To assess speech alterations in mouth-breathing children, and to correlate them with the respiratory type, etiology, gender, and age.
MethodA total of 439 mouth-breathers were evaluated, aged between 4 and 12 years. The presence of speech alterations in children older than 5 years was considered delayed speech development. The observed alterations were tongue interposition (TI), frontal lisp (FL), articulatory disorders (AD), sound omissions (SO), and lateral lisp (LL). The etiology of mouth breathing, gender, age, respiratory type, and speech disorders were correlated.
ResultsSpeech alterations were diagnosed in 31.2% of patients, unrelated to the respiratory type: oral or mixed. Increased frequency of articulatory disorders and more than one speech disorder were observed in males. TI was observed in 53.3% patients, followed by AD in 26.3%, and by FL in 21.9%. The co-occurrence of two or more speech alterations was observed in 24.8% of the children.
ConclusionMouth breathing can affect speech development, socialization, and school performance. Early detection of mouth breathing is essential to prevent and minimize its negative effects on the overall development of individuals.
Verificar alterações na fala em crianças respiradoras orais e relacioná-las com o tipo respiratório, a etiologia, o gênero e a idade.
MétodoForam avaliados 439 respiradores orais com idade entre quatro e 12 anos. Considerou-se atraso no desenvolvimento de fala a presença de alterações em crianças acima de cinco anos de idade. As alterações observadas foram interposição de língua (IL), ceceio frontal (CF), troca articulatória (TA), omissões (OM) e ceceio lateral (CL). Relacionou-se etiologia da respiração oral, gênero, idade, tipo respiratório e alterações de fala.
ResultadosAlterações de fala foram diagnosticadas em 31,2% dos pacientes sem relação com o tipo respiratório: oral ou misto. Maior frequência de trocas articulatórias e mais de uma alteração de fala ocorreram no gênero masculino. IL foi documentada em 53,3% pacientes, seguida por TA em 26,3% e CF em 21,9%. Concomitância de duas ou mais alterações de fala ocorreu em 24,8% das crianças.
ConclusãoRespirar pela boca pode afetar o desenvolvimento da fala, a socialização e o desempenho escolar. A detecção precoce da respiração oral é essencial para prevenir e minimizar seus efeitos negativos sobre o desenvolvimento global dos indivíduos.
Nasal breathing improves the quality of the inspired air, protects the airways, and promotes correct positioning of the phono-articulatory organs, ensuring good performance of the stomatognathic functions.1,2
Mouth breathing, a pathological condition,3 may be due to upper airway obstruction, sagging facial muscles, or habit;1 any individual who has exhibited this type of breathing for a minimum of six months should be considered a mouth breather.4 Genetic factors and exposure to obstructive factors, regardless of etiology, can be detrimental to child development.
Among the consequences of mouth breathing are alterations in cranio-orofacial growth, speech, nutrition, body posture, sleep quality, and school performance.1 Overall, the mouth breather presents alterations in posture, tone, and mobility of lips, tongue and cheeks, resulting in less efficiency in stomatognathic functions: chewing, swallowing and speech, flaccid jaw elevator muscles, anterior head posture, maxillary atresia, and speech disorders.5,6
Speech can be altered due to flaccid facial muscles, incorrect positioning of the tongue,7 or structural problems of the oral cavity caused by malocclusion and/or deficiencies in facial growth and development.2,8
The most commonly described speech disorders in mouth breathers are: anterior position of tongue during production of lingual dental phonemes,9 imprecision in bilabial (/p/,/b/,/m/) and fricative (/f/,/v/,/s/,/z/,/¿/,/∫/) phonemes in Portuguese, frontal lisp (FL), and lateral (LL) lisp.10–12 Children who are mouth-breathers can also have daytime sleepiness,13,14 poor brain oxygenation,15 or immature auditory processing. All of these complications can lead to learning disabilities.16
Thus, the aims of this study were to assess the development of speech, the most frequently observed speech alterations, and to correlate them with the etiology of mouth breathing The knowledge of these aspects can help health professionals to prevent or minimize the consequences of mouth breathing.
MethodsMouth-breathing children (n=439) aged 4 to 12 years, enrolled in and regularly attending the Mouth-breather Center (Centro do Respirador Bucal – CRB) of the Universidade Federal de São Paulo/Escola Paulista de Medicina (UNIFESP-EPM) from May of 2000 to May of 2011, were evaluated. Patients with genetic syndromes, orofacial malformations, or mental retardation were excluded.
Patients were evaluated according to standards established by the CRB. First, patients were evaluated by the otorhinolaryngology specialist and then, by the other specialists of the CRB: allergist, physical therapis, dentist, orthodontist, and speech therapist, always on the same day.
Patients with a history of mouth breathing for at least six months, with nasal obstruction, pallid or hyperemic nasal mucosa, with or without hypertrophy of adenoid (volume occupying less than 70% of airway) and tonsils (grade I or II), and nonobstructive nasal septal deviation/turbinate (Brozek et al.5), conditions observed by the otorhinolaryngology specialist during clinical examination and nasal fibroscopy, were included.
The allergic etiology in patients with a clinical diagnosis of rhinitis (runny nose, sneezing, itchy nose and/or eye) was confirmed by reports of clinical exposure, onset/worsening of symptoms, and immediate hypersensitivity skin test positive to aeroallergens (D. pteronyssinus, D. farinae, Blomia tropicalis, Penicillium notatum, Aspergillus fumigatus, Alternaria alternata, Periplaneta americana, Blattella germanica, dog epithelium, cat epithelium; positive [histamine, 10mg/mL] and negative controls [saline]; IPI – ASAC do Brasil). Patients were considered allergic when they showed mean induced wheal diameter to at least one of the allergens tested ≥ 3mm.17
Once mouth breathing and its etiology were confirmed, according to the protocol, the orthodontist, during clinical assessment and analysis of orthodontic documentation, assessed the presence/absence of occlusion alterations. The dentist assessed the status of the teeth, the oral and perioral mucosa, and gums.
Patients were classified according to the etiology of oral breathing as: atopy (A) - patients without hypertrophy of adenoids and/or pharyngeal tonsils, but with allergy symptoms (nasal itching, rhinorrhea, nasal obstruction, sneezing) and positive immediate hypersensitivity skin test (IHST); hypertrophy of adenoids and/or pharyngeal tonsils (H) - patients with obstruction due to hypertrophy without allergic symptoms and negative IHST; atopy associated with hypertrophy (A+H) - patients with obstruction due to hypertrophy, allergic symptoms, and positive IHST; or functional (F) - mouth=breather with no hypertrophy, no symptoms of allergic rhinitis, and negative IHST.
The speech therapy assessment evaluated the respiratory mode by direct observation during consultation, and with the use of a Glatzel mirror. Patients were classified as oral (the patient had nasal flow restriction and remained with his/her mouth open during the evaluation session) or oro-nasal (patient ventilated through both nostrils with parted lips). The speech therapist also performed the clinical evaluation of tone and mobility of the phono-articulatory organs and stomatognathic functions, among them, speech. The speech evaluation was performed by spontaneous conversation and picture naming in an articulatory album, made with several pictures covering all the phonemes of the Portuguese language in three distinct positions: beginning, middle, and end of the word.18–20
Anamnesis data such as development of feeding (time of breastfeeding, evolution of food consistency, eating solid foods), stimulation level (educational level of parents and early school life), and history of ear infections during the child's development were not considered in this research as not enough parents/caregivers could provide this information.
The diagnosis of speech considered age and physiological development. The presence of alterations in children older than five years was considered delayed speech development.
In these cases, the observed alterations were classified as: tongue interposition (TI) before the utterance of/t/,/d/,/n/, and/l/; frontal lisp (FL), the interposition of the anterior tongue in the utterance of/s/and/z/; sound omissions (SO); articulatory disorders (AD), characterized by exchanging one sound for another, systematically or not; and lateral lisp (LL), the lateral interposition of the tongue, resulting in the distortion of the sounds/∫/and/¿/.21 The existence of several concomitant speech disorders was also verified.
The chi-squared test or Fisher's test were used for the analysis of the variables, establishing 5% as the rejection level for the null hypothesis. This study was approved by the Research Ethics Committee of the Hospital São Paulo and UNIFESP-EPM (No. 1,428/07).
ResultsOf the 439 children evaluated, 137 were older than five years and had speech disorders. Of these, 64 were females and 73 males, divided into age groups: 37.2% were aged between 5 and 6 years, 30.7% between 7 and 8 years old, 19% between 9 and 10 years, and 13.1% between 11 and 12 years. The type of breathing in patients with speech disorders was oro-nasal in 44.5% and oral in 55.5%. The etiological cause of nasal obstruction was defined as follows: A in 35.8% of patients, H in 21.2%, A+H in 33.6%, and and F in 9.5%.
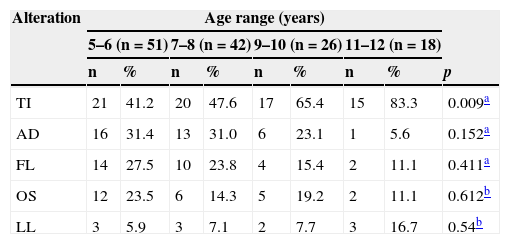
The most frequently observed speech disorders were TI in 53.3% of patients, AD in 26.3%, FL in 21.9%, SO in 18.2%, and LL in 8%. The age groups differed in relation to TI, with a significantly higher number in the age ranges >9 years.
There was no significant association between the type of breathing)oral or oro-nasal) and speech disorders; however, AD was significantly higher in male patients. Table 1 shows the lack of association between speech disorders and etiology of oral breathing.
Distribution of speech problems according to age groups.
| Alteration | Age range (years) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5–6 (n=51) | 7–8 (n=42) | 9–10 (n=26) | 11–12 (n=18) | ||||||
| n | % | n | % | n | % | n | % | p | |
| TI | 21 | 41.2 | 20 | 47.6 | 17 | 65.4 | 15 | 83.3 | 0.009a |
| AD | 16 | 31.4 | 13 | 31.0 | 6 | 23.1 | 1 | 5.6 | 0.152a |
| FL | 14 | 27.5 | 10 | 23.8 | 4 | 15.4 | 2 | 11.1 | 0.411a |
| OS | 12 | 23.5 | 6 | 14.3 | 5 | 19.2 | 2 | 11.1 | 0.612b |
| LL | 3 | 5.9 | 3 | 7.1 | 2 | 7.7 | 3 | 16.7 | 0.54b |
AD, articulatory disorders; FL, frontal lisp; LL, lateral lisp; SO, sound omissions TI, tongue interposition.
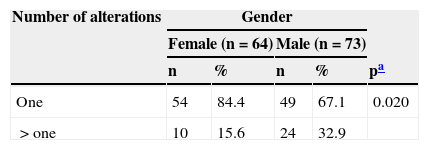
When analyzing the presence of more than one speech disorder according to age group, there was no significant difference between the ages. When associating gender and presence of more than one speech disorder, as shown in Table 2, it was observed that male children had a significantly higher percentage of cases with more than one alteration.
Presence of speech problems in children according to gender.
| Number of alterations | Gender | ||||
|---|---|---|---|---|---|
| Female (n=64) | Male (n=73) | ||||
| n | % | n | % | pa | |
| One | 54 | 84.4 | 49 | 67.1 | 0.020 |
| >one | 10 | 15.6 | 24 | 32.9 | |
When speech is the aim of a study, it is difficult to encompass all aspects that may affect the outcome. Type of breathing, together with time of history, the severity of allergy, and frequency of crises; hypertrophy of pharyngeal tonsils and/or adenoid and the degree of hypertrophy; development of eating habits and the duration, frequency, and intensity of harmful habits; facial profile, strength and mobility of the facial muscles; development of hearing, auditory condition at the time of testing, and auditory processing; dental occlusion and craniofacial growth; and even the level of stimulation received during development should all be considered as so that the study's results are more comprehensive.
Although several studies have reported that mouth breathers can have speech disorders,1,2,11 and that FL and LL are frequent in this population,10 the lack of more detailed accounts describing this possible association,12 prompted the performance of this study, even considering the limitations caused by the diversity of interfering factors in speech development.
As patients from a referral service were evaluated, it was observed that the A etiology (alone or combined) was the most common among the patients, similar to what was previously observed by other investigators.2,22,23
Although delays in language and/or speech can occur three times more often in boys than in girls, according Vitto & Feres,24 the present study, when correlating speech and gender, demonstrated differences only in AD, for which males showed a significantly higher percentage.
Dissimilarly, FL and LL were not the most frequent alterations.10 It was initially believed that FL would be more frequent in cases of tonsil hypertrophy, since by occupying more space in the back of the oral cavity, they would cause projection of the tongue, and thus the FL. The present data did not confirm this assumption, as although FL was more frequent in the A+H etiology, it was not for the H etiology.
Among all the aspects studied, it is noteworthy that 31.2% of patients evaluated were children with speech disorders who were older than five years, an age when the phonological system must be fully developed,25 suggesting that mouth breathing may be an interfering factor in its development. However, dental occlusion, which was not considered in the present study, may have an important association with speech disorders, as observed by Farronato et al.26 The presence of Angle class III malocclusion, diastema, increased overjet, and presence of open bite or deep bite tend to be associated with speech disorders.
Aspects related to the development of eating habits in these patients or the history of harmful habits were not considered in the study; these factors can affect facial muscles and hinder the utterance of correct phonemes. According to Thomas et al.,27 the time of breastfeeding alone does not appear to be directly related to malocclusions, but can aggravate dental-facial problems when associated with parafunctional habits.
Despite the limitations of the present study, it is believed the data obtained are of utmost importance, especially when considering that, in general, speech disorders were more frequent between 5 and 8 years of age, with 24.8% of children concomitantly showing more than one alteration. This demonstrates that speech intelligibility may be impaired at an age range (5–8 years) during which the interaction with peers is important for development and when promptness to learn how to read and write is being established. Therefore, mouth breathers, in addition to the risk of delayed speech development, can have difficulties in socialization and at school, regarding literacy and its subsequent process.28
Studies have demonstrated a close relationship between mouth breathing and learning disabilities, and attention and memory deficits.15,16,29,30 However, there have been no reports of studies correlating alterations in breathing and learning difficulties of individuals with delayed speech development.
The auditory aspect should be considered in this circumstance, as it can interfere with the perception of sounds of language, making the acquisition and/or correction of speech and writing difficult. In the first years of school, the pronunciation of words directly influences the learning of reading and writing, to the point of affecting their acquisition and development.
The mouth breather is vulnerable to ear infections from both palatine tonsils and/or pharyngeal hyperplasias, as well as swelling of the nasal mucosa in allergic cases, which may lead to malfunction of the Eustachian tube and fluctuating hearing loss.31 This can interfere with the capacity to identify speech sounds during development, causing delays and alterations.
The structural and functional consequences of mouth breathing are know to often be spontaneously irreversible, thus its early detection is crucial for the implementation of a multidisciplinary approach towards treatment.
The present findings suggest that monitoring the development of mouth breathers is essential, aiming at improving quality of life and minimizing the negative effects of mouth breathing. Among the various professionals, the speech therapist can greatly contribute to the quality of life of these patients by working on the development of language and speech, stomatognathic functions, and assisting in the development of reading and writing.
Conflicts of interestThe authors declare no conflicts of interest.