The prevalence of allergic conjunctivitis (AC) has not been established. Estimates suggest that ocular allergies affect 15% to 20% of the worldwide population, yet most epidemiological studies encompass nasal and ocular allergy symptoms and have not been specific to AC. The aim of this study was to verify the prevalence of ocular allergy symptoms, co-morbidities, and their impact on adolescents.
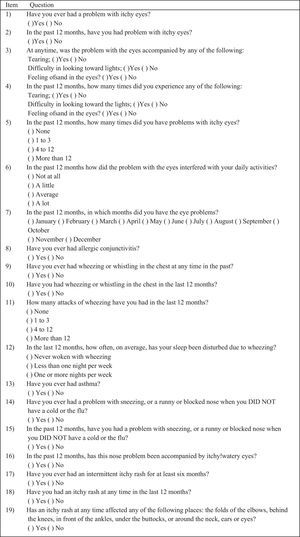
MethodsAdolescents were selected from a sample of schools, and completed in classrooms a previously validated questionnaire on symptoms of AC. AC diagnosis was considered when more than three episodes of ocular itching were reported in the past 12 months. Related symptoms such as tearing, photophobia, foreign body sensation, impact on daily activities, and diagnosis of AC were analyzed.
ResultsQuestionnaires were obtained from 3,120 adolescents (mean age 13.3±1.1 years). Ocular itching in the past 12 months occurred in 1,592 (51%). The most frequently associated symptom was tearing (74%), followed by photophobia (50.1%) and foreign body sensation (37.1%). The prevalence of AC was 20.7%, affecting more females than males (56.1% versus 45.9%; p= 0.01). The risks of an adolescent with ocular allergy to present asthma, rhinitis, and atopic eczema were (OR= 5.7; 95% CI: 4.5 to 7.1), (OR=3.6; 95% CI: 3.0 to 4.3), and (OR=2.6; 95% CI: 2.0 to 3.5), respectively. Severe interference in daily activities was reported by 30.5%.
ConclusionsSymptoms of ocular allergy are common, frequently associated to other allergic diseases, and impact the daily activities of adolescents.
A prevalência de conjuntivite alérgica (CA) não foi estabelecida. Estimativas sugerem que alergias oculares afetam de 15 a 20% da população mundial, ainda que a maioria dos estudos epidemiológicos abranjam sintomas de alergia nasal e ocular e não sejam específicos a respeito da CA. O objetivo deste estudo foi verificar a prevalência de sintomas, comorbidades e o impacto da alergia ocular em adolescentes.
MétodosOs adolescentes foram selecionados de uma amostra de escolas e preencheram, em sala de aula, um questionário previamente validado sobre os sintomas da CA. O seu diagnóstico foi considerado quando mais de três episódios de prurido ocular foram relatados nos últimos 12 meses. Sintomas relacionados, como lacrimejamento, fotofobia, sensação de corpo estranho, impacto sobre as atividades diárias e diagnóstico de conjuntivite alérgica, foram analisados.
ResultadosForam obtidos questionários de 3.120 adolescentes (média de 13,3±1,1 ano). Nos últimos 12 meses, 1.592 (51%) adolescentes tiveram prurido ocular. O sintoma relacionado mais frequente foi lacrimejamento (74%), seguido de fotofobia (50,1%) e sensação de corpo estranho (37,1%). A prevalência de conjuntivite alérgica foi de 20,7%, afetando mais pessoas do sexo feminino do que do masculino (56,1% em comparação a 45,9%; p=0,01). O risco de um adolescente com alergia ocular apresentar asma, rinite e eczema atópico foi (RC=5,7; CI de 95%: 4,5 a 7,1); (RC=3,6; CI de 95%: 3,0 a 4,3) e (RC=2,6; CI de 95%: 2,0 a 3,5), respectivamente. Uma interferência grave nas atividades diárias foi relatada por 30,5%.
ConclusõesSintomas de alergia ocular são comuns, frequentemente relacionados a outras doenças alérgicas, e causam impacto sobre as atividades diárias de adolescentes.
Ocular allergy (OA) is a general term to describe different phenotypes, of which seasonal and perennial allergic conjunctivitis (AC) represent the majority of diagnoses. Severe conditions, such as atopic keratoconjunctivitis and vernal keratoconjunctivitis, affect a smaller number of patients.1
There are few data on OA epidemiology. Allergies are considerably underreported, and incidence has a wide variation depending on geographic location, which interferes with estimates on prevalence of OA. A survey conducted by the American College of Allergy, Asthma, and Immunology found that 35% of families interviewed experienced allergies, of which more than 50% reported associated eye symptoms.2 The importance of OA results mainly from its frequency, which ranges from 5% to 22% of the population.3
Some studies have proposed the concept of ‘one disease’ for asthma and allergic rhinitis. Recent data have also suggested that AC may be part of this entity, based on the fact that most patients suffering from allergic rhinitis also complain of ocular symptoms.4 In contrast, it has been shown that allergic ocular symptoms were the only manifestation of allergy in approximately 25% of allergic adults.5 OA is increasingly recognized as a distinct symptom that imposes its own burden on patient's quality of life.6
In adolescents, most of the epidemiological data, including data from different phases of the International Study on Asthma and Allergies in Childhood (ISAAC), associate ocular symptoms with nasal symptoms, so it is difficult to separate the prevalence of AC from that of allergic rhinitis. This study aimed to determine the OA prevalence and co-morbidities in schoolchildren.
MethodsThis was a cross-sectional study conducted between April and May of 2009 in Curitiba, State of Paraná, Brazil. The survey reached students of seventh and eighth grades to include most of 13 and 14 year olds up to a minimum of 3,000 participants. Information regarding the schools was provided by the Paraná Department of Education. In 2009, there were 253 schools in Curitiba, which were alphabetically ordered and randomized by computer. This sample size has power of 90% to detect differences of 2% in prevalence at 1% significance level. The survey administration techniques followed the ISAAC phase I standardized method.7
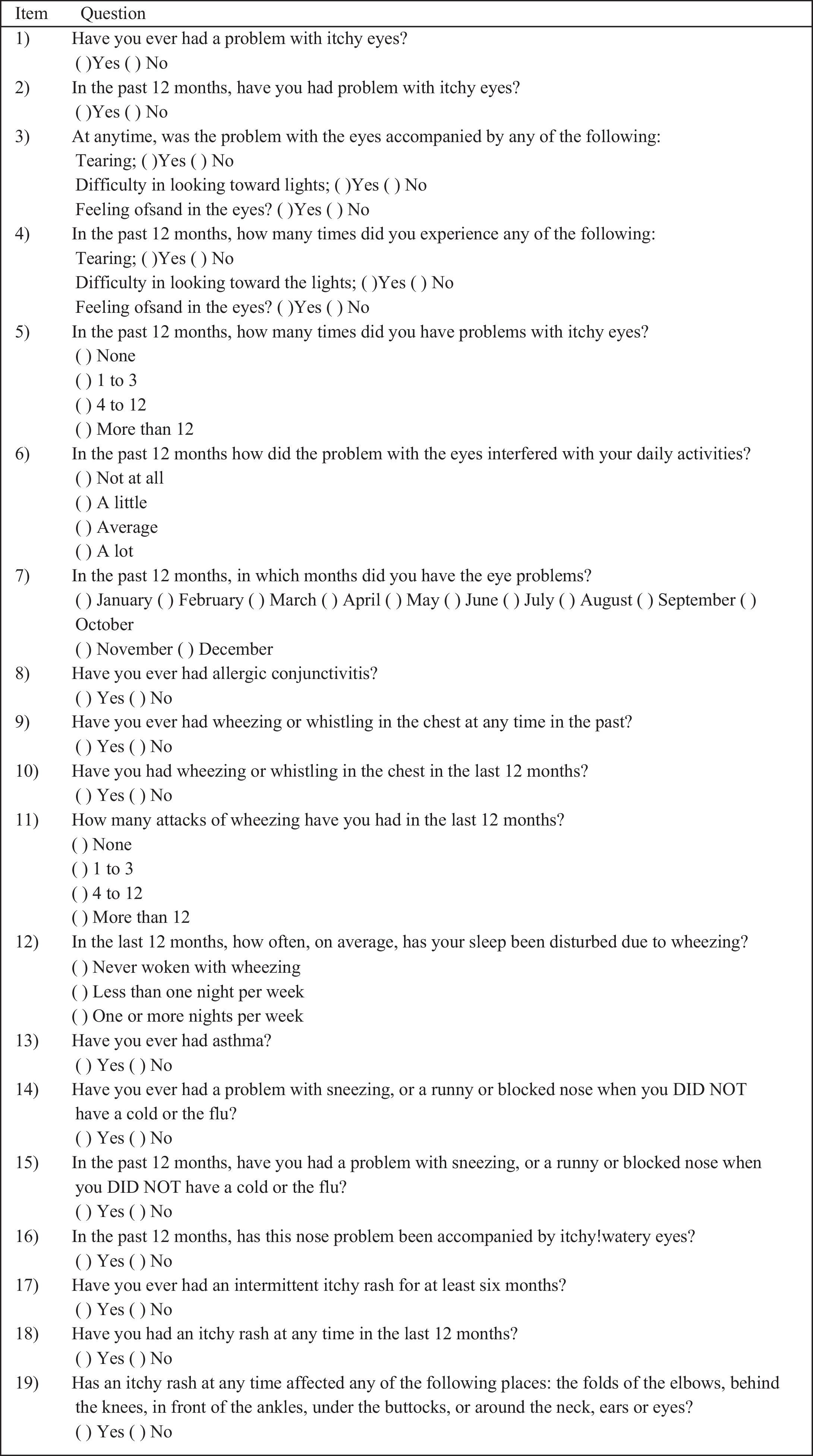
Subjects fulfilled a validated questionnaire from the ISAAC core questionnaire for 13 and 14 year olds, which comprised eight items on OA symptoms (Fig. 1)8 and 11 relevant items on asthma, rhinitis, and atopic eczema symptoms.7
OA was defined as more than three episodes of ocular itching reported in the last 12 months. Subjects with symptoms occurring only between September and December, which is the grass pollen season in the area, were classified as having seasonal symptoms, whereas patients with symptoms occurring both during and apart from the grass pollen season were classified as having perennial symptoms. To investigate the burden of OA, children were asked how much their eye problem had interfered with daily activities in the last 12 months. Those who responded ‘not at all’ or ‘a little’ were classified as ‘mild,’ whereas those responding ‘a moderate amount’ or ‘a lot’ were classified as ‘severe.’
Asthma was considered as positive responses to wheezing in the last 12 months. Frequent asthma symptoms were considered when more than three attacks of wheezing were reported, and severe asthma symptoms when the adolescent had sleep disturbances due to wheezing. Rhinitis was defined when symptoms (sneezing, runny or blocked nose) were present in the absence of cold or the flu. Atopic eczema was considered when a recurrent itchy rash affecting skin folds, for at least six months, had occurred. To reduce errors of recall, only symptoms occurring in the last 12 months were considered.
The statistical package StatCalc-7® was used to analyze the data. The response rate was calculated as the number of completed written questionnaires divided by the number of participants. The proportion of adolescents with allergic symptoms was calculated with a 95% confidence interval (CI). Pearson's chi-squared test was used to compare categorical variables. The significance level was 0.05. The odds ratio (OR) and 95% CI was used to verify the strength of association between OA and the other atopic conditions (asthma, rhinitis, and atopic eczema). The study was approved by the institutional review board, and informed consent was obtained from all participants.
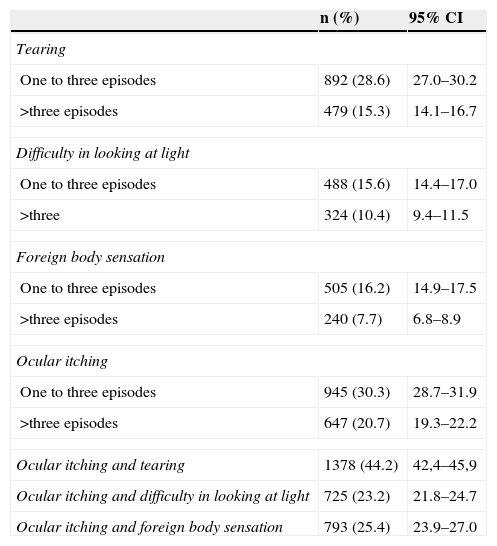
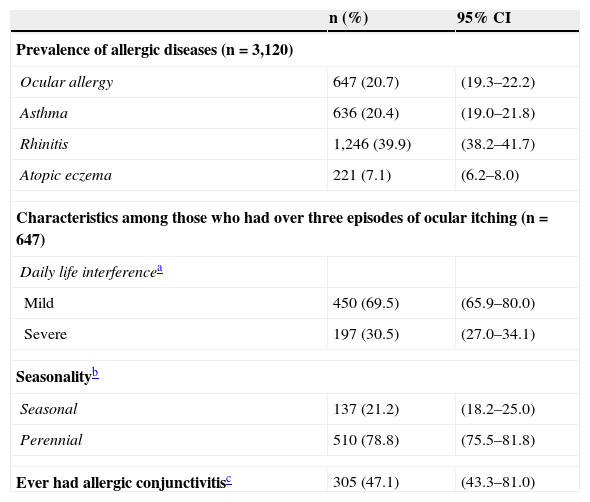
ResultsThere were 3,468 subjects approached; 68 did not consent and 280 did not complete the questionnaire correctly. There were 3,120 adolescents included; the response rate was 91.8% (51.2% females). The age varied between 12 and 18 years old (mean 13.3±1.1 years old). The prevalence of symptoms of OA was 20.7% (Table 1). Among those considered as having OA, 30.5% had severe symptoms (79% were perennial), and 47% reported a previous diagnosis of AC (Table 2).
Prevalence of ocular allergy symptoms in adolescents (n=3,120).
| n (%) | 95% CI | |
|---|---|---|
| Tearing | ||
| One to three episodes | 892 (28.6) | 27.0–30.2 |
| >three episodes | 479 (15.3) | 14.1–16.7 |
| Difficulty in looking at light | ||
| One to three episodes | 488 (15.6) | 14.4–17.0 |
| >three | 324 (10.4) | 9.4–11.5 |
| Foreign body sensation | ||
| One to three episodes | 505 (16.2) | 14.9–17.5 |
| >three episodes | 240 (7.7) | 6.8–8.9 |
| Ocular itching | ||
| One to three episodes | 945 (30.3) | 28.7–31.9 |
| >three episodes | 647 (20.7) | 19.3–22.2 |
| Ocular itching and tearing | 1378 (44.2) | 42,4–45,9 |
| Ocular itching and difficulty in looking at light | 725 (23.2) | 21.8–24.7 |
| Ocular itching and foreign body sensation | 793 (25.4) | 23.9–27.0 |
CI, confidence interval.
Prevalence of allergic diseases and characteristics among those who had over three episodes of ocular itching.
| n (%) | 95% CI | |
|---|---|---|
| Prevalence of allergic diseases (n=3,120) | ||
| Ocular allergy | 647 (20.7) | (19.3–22.2) |
| Asthma | 636 (20.4) | (19.0–21.8) |
| Rhinitis | 1,246 (39.9) | (38.2–41.7) |
| Atopic eczema | 221 (7.1) | (6.2–8.0) |
| Characteristics among those who had over three episodes of ocular itching (n=647) | ||
| Daily life interferencea | ||
| Mild | 450 (69.5) | (65.9–80.0) |
| Severe | 197 (30.5) | (27.0–34.1) |
| Seasonalityb | ||
| Seasonal | 137 (21.2) | (18.2–25.0) |
| Perennial | 510 (78.8) | (75.5–81.8) |
| Ever had allergic conjunctivitisc | 305 (47.1) | (43.3–81.0) |
CI, confidence interval.
Mild symptoms in the past 12 months: if they responded ‘not at all’ or ‘a little’ for daily life interference; severe symptoms: if they responded ‘a moderate amount’ or ‘a lot’.
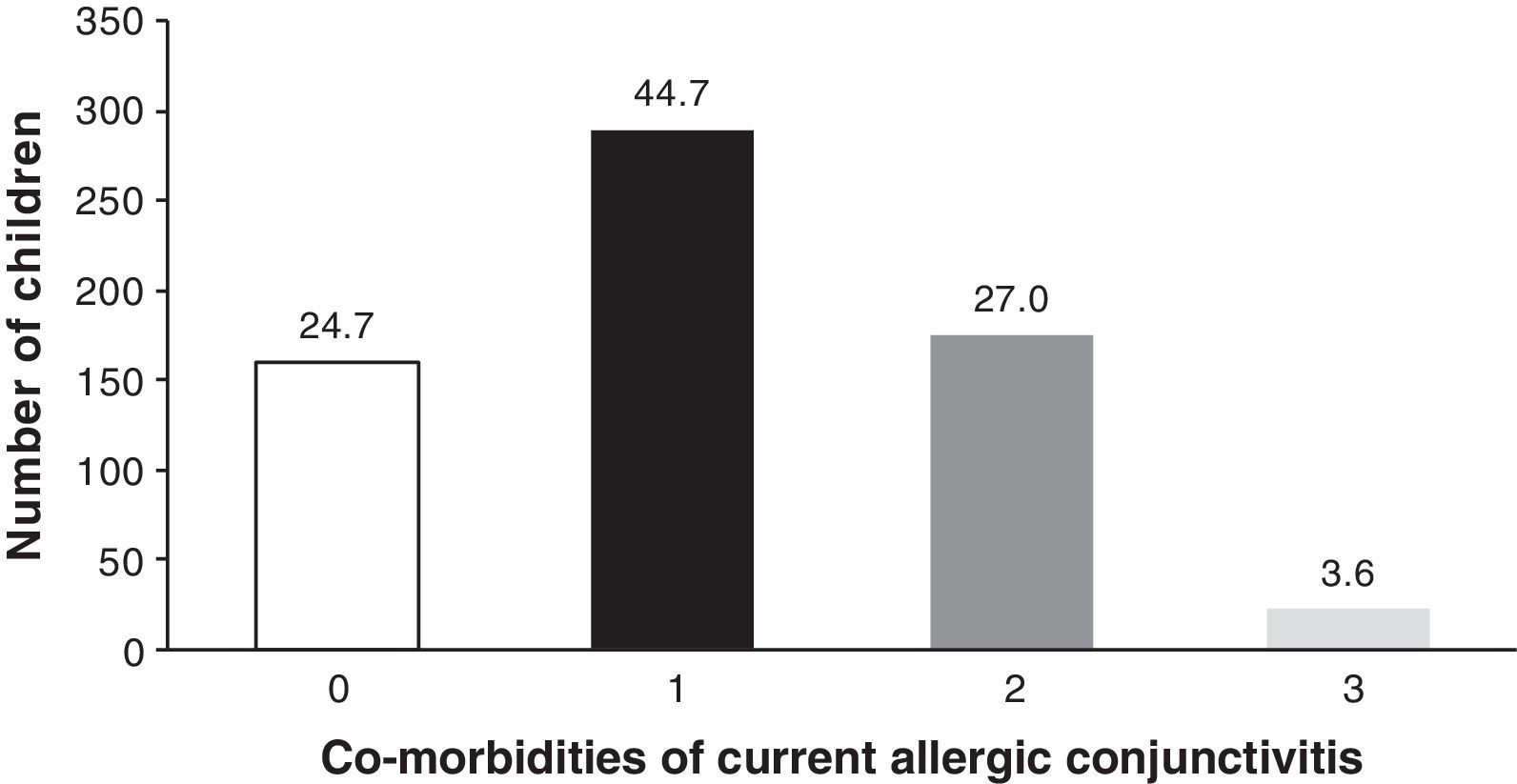
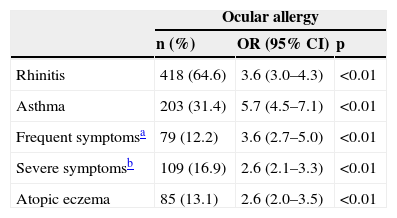
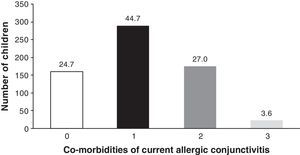
OA-related co-morbidities are shown in Table 3. At least one co-morbidity (asthma, rhinitis, or atopic eczema) was reported by 75.3% of children with OA. Rhinitis was the most frequent co-morbidity (64.6%). Asthma occurred in 31.4% and atopic eczema in 13.1%. The number of children with none, one, two or three allergy-related co-morbidities is shown in Fig. 2. Co-morbidities of perennial versus seasonal OA compared through the chi-squared test showed that rhinitis was more common in those with perennial symptoms (66.7% versus 56.9%; p=0.034), whereas asthma and atopic eczema did not differ between the two groups (33.1% versus 24.8%; p=0.062) and (12.3% versus 16%; p=0.25), respectively. Daily life interference was greater in those with perennial symptoms (22.7% versus 13.1%; p<0.01).
Co-morbidities of ocular allergy in children (n=647).
| Ocular allergy | |||
|---|---|---|---|
| n (%) | OR (95% CI) | p | |
| Rhinitis | 418 (64.6) | 3.6 (3.0–4.3) | <0.01 |
| Asthma | 203 (31.4) | 5.7 (4.5–7.1) | <0.01 |
| Frequent symptomsa | 79 (12.2) | 3.6 (2.7–5.0) | <0.01 |
| Severe symptomsb | 109 (16.9) | 2.6 (2.1–3.3) | <0.01 |
| Atopic eczema | 85 (13.1) | 2.6 (2.0–3.5) | <0.01 |
CI, confidence interval; OR, odds ratio.
The probability of an adolescent with OA to show asthma, rhinitis, and atopic eczema was (OR=5.7; 95% CI: 4.5 to 7.1); (OR=3.6; 95% CI: 3.0 to 4.3) and (OR=2.6; 95% CI: 2.0 to 3.5), respectively. The association between asthma and OA was greater among those with both OA and rhinitis than those with OA only (36.8% versus 20.5%; p<0.01).
DiscussionWritten questionnaires have been widely used in epidemiological studies of allergic diseases. The prevalence of asthma, rhinoconjunctivitis, and atopic eczema have been verified and compared throughout the globe. However, OA symptoms are less studied, and most of epidemiological studies have evaluated eyes and nasal symptoms combined, so it is difficult to analyze the prevalence of OA and its relationship with other allergic diseases.
There are few validated questionnaires to study OA. In a case-control study involving 102 subjects, more than three episodes of ocular itching in the last 12 months was predictive of OA with sensitivity of 85.4% and specificity of 85.1%.8 Although not pathognomonic, recurrent ocular itching is the most frequent symptom of OA9 and it is the first symptom observed in allergen conjunctival challenge.10 Patients with blepharitis, eczema, keratoconjunctivitis sicca, and other types of conjunctivitis may occasionally present with ocular itching.11
The questionnaire was designed specifically to assess prevalence of OA symptoms, and a high response rate was obtained.8 Ocular itching was identified in 51% of participants. The prevalence of OA was 20.7%, considering the criterion of more than three episodes of ocular itching in the last 12 months. In the US, ocular itching and tearing were identified in 40% of 20,010 participants in the National Health and Nutrition Examination Survey.5 In Sweden, response to a written questionnaire followed by a subsequent interview of 396 schoolchildren aged 12 to 13 years estimated the cumulative prevalence of AC of 19.1%,12 while in Turkey the overall prevalence of AC in children 6-14 years was 7.1%.13 In Karachi, Pakistan, 818 children aged between 5 and 19 years underwent vision assessment and slit lamp examination by an ophthalmologist. Diagnosis of AC was confirmed in 19.2%, considering the presence of papillae in the upper tarsal conjunctiva, redness of the eyes, and history of itching and burning.14
The prevalence of OA has a wide variation between geographic areas not only due to genetic differences and environmental factors, but also due to the lack of standardization in the assessment of ocular symptoms by validated methods. The ISAAC phase III comprised 304,679 adolescents aged 13-14 years from 56 countries, and demonstrated that the prevalence of nasal symptoms associated with itchy watery eyes ranged from 4.5% to 45.1% among adolescents.15 In the ISAAC, there were no questions regarding isolated AC symptoms, and the opportunity to verify its prevalence was missed. If validated questions for ocular symptoms had been included, the identification of the prevalence of AC and its relationship with other allergic diseases could have been facilitated.16
In this study, lacrimation was associated in 73.9% of adolescents with OA. After exposure of the ocular surface to allergens, there is a late phase reaction with cell infiltrate that could lead to obstruction of the nasolacrimal duct. Tearing caused by neuronal reflex has also been observed after nasal provocation tests17.
‘Difficulty in looking at light’ was reported by 45.7% of OA participants. It is important to distinguish this symptom from photophobia, which when detected, suggests alternative diagnosis as iritis and uveitis.18 Foreign body sensation occurs when there is a break in the corneal epithelium, exposing sensitive corneal nerves to the opening and closing of the eyelids.19 This symptom was reported by 20% of those with OA.
Conjunctival hyperemia is a common symptom of OA, but it is nonspecific. In recent years, an increase in the prevalence of red eye has occurred due to an increase in the use of contact lenses and exposure to irritants such as tobacco smoke and pollutants.20
Seasonal AC (SAC) and perennial AC (PAC) are the most prevalent types of OA. SAC is reported to be more common than PAC in temperate climate countries.11 However, in tropical climates, perennial symptoms appear to be more common. A study from Thailand with 445 patients with AC has showed that 81.8% had PAC. Most of them were sensitized to Dermatophagoides pteronyssinus (Dp) (70.2%) and house dust (67.5%).21 In this study, 78.8% of subjects with OA had perennial symptoms. In addition, when symptoms were perennial there was a stronger association with rhinitis and greater impact in daily life activities compared with seasonal symptoms. In 1999, a study to evaluate atopic sensitization in this population demonstrated that skin sensitization to Dp and Lolium multiflorum (Lm) in 3,271 13 to 14 year-old schoolchildren was 31.3% and 4.7%, respectively. Whereas in 3,041 adults, positive skin prick test was 38.9% to Dp and 15.4% to Lm.22 These findings suggest that perennial allergens are important triggering agents in this population.
Approximately one fifth of the students with OA reported that ocular symptoms caused moderate or severe interference in daily activities, though more specific questions related to quality of life have not been included in this evaluation. In rhinitis, studies have shown that this question was well correlated with other indicators of morbidity, including reported symptom severity, interference with specific activities of daily living, and medical service use.7 In the Allergies in America Survey, 23% of AR patients found red, itchy eyes to be extremely bothersome and 20% said the same for watery eyes.23 Ten percent of patients surveyed believed that red, itchy eyes were their most bothersome symptom.
Despite the high prevalence of OA and important morbidity it imposes, the disease is often under-diagnosed. Half of the subjects considered as having OA answered ‘yes’ to the question ‘Have you had AC?’, suggesting that OA is under-recognized. It is known that OA symptoms may not become severe enough to lead patients to visit their doctors. A study performed in Portugal with 220 patients with AC demonstrated that, although significant impairment of quality of life had been observed during acute episodes of OA, only 19.4% had an appointment with an ophthalmologist as a first action and 37.2% had previous allergic evaluation.24
OA is also under-recognized by physicians. In a review of medical records of 1,549 asthmatic patients from a tertiary referral hospital, 681 (44%) had at least one ocular symptom suggestive of OA. However AC was diagnosed only in 16% by the attending physician.25
It is common to face associations between allergic conditions. However, few studies have evaluated OA comorbidities. In the present study, OA was often associated with at least one allergic condition. Rhinitis was the most common, followed by asthma and atopic eczema. Rhinoconjunctivitis has been identified as a risk factor for asthma. The prevalence rate of RCA between asthmatics may be as high as 90%.26 For individuals studied in Curitiba, the odds ratios of an adolescent with OA to have asthma, rhinitis, and atopic eczema were six, four, and three times, respectively. The association between asthma and OA was greater among those with both OA and rhinitis. It is not known why the combination of symptoms varies among allergic patients. In a birth cohort study with 404 unselected 6-year-old children, it was suggested that the link between allergic disorders tends to be stronger in those with IgE-mediated reaction.27
The present study has provided information of isolated OA epidemiology. From the public health perspective, it is important to diagnose, treat, and evaluate comorbidities of patients with OA, since this disease is highly prevalent and frequently associated with other allergic diseases. Assessing risk factors and the allergic status of these patients should be the focus of future epidemiological studies on AC.
FundingUniversidade Federal do Paraná.
Conflicts of interestThe authors declare no conflicts of interest.
The authors are grateful to the following medical students, participants of the GEA Study Group: Bruna Bozelli Leopoldino, Cristine Secco Rosário, Fernanda Barkema, Fernanada Gasparin Palermo, Giseli Macedo, Larissa Dalla Costa Kusano, Natalia Oliveira de Eiras, Renata Robl, Ricardo Parolin Schnekenber, Thieri Drage Costa, and Vitor Guimarães de Macedo. They also would like to thank Dr. Elizabeth Maria Mercer Mourão for her valuable contributions, the school's directors, and participating students and their parents.
Please cite this article as: Geraldini M, Neto HJ, Riedi CA, Rosário NA. Epidemiology of ocular allergy and co-morbidities in adolescents. J Pediatr (Rio J). 2013;89:354–60.