to review the literature for clinical data on infants with allergic or eosinophilic colitis.
Data sourceMEDLINE search of all indexes was performed using the words “colitis or proctocolitis and eosinophilic” or “colitis or proctocolitis and allergic” between 1966 and February of 2013. All articles that described patients’ characteristics were selected.
Data synthesisa total of 770 articles were identified, of which 32 met the inclusion criteria. The 32 articles included a total of 314 infants. According to the available information, 61.6% of infants were male and 78.6% were younger than 6 months. Of the 314 patients, 49.0% were fed exclusively breast milk, 44.2% received cow's milk protein, and 6.8% received soy protein. Diarrheal stools were described in 28.3% of patients. Eosinophilia was found in 43.8% (115/263) of infants. Colonic or rectal biopsy showed infiltration by eosinophils (between 5 and 25 per high-power field) in 89.3% (236/264) of patients. Most patients showed improvement with the removal of the protein in cow's milk from their diet or the mother's diet. Allergy challenge tests with cow's milk protein were cited by 12 of the 32 articles (66 patients).
Conclusionseosinophilic colitis occurs predominantly in the first six months of life and in males. Allergy to cow's milk was considered the main cause of eosinophilic colitis. Exclusion of cow's milk from the diet of the lactating mother or from the infant's diet is generally an effective therapeutic measure.
revisão da literatura sobre dados clínicos de lactentes com colite eosinofílica ou alérgica.
Fonte dos dadospesquisa no Medline de todas as indexações com as palavras “colitis or proctocolitis and eosinophilic” ou “colitis or proctocolitis and allergic” entre 1966 e fevereiro de 2013. Foram selecionados todos os artigos que descreviam as características dos pacientes.
Síntese dos dadosforam identificados 770 artigos dos quais 32 preenchiam os critérios de inclusão. Os 32 artigos incluíram o total de 314 lactentes. Conforme as informações disponíveis, 61,6% dos lactentes eram do sexo masculino e 78,6% apresentavam idade inferior a 6 meses. Dos 314 pacientes, 49,0% encontrava-se em aleitamento natural exclusivo, 44,2% recebiam proteína do leite de vaca e 6,8% proteína da soja. Fezes diarreicas foram descritas em 28,3% dos pacientes. Eosinofilia foi encontrada em 43,8% (115/263) dos lactentes. Biópsia retal ou colônica mostrou infiltração por eosinófilos (entre 5 e 25 por campo de grande aumento) em 89,3% (236/264) dos pacientes. A maioria dos pacientes apresentou melhora com a retirada da proteína do leite de vaca da sua dieta ou das suas mães. Teste de desencadeamento com proteína do leite de vaca foi citado em 12 dos 32 artigos (66 pacientes).
Conclusõescolite eosinofílica ocorre predominantemente nos primeiros seis meses de vida e no sexo masculino. Alergia ao leite de vaca foi considerada a principal causa de colite eosinofílica. Dieta de exclusão do leite de vaca da mãe lactante ou da dieta do lactente é uma medida terapêutica geralmente eficaz.
The prevalence of food allergy has increased in recent decades, especially in the pediatric population.1,2 Foods most often related to food allergy are cow's milk, eggs, soy, peanuts, nuts, seafood, and kiwifruit.2 In infants, cow's milk protein allergy (CMA) is the most common, and usually starts in the first six months of life.
In Brazil, the prevalence of food allergy and the most important types of food allergy are yet to be determined. A study performed in the five geographic regions of Brazil assessed the sensitization of children with atopy, demonstrating that the most sensitizing food allergens were fish, eggs, cow's milk, wheat, peanuts, soybeans, and corn.3 Among infants, the food that most frequently caused sensitization was cow's milk.3 It is noteworthy that the presence of sensitization does not mean that the individual will effectively have food allergy.
Based on information from other countries, CMA is the most common type of food allergy in childhood.4 It affects approximately 3% of children,5 and its prevalence is higher in the first year of life. An epidemiological study performed in pediatric gastroenterology clinics in several regions of Brazil showed that among 9,478 consultations, 7.3% were prompted by a known or suspected food allergy, and the following were the suspected foods: 77% of cases, cow's milk; 8.7% of cases, soy; 2.7% of cases, egg; and 11.6% of cases, other foods. The analysis of new cases and follow-up allowed for a good estimation of an incidence of 2.2% and prevalence of 5.4% of patients with confirmed or suspected CMA.6
CMA should be regarded as an important clinical entity, since that normal infants have high rates of growth and development, and both CMA and the use of inadequate diet substitutes can compromise full growth and development in this important phase of life.6,7
Eosinophilic or allergic colitis has been described as a common entity,5,8 but its exact prevalence is unknown.4 Walker-Smith, one of the pioneers in the study of gastrointestinal food allergy, stated that, since the last decade CMA has been occurring with different manifestations when compared to those observed in the 1970s and 1980s, when there was a predominance of enteropathy induced by the milk in the infants’ diet with infections by enteropathogenic Escherichia coli.9 In this context, the epidemiological study performed in Brazil6 demonstrated that 20.6% of infants with known or suspected CMA had blood in the stool that might be the result of allergic or eosinophilic colitis.
Eosinophilic colitis is considered one of the presentations of primary gastrointestinal eosinophilic diseases. This group of diseases also includes eosinophilic esophagitis, eosinophilic gastritis, and eosinophilic gastroenteropathy. The differential diagnosis of eosinophilic diseases must include causes that may result in secondary eosinophilic infiltration, such as certain intestinal parasites (Enterobius vermicularis, Strongyloides stercoralis, and Trichuris trichiura) and drugs (carbamazepine, rifampicin, gold, non-steroidal anti-inflammatory drugs, and tacrolimus).10,11 It is also noteworthy that the clinical picture depends on the predominance of eosinophilic infiltration in the different layers of the intestine, that is, mucosal, muscularis, and serosa layers. There is a high association with atopy at all ages; however, in infants, the connection with food allergy is more frequently established.
Conversely, in adults, in addition to the adverse reaction to foods, other mechanisms lead the treatment to often include medicines in addition to elimination diet. Thus, the term allergic colitis can be used as a second alternative to denominate eosinophilic colitis, in a more appropriate form for infants.10,11
Thus, considering the increase in the number of infants with bleeding in the stool associated with CMA and the lack of articles with large samples, a literature review of articles indexed from 1966 to February of 2013 was performed, focusing on clinical and evolution aspects of infants with eosinophilic or allergic colitis.
MethodsA search was performed in the MEDLINE database for all indexed articles containing the words “colitis or proctocolitis and eosinophilic” and “colitis or proctocolitis and allergic”, between 1966 and February of 2013. Publications were considered in the following languages: English, Portuguese, and Spanish. All types of articles were included, as long as they contained the clinical information of the infants with colitis or eosinophilic or allergic proctocolitis.
The abstracts were independently analyzed by two authors who selected articles that had samples or case reports of infants (younger than 24 months) whether or not they presented with a clinical picture of elimination of blood in diarrheal stool attributed to colitis or allergic or eosinophilic proctocolitis.
Articles whose abstracts were insufficient to define inclusion or exclusion were read in full. In case of disagreements among the researchers regarding the inclusion of a certain article, information was reassessed until consensus was achieved.
Regarding the selected articles, the following data were evaluated: age and gender of the infant, clinical picture and diet at diagnosis, tests, prescribed treatment, and allergy challenge test was performed.
ResultsA total of 770 articles were identified in the initial search, of which 32 were selected according to the predefined inclusion criteria, evaluating 314 infants.11–42
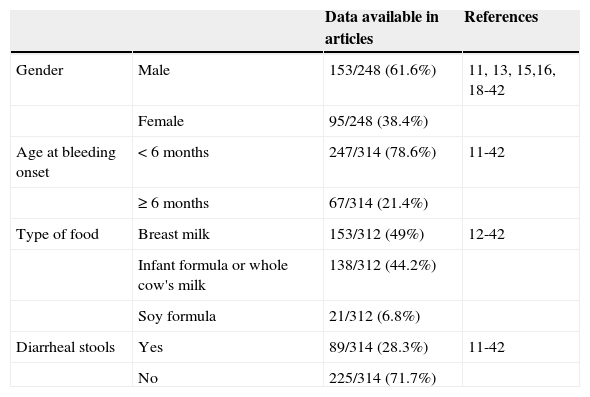
According to data shown in Table 1, of the 314 infants, most were male and younger than 6 months. Diarrheal stools were described in 28.3% of patients.
Demographic and clinical data on allergic or eosinophilic colitis according to the review of published articles.
| Data available in articles | References | ||
|---|---|---|---|
| Gender | Male | 153/248 (61.6%) | 11, 13, 15,16, 18-42 |
| Female | 95/248 (38.4%) | ||
| Age at bleeding onset | < 6 months | 247/314 (78.6%) | 11-42 |
| ≥ 6 months | 67/314 (21.4%) | ||
| Type of food | Breast milk | 153/312 (49%) | 12-42 |
| Infant formula or whole cow's milk | 138/312 (44.2%) | ||
| Soy formula | 21/312 (6.8%) | ||
| Diarrheal stools | Yes | 89/314 (28.3%) | 11-42 |
| No | 225/314 (71.7%) |
Regarding diet at diagnosis, 153 infants (49%) were exclusively breastfed, and the remaining received cow's milk protein (44.2%), except for 21 infants (6.8%) who received soy-based formula.
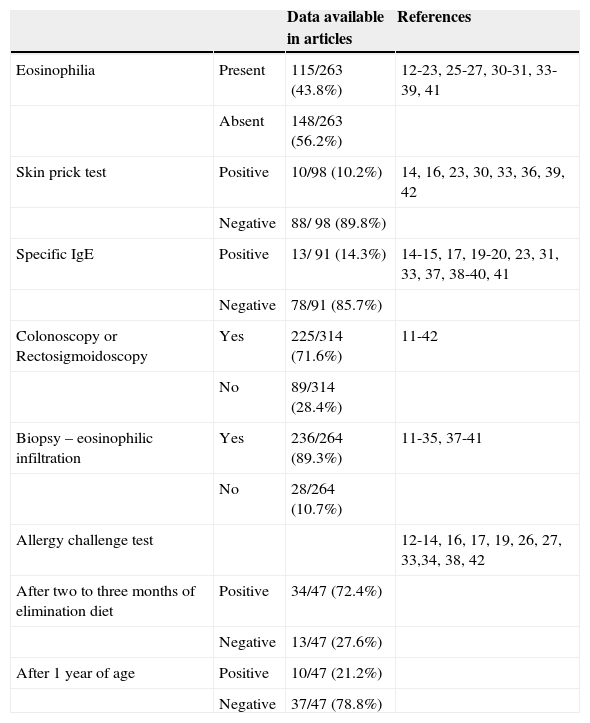
Regarding complementary tests, eosinophilia was found in 43.8% (115/263) of infants (Table 2). Sensitization to cow's milk was assessed by skin prick test in 98 patients, and was positive in 10 (10.2%) infants. Specific IgE against cow's milk protein was tested in 91 patients, and was positive in 13 (14.3%).
Additional tests used for the diagnosis of eosinophilic or allergic colitis according to the literature review.
| Data available in articles | References | ||
|---|---|---|---|
| Eosinophilia | Present | 115/263 (43.8%) | 12-23, 25-27, 30-31, 33-39, 41 |
| Absent | 148/263 (56.2%) | ||
| Skin prick test | Positive | 10/98 (10.2%) | 14, 16, 23, 30, 33, 36, 39, 42 |
| Negative | 88/ 98 (89.8%) | ||
| Specific IgE | Positive | 13/ 91 (14.3%) | 14-15, 17, 19-20, 23, 31, 33, 37, 38-40, 41 |
| Negative | 78/91 (85.7%) | ||
| Colonoscopy or Rectosigmoidoscopy | Yes | 225/314 (71.6%) | 11-42 |
| No | 89/314 (28.4%) | ||
| Biopsy – eosinophilic infiltration | Yes | 236/264 (89.3%) | 11-35, 37-41 |
| No | 28/264 (10.7%) | ||
| Allergy challenge test | 12-14, 16, 17, 19, 26, 27, 33,34, 38, 42 | ||
| After two to three months of elimination diet | Positive | 34/47 (72.4%) | |
| Negative | 13/47 (27.6%) | ||
| After 1 year of age | Positive | 10/47 (21.2%) | |
| Negative | 37/47 (78.8%) |
Of the 314 patients, 225 (71.6%) underwent colonoscopy or rectosigmoidoscopy, which showed areas of friability and erosive lesions of the mucosa. In addition to these patients, 39 underwent rectal biopsy without endoscopic procedure. Thus, biopsies were performed in 264 patients showing eosinophil infiltration (between 5 and 25 per high-power field) in 236 (89.3%) patients. Other histopathological findings were foci of erythema, chronic inflammatory infiltrate with areas of activity (lymphocytes, plasma cells, eosinophils), and signs of degeneration and regeneration of epithelial cells.
Cow's milk protein was removed from the diet of the mother and/or of the infant in most cases, with disappearance of intestinal bleeding.
Allergy challenge tests with cow's milk protein were mentioned in 12 of 32 articles, and were performed in 66 patients. Of these, 47 tests were performed two to three months after diagnosis and start of the elimination diet, and were positive in 34 (72.4%) patients, while 47 other tests were performed after one year of age, and were positive in only 10 (21.2%) patients.
DiscussionEosinophilic or allergic colitis is a frequent manifestation of CMA in infants, occurring predominantly in males and usually starting in the first six months of life. According to the literature, approximately half of the cases occur during exclusive breastfeeding. Treatment consists of the exclusion of cow's milk proteins from the diet of the lactating mother and/or infant.
The first description of eosinophilic colitis was made by Kaijser in 1937.43 Allergic proctocolitis was described by Rubin in 1940 and subsequently by Grybosky in the 1960s. They manifest as inflammatory changes of the colon and rectum, secondary to immune reactions triggered by ingestion of food proteins.44
Its exact prevalence is unknown. Arvola et al., in 2006, evaluated the cause of rectal bleeding in 40 infants and found an association with CMA through allergy challenge test in 18% of cases.33 This result differs from the data retrieved by the present literature search, which demonstrated that most patients experienced recovery when submitted to elimination diet excluding cow's milk and dairy products (Table 2). However, it is important to observe that only a small percentage of the articles analyzed mentioned the use of the allergy challenge test to confirm the diagnosis of CMA. According to the data compiled in this article, 72.4% of allergy challenge tests were positive when performed up to two to three months of the elimination diet onset.
Eosinophilic colitis can occur since the neonatal period. In the present review, six reports of eosinophilic colitis in the first week of life were retrieved.13,25,31,35,39,41
The main clinical manifestation of the disease is the presence of blood in stool, whether or not associated with diarrheal stools.44,45 In general, the infant presents no weight loss, impairment of general health status, or changes at abdominal palpation.5,43 In all descriptions compiled in this article, the clinical manifestation of blood in the stool was reported in all patients, while diarrhea was reported in only 28.3% of cases.
Several foods have been associated with the development of eosinophilic colitis, but most cases are associated with cow's milk protein.44 About 50% of cases occur in children on exclusive breastfeeding.5,44,45 Kilshaw and Cant demonstrated that the presence of β-lactoglobulin can be detected in most samples of breast milk from mothers who consume cow's milk.46 In the present review, 49% of the described patients were exclusively breastfed. Most articles mention that the process is controlled when the proteins in cow's milk are excluded from the lactating mother's diet. Especially in recent years, studies have identified a subgroup of infants with eosinophilic colitis in the presence of exclusive breastfeeding that did not improve with the exclusion of cow's milk proteins from their mothers’ diet.37,39,47
Patients with this characteristic have been attended to at this service; however, no data are available on the proportion of infants with eosinophilic colitis during exclusive breastfeeding who do not improve after the exclusion of cow's milk from their mothers’ diet.47 A conducted in Hungary evaluated 34 infants on exclusive breastfeeding with blood in stool caused by eosinophilic colitis. Of the 34 patients, ten had persistent hematochezia when their mothers eliminated cow's milk and egg proteins from their diet. After confirming the diagnosis by colonoscopy and biopsy, breast milk was discontinued and replaced by an amino acid formula. All ten patients improved and showed no recurrence during the 13-month minimum follow-up.37
In this circumstance, two hypotheses can be raised: (1) persistence of small amounts of cow's milk proteins in the maternal diet despite the recommendation of elimination diet, considering that it is very difficult for the lactating mother to effectively remove cow's milk proteins from their diet; (2) Allergy to other foods present in the mother's diet that are transported through breast milk, thus raising the suspicion of eosinophilic colitis by multiple food allergies. In this context, a preliminary study performed in Italy39 evaluated 14 infants with allergic colitis that did not improve after their mothers started having a hypoallergenic diet (free of cow's milk, soy, and egg). The authors performed a skin prick test, specific IgE measurement, and patch test.
All foods tested by the skin prick test and IgE were negative. Conversely, the patch test was positive with their own mother's milk in all cases, with cow's milk in 50% of cases, with soy in 28%, with egg in 21%, with rice in 14%, and with wheat in 7%. Thus, it can be deduced that other foods that were not investigated and that are transported through breast milk could also be responsible for the process of eosinophilic colitis. The results of this article should be interpreted with caution, given the small number of patients and the lack of comparison groups consisting of children with eosinophilic colitis responsive to elimination diet carried out by the mother and another group with normal infants. The main objective of the Academy of Breastfeeding Medicine is to develop protocols for the treatment of diseases that may compromise the success of breastfeeding. Allergic proctocolitis was the subject of one of these protocols.
For cases that did not improve with the exclusion of cow's milk from the mother's diet, the exclusion of other foods (soy, citrus, eggs, peanuts, wheat, corn, strawberries and chocolate) is recommended. They emphasize that such a diet can only be carried out with the supervision of a dietician experienced in the area, to ensure the mother's diet meets her basic nutritional and lactation needs. It recognizes that an infant with more severe eosinophilic colitis that does not respond to an elimination diet conducted by the mother should be fed exclusively on formula adequate for the treatment of CMA.47 In general, when the allergen is excluded from the mother's diet, the bleeding disappears within 72 to 96hours, with a maximum waiting period of two weeks.9,47
The diagnosis of eosinophilic colitis caused by CMA should be established based on history and thorough physical examination.5,45 It is important to exclude the differential diagnosis of rectal bleeding, such as infections, necrotizing enterocolitis, intestinal intussusception, and anal fissure.5,44
To date, there are no non-invasive tests to confirm the diagnosis. Eosinophilia can be found in approximately 50% of patients with allergic colitis. The skin prick test and measurement of specific IgE against cow's milk can show negative results in infants, as identified in the present review. In turn, the patch test was evaluated in a few studies and, due to the lack of result standardization, it is not recommended to date.9,45
The diagnostic confirmation is based on the favorable clinical response by the patient after the start of the allergen elimination diet (cow's milk) and recurrence of bleeding with the reintroduction (allergy challenge test) of cow's milk protein in the diet.5,44,45 The allergy challenge test is considered the most reliable method for the diagnosis of food allergy.9 It can be performed in three different ways: non-blind (open), single-blind, and double-blind placebo-controlled test.9 The two blinded modalities should be used when the clinical manifestations are subjective. In the case of infants, the non-blind allergy challenge test is traditionally recommended.9,45
It is noteworthy that only 12 of the 32 articles analyzed in this review sought to confirm the diagnosis with an allergy challenge test. 78.8% of the patients who were submitted to the allergy challenge test after 12 months of age showed negative result, indicating the development of tolerance. Conversely, when the allergy challenge test was performed two to three months after the start of the elimination diet, the diagnosis was confirmed in 72.4% of patients. Thus, when tested, the diagnosis of CMA is confirmed early in most patients, whereas after 12 months, the development of tolerance to cow's milk proteins is usually observed.
Many authors do not use the allergy challenge test to diagnose food allergy, which is the reason for the large discrepancy in reported prevalence and incidence of food allergy. A cohort study that followed 480 children from birth to 3 years of age showed that 28% of parents thought that their children's symptoms could be due to food allergy, especially in the first year of life. Conversely, when the allergy challenge test was performed, the diagnosis was confirmed in only 8% of cases. This result shows the importance of completing the allergy challenge test in the diagnosis of food allergy, avoiding unnecessary costs and maintenance of an elimination diet.48
Additionally, the possibility of tolerance development during the interval between the diagnosis and the allergy challenge test cannot be ruled out. In this context, it should be noted that, since the 1990s, the European Society of Pediatric Gastroenterology and Nutrition has considered the non-blind allergy challenge test appropriate for infants, in view of the fact that at this age range the suggestion component induced by the test is virtually nonexistent.9,49 It should be noted that allergy challenge tests should not be performed if there is risk of anaphylaxis. It is currently recommended to start the test in a hospital environment.9,45
The diagnostic workup can be performed by invasive procedures such as sigmoidoscopy and colonoscopy, always associated with local biopsies.
The most common findings are extensive involvement of the rectum and colon mucosa with areas of erosion interspersed with those of normal mucosa. Lymphoid nodular hyperplasia can also be observed. The characteristic histological analysis of food allergy discloses signs of inflammation and eosinophil infiltration in the intestinal mucosa and lamina propria. Although there are controversies, the presence of more than 20 eosinophils per high-power field is generally considered indicative of eosinophilic infiltration. The indication of these procedures should be made considering the clinical characteristics of each particular case.44,45
The treatment of eosinophilic colitis consists in the exclusion of the allergen from the diet (cow's milk protein), constituting the “elimination diet”. In the case of infant formula, which uses cow's milk as basis, its substitution by a formula containing extensively hydrolyzed protein should be recommended.9 Patients who have not responded well to these should receive free amino acid formula.9 In cases of exclusive breastfeeding, the mother's diet should exclude cow's milk and dairy foods, and breastfeeding should be maintained.9,45
In conclusion, CMA should be considered the main cause of eosinophilic colitis. Tests to assess sensitization to cow's milk do not contribute to establish the diagnosis. Despite the heterogeneity in diagnostic criteria, the infiltration of the rectal mucosa with eosinophils is reported in most biopsies. Exclusion of cow's milk and dairy products from the diet of the mother or infant is an effective therapeutic measure. Allergy challenge test confirmed the diagnosis of CMA in most patients when performed a few weeks after recovery attained through the elimination diet, while tolerance to cow's milk was characterized in most cases with eosinophilic colitis after 12 months of age.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Lozinsky AC, Morais MB. Eosinophilic colitis in infants. J Pediatr (Rio J). 2014;90:16–21.