) | ||
| History of prematurity | <0.001 | 5.82 (4.31–7.87) | |||
| Yes | 252 (12.5) | 94 (37.3) | 158 (62.7) | ||
| No | 1770 (87.5) | 164 (9.3) | 1606 (90.7) | ||
| History of low birth weight | <0.001 | 4.57 (3.38–6.17) | |||
| Yes | 269 (13.3) | 88 (32.7) | 181 (67.3) | ||
| No | 1747 (86.7) | 168 (9.6) | 1579 (90.4) | ||
| Parity | 0.94 | 1.01 (0.77–1.32) | |||
| Primiparous | 850 (42.0) | 109 (12.8) | 741 (87.2) | ||
| Multipara | 1172 (58.0) | 149 (12.7) | 1023 (87.3) | ||
| Number of prenatal consultations | 0.06 | 1.39 (0.98–1.97) | |||
| <6 consultations | 279 (15.0) | 46 (16.5) | 233 (83.5) | ||
| ≥6 consultations | 1586 (85.0) | 197 (12.4) | 1389 (87.6) | ||
| Beginning of prenatal care | 0.42 | 0.86 (0.60–1.23) | |||
| After first trimester | 347 (17.4) | 40 (11.5) | 307 (88.5) | ||
| In first trimester | 1646 (82.6) | 216 (13.1) | 1430 (86.9) | ||
| Gestational risk | <0.001 | 2.45 (1.87–3.22) | |||
| Yes | 522 (26.0) | 110 (21.1) | 412 (78.9) | ||
| No | 1487 (74.0) | 146 (9.8) | 1341 (90.2) | ||
| Delivery type | 0.27 | 1.16 (0.89–1.50) | |||
| Cesarean section | 984 (48.7) | 134 (13.6) | 850 (86.4) | ||
| Vaginal delivery | 1035 (51.3) | 124 (12.0) | 911 (88.0) | ||
| Intrapartum risk | <0.001 | 2.46 (1.61–3.76) | |||
| Yes | 128 (6.3) | 32 (25.0) | 96 (75.0) | ||
| No | 1894 (93.7) | 226 (11.9) | 1668 (88.1) | ||
| Neonatal history variables | |||||
| Prematurity (<37 weeks) | <0.001 | 7.53 (5.39–10.50) | |||
| Yes | 177 (8.9) | 80 (44.9) | 98 (55.1) | ||
| No | 1820 (91.1) | 178 (9.8) | 1641 (90.2) | ||
| Gestational age | |||||
| <32 weeks | 19 (1.0) | 18 (94.7) | 1 (5.3) | <0.001 | 166.05 (22.04–1251.2) |
| 33–36 weeks | 158 (7.9) | 62 (39.2) | 96 (60.8) | <0.001 | 5.96 (4.18–8.50) |
| ≥37 weeks | 1820 (91.1) | 178 (9.8) | 1642 (90.2) | ||
| Low birth weight (<2500 g) | <0.001 | 8.17 (5.82–11.47) | |||
| Yes | 169 (8.4) | 79 (46.7) | 90 (53.3) | ||
| No | 1835 (91.6) | 178 (9.7) | 1657 (90.3) | ||
| Birth weight | |||||
| <1500g | 14 (0.7) | 14 (100.0) | 0 (0.0) | <0.001 | 121.02 (15.74–930.52) |
| 1500–2499g | 155 (7.7) | 65 (41.9) | 90 (58.1) | <0.001 | 6.73 (4.72–9.58) |
| ≥2500g | 1835 (91.6) | 178 (9.7) | 1657 (90.3) | ||
| Gender | 0.04 | 1.33 (1.02–1.72) | |||
| Male | 1005 (49.7) | 144 (14.3) | 861 (85.7) | ||
| Female | 1017 (50.3) | 114 (11.2) | 903 (88.8) | ||
PR, prevalence ratio; SUS, Unified Health System; LBW, low birth weight. Variables expressed as n (%).
Missing values (n) self-reported ethnicity (6); work outside of home (33); schooling (19); household density (17); family support (13); considered as the head of the family (14); social support (12); source of water (20); wastewater and sewage (22); history of neonatal deaths (4); history of low birth weight (6); number of prenatal consultations (157); beginning of prenatal (29); gestational risk (13); type of delivery (3); prematurity (25); gestational age (25); low birth weight (18); and birth weight (18).
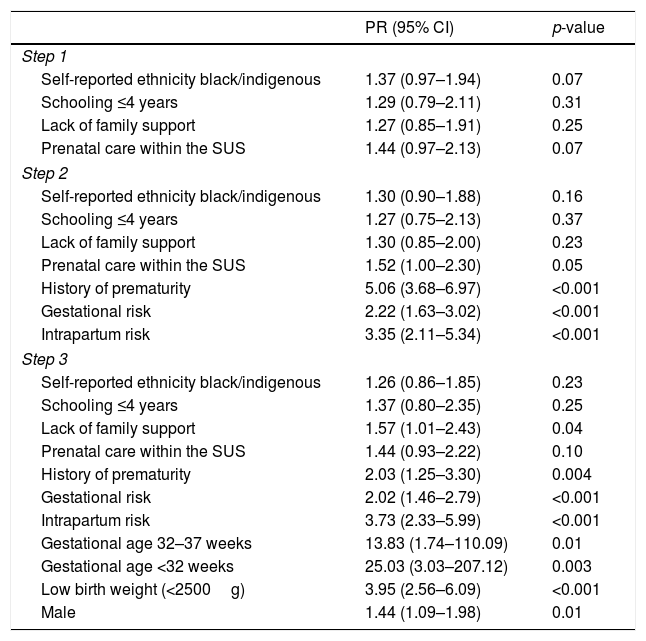
In the first step, the distal determinants were included, and no significant association was observed with hospitalization during neonatal period. Sequentially, the variables of the intermediate level were added to the model, and statistical significance was observed for history of prematurity, gestational risk, and intrapartum risk (p<0.001 for all). Finally, the variables of the proximal hierarchical level, referring to the newborn (block 3), were added to the hierarchical model. The PR (95% CI) of the factors that remained associated with hospitalization during neonatal period in the final hierarchical model were: history of prematurity (2.03 [1.25–3.30], p=0.004), gestational risk (2.02 [1.46–2.79], p<0.001) and intrapartum risk (3.73 [2.33–5.99], p<0.001) at the intermediate level; and gestational age (GA=32–37 weeks: 13.83 [1.74–110.09], p=0.01) and (GA<32 weeks: 25.03 [3.03–207.12], p=0.003), low-birth-weight (3.95 [2.56–6.09], p<0.001), and male gender (1.44 [1.09–1.98], p=0.01) at the proximal level (Table 3).
Final model of factors associated with hospitalization during neonatal period.
| PR (95% CI) | p-value | |
|---|---|---|
| Step 1 | ||
| Self-reported ethnicity black/indigenous | 1.37 (0.97–1.94) | 0.07 |
| Schooling ≤4 years | 1.29 (0.79–2.11) | 0.31 |
| Lack of family support | 1.27 (0.85–1.91) | 0.25 |
| Prenatal care within the SUS | 1.44 (0.97–2.13) | 0.07 |
| Step 2 | ||
| Self-reported ethnicity black/indigenous | 1.30 (0.90–1.88) | 0.16 |
| Schooling ≤4 years | 1.27 (0.75–2.13) | 0.37 |
| Lack of family support | 1.30 (0.85–2.00) | 0.23 |
| Prenatal care within the SUS | 1.52 (1.00–2.30) | 0.05 |
| History of prematurity | 5.06 (3.68–6.97) | <0.001 |
| Gestational risk | 2.22 (1.63–3.02) | <0.001 |
| Intrapartum risk | 3.35 (2.11–5.34) | <0.001 |
| Step 3 | ||
| Self-reported ethnicity black/indigenous | 1.26 (0.86–1.85) | 0.23 |
| Schooling ≤4 years | 1.37 (0.80–2.35) | 0.25 |
| Lack of family support | 1.57 (1.01–2.43) | 0.04 |
| Prenatal care within the SUS | 1.44 (0.93–2.22) | 0.10 |
| History of prematurity | 2.03 (1.25–3.30) | 0.004 |
| Gestational risk | 2.02 (1.46–2.79) | <0.001 |
| Intrapartum risk | 3.73 (2.33–5.99) | <0.001 |
| Gestational age 32–37 weeks | 13.83 (1.74–110.09) | 0.01 |
| Gestational age <32 weeks | 25.03 (3.03–207.12) | 0.003 |
| Low birth weight (<2500g) | 3.95 (2.56–6.09) | <0.001 |
| Male | 1.44 (1.09–1.98) | 0.01 |
SUS, Brazilian Unified Health System.
Factors related to neonatal history and maternal reproductive history were associated with neonatal hospitalization. Although few Brazilian studies have evaluated the factors associated with hospitalization during neonatal period, the analysis of factors related to neonatal death has been described more frequently. In neonatal inpatient surveys, neonatal mortality should be considered, because the factors associated with hospitalization are similar to those associated with neonatal mortality. Most often, the conditions that lead newborns to the hospital are similar to those that can lead to death in the neonatal period.
Neonatal mortality should still be considered a public health problem.14 A national cross-sectional study including more than 20,000 women was conducted to evaluate risk factors associated with neonatal mortality using an hierarchical approach.8 Maternal intercurrences during pregnancy and low birth weight were the main factors associated with neonatal mortality. The present study described similar results in relation to the factors associated with hospitalization during neonatal period, corroborating the presence of the same factors related to mortality and hospitalization during neonatal period. Both studies included data from the five macro-regions of Brazil, and presented similar methodology, with maternal interview and statistical analysis by hierarchical approach at different levels. Some of the characteristics presented by their populations were very similar.8
In Brazil, there is an increase in the incidence of prematurity,8,15 a factor that has been strongly associated with neonatal morbidity and mortality.16 A study by the Brazilian Network of Neonatal Research described that early neonatal mortality occurred within seven days of life in up to 16% of preterm infants with birth weight <1500g.17 Therefore, the evaluation of factors associated with prematurity becomes essential for the estimation of risk factors for hospitalization or mortality. History of prematurity, maternal age extremes, presence of infections, and multiple pregnancies were predictors of prematurity.9 In the present study, the presence of previous history of prematurity doubled the risk of hospitalization during neonatal period (2.03 [1.25–3.30], p=0.004). In addition, prematurity was also associated with hospitalization during neonatal period in the multivariate model (GA of 32–37 weeks: OR=13.83 [1.74–110.09] and GA<32 weeks: 25.03 [3.03–207.12]). In Brazil, the same was observed. Prematurity was associated with neonatal mortality (GA of 33–36 weeks: OR=9.01 [4.74–17.14] and GA≤32 weeks: 200.91 [120.70–334.41]) in the univariate analysis of conditions related to the newborn, but was suppressed from the final hierarchical model.8 In agreement with the influence of prematurity as a predictor for neonatal disease, gestational age<32 weeks was one of the factors included in an indicator of neonatal morbidity “near-miss” constructed by logistic regression models.18
Few studies have evaluated the factors related to hospitalization during neonatal period in Brazil. In 2012, Granzotto et al. analyzed the epidemiological profile of 466 hospitalizations of a historical cohort in an intensive care unit at a university reference hospital, between 2008 and 2010 in Southern Brazil.19 Prematurity (72%) and low birth weight (69%) were the main conditions associated with hospitalization during neonatal period. A cross-sectional, population-based study correlated birth data with neonatal admission records between 2001 and 2011 in New South Wales, Australia's most populous state.20 The authors accessed data from more than 1,000,000 premature and full-term births. The prevalence of neonatal hospitalization was up to ten times higher in newborns with GA<33 weeks when compared to those born at term (97% vs. 9.4%). The risk of hospitalization and duration of hospitalization was inversely proportional to GA. Infants with GA of less than 33 weeks presented a risk of hospitalization ranging from three to six times higher when compared to full-term newborns. The risk of hospitalization associated with prematurity described by Stephens et al. was lower than that reported by the present study. The greater sample size of the Australian study, as well as the higher prevalence of prematurity in Brazil in relation to developed countries, may be explanatory factors for this divergence.8,21
The main strengths of this study were the use of primary data provided by mothers interviewed in randomly selected municipalities in all Brazilian regions. It is acknowledged that the present study might not be considered as a population-based study. This hypothesis was reinforced by the fact that half of mothers interviewed were supported by Bolsa Família, a social program for lower-income families. However, 2022 interviews were performed in 152 basic health units across the country. Table 1 describes the number of basic health units according to municipalities and macro-regions. In addition, 25% more interviews were included than previously calculated in the sample size estimation, and less than 1% of interviews were excluded due to missing data. Others strengths may be the pilot-study performed for investigator training before data collection and the use of a hierarchical approach in the statistical analysis, since the diseases that affect newborns usually involve a large number of variables.22
The potential limitations of this study may be related to data collection by means of maternal interviews and absence of data review in hospital records. The information collected by means of interviews with the mothers may be subject to verification bias, since it is conditioned to maternal understanding and memory. The data on prenatal care, delivery period, related to neonatal history, and reasons for hospitalization during neonatal period may be less robust in this type of study when compared to hospital-based studies, due to being subject to omission of registration. However, the average age of the children at the time of the interview was 20 months, which decreases this time. In turn, memory bias can be minimized by the fact that hospital admission in the first 28 days of the child's life constitutes a significant episode for the mother. Another critical potential in the statistical analysis was the non-inclusion of the number of prenatal consultations in the hierarchy model, since this variable was associated with the outcome evaluated in the univariate analysis. The authors are aware that absence or inadequate prenatal care may be associated with neonatal mortality.23–25 However, the number of observations not available in this variable (n=214) would lead to the exclusion of a large proportion of patients in the multivariate model, thus impairing the analysis. It is acknowledged that a potential selection bias of basic health units might be present, despite the randomly selection of municipalities. However, this bias might be minimized by the fact that the interviews were performed in basic health units that had the largest number of children followed.
In conclusion, the present study found that factors related to the newborn (male gender, prematurity, and low birth weight), as well as those related to maternal reproductive factors (history of prematurity, gestational risk, and intrapartum risk) were associated with hospitalization during the neonatal period. These results corroborate the importance of improving the quality of prenatal care and delivery in order to reduce prematurity and low birth weight.
Conflicts of interestThe authors declare no conflicts of interest.
This study was supported by the National Health Fund (SMS/FNS/MS) under the agreement of the General Coordination of Child Health and Breastfeeding (CGSCAM/DAPES/SAS/MS) with the Fernandes Figueira National Institute for Women's, Children's, and Adolescents’ Health (IFF/FIOCRUZ).
Please cite this article as: Quaresma ME, Almeida AC, Méio MD, Lopes JM, Peixoto MV. Factors associated with hospitalization during neonatal period. J Pediatr (Rio J). 2018;94:390–8.