To evaluate the effectiveness of a thermoregulation bundle for preventing admission hypothermia in very low-birth weight preterm infants.
MethodsInterventional study with retrospective evaluation of data undertaken in a tertiary neonatal unit including all very low-birth weight preterm infants (<1500g) born at and admitted to the unit. Two periods were compared: before intervention (PI; 01/01/2012 to 02/28/2014_ and after intervention (PII; 04/01/2014 to 11/30/2016). The intervention started in March 2014. At PI procedures in the delivery room were: placement in a crib with a radiant heat source, doors always closed, polyethylene body plastic bag, double cap (plastic and cotton mesh), room temperature between 24 to 27°C and transport to neonatal unit in a pre-heated incubator (36–37.0°C). At PII, there was a reinforcement on not opening the plastic bag during the entire resuscitation process, even at an advanced stage, and the anthropometric measures and routine care were performed in the neonatal unit. Maternal, delivery, and neonatal variables were compared. Admission hypothermia was considered when admission axillary temperature was <36.0°C. Periodic results were shown to the team every six months and results were discussed.
ResultsThe incidence of admission hypothermia was reduced significantly in PII (37.2 vs. 14.2%, p<0.0001) and admission temperature medians were higher (36.1 vs. 36.5°C, p<0.001). At PII, there was an increase in the number of infants transported with oxygen (49.5 vs. 75.5%, p<0.0001). No differences were observed regarding birth weight and gestational age.
ConclusionThere was a very important reduction in admission hypothermia incidence and a higher median admission temperature after continued protocol implementation.
Avaliar a efetividade de um programa de medidas para prevenção de hipotermia à admissão em recém-nascidos pré-termo de muito baixo peso.
MétodosEstudo de intervenção com coleta retrospectiva de dados em unidade neonatal terciária que incluiu todos os recém-nascidos pré-termo de muito baixo peso (< 1.500g) nascidos e admitidos na unidade. Foram comparados dois períodos: antes da intervenção PI - 01/01/2012 a 28/02/2014 e depois da intervenção PII - 01/04/2014 a 30/11/2016. O mês de março de 2014 foi o início da intervenção. Em PI as medidas em sala de parto foram: recepção em berço de calor radiante, portas sempre fechadas, uso de saco plástico corporal, colocação de dupla touca (plástico e malha) na cabeça, temperatura ambiental entre 24-27°C e transporte em incubadora aquecida (36-37,0°C). No PII reforçou-se a não abertura do saco plástico durante toda reanimação mesmo que avançada e dados antropométricos e cuidados rotineiros realizados na unidade de internação. Variáveis maternas, de parto e neonatais foram comparadas entre os dois períodos. A hipotermia à admissão foi considerada quando temperatura axilar<36,0°C. Resultados parciais foram apresentados e discutidos com a equipe semestralmente.
ResultadosA incidência da hipotermia à admissão diminuiu significativamente em PII (37,2 x14,2%, p<0,0001) e a mediana de temperatura foi mais elevada (36,1x36,5° C, p<0,001). Houve aumento significativo do número de crianças transportadas com oxigênio em PII (49,5 x 75,5%, p<0,0001). Não houve diferenças para peso ao nascer e idade gestacional.
ConclusãoHouve redução acentuada de hipotermia à admissão e melhora na mediana da temperatura de admissão hospitalar em recém-nascidos pré-termo de muito baixo peso após implantação do protocolo.
Newborns are prone to rapid body temperature drop through the mechanisms of convection, evaporation, conduction, and radiation. In the first 10–20min of life, if there is no intervention to prevent heat loss, the infant's temperature can decrease by 2–4°C.1,2 The lower the gestational age and the birth weight, the more significant these losses are and the higher the risk of hypothermia.3,4 This phenomenon is due to the fact that very low birth weight (VLBW) preterm infants have a relatively large body surface area, thin skin, scarcity of subcutaneous tissue, low glycogen stores, and almost absent brown fat stores, as well as the incapacity of producing tremors to generate heat and inadequate vascular control for thermoregulation.2
Exposure to low body temperature is directly related to higher morbidity and mortality rates.3–5 The study by Laptook et al.3 demonstrated that the newborns’ admission temperature to the neonatal unit (NU) was inversely related to in-hospital mortality, with a 28% increase in the mortality rate per every 1°C of decrease in the admission temperature in VLBW infants. Additionally, admission hypothermia (AH) increases the risk of late sepsis,3 increases the rate of oxygen consumption, causes pulmonary and systemic vasoconstriction, and is associated with worsening of respiratory distress, metabolic acidosis, hypoglycemia, coagulation disorder, and peri-intraventricular hemorrhage.2,6
One of the major challenges in neonatology is the maintenance of normothermia from birth to NU admission. In 2011, the Brazilian Society of Pediatrics (SBP) included hypothermia prevention methods into the neonatal resuscitation program, such as maintenance of temperature in the delivery rooms between 23 and 26°C, resuscitation under a radiant heat source, use of plastic body bag, use of double cap (plastic and cotton) on the infant's head, and transport to the NU in heated incubators. These measurements aim to maintain the body temperature between 36.5 and 37.5°C.7
AH is frequently observed in NUs, even in those with advanced technological support, ranging from 31% to 90% in NU in the United States.8 Data from the Brazilian Neonatal Research Network indicate AH rates (axillary temperature <36°C) of VLBW infants in the 20 registered neonatal intensive care units ranging from 9% to 91% in the year 2015.9
Thus, the aim of this study was to evaluate the outcome of prevention measures on the AH rates in VLBW newborns in a tertiary NU in two distinct periods, before and after an intervention program.
MethodsThis was an intervention study with retrospective data collection, carried out in the Division of Neonatology of Hospital da Mulher Prof. Dr. José Aristodemo Pinotti – Centro de Atenção Integral à Saúde da Mulher of Universidade Estadual of Campinas, São Paulo, Brazil. It is a public tertiary university NU with 30 beds. The study population included all live VLBW newborns (<1500g) admitted to the NU, except for deaths in the delivery room and those born outside the institution.
Two periods were analyzed. The first period (PI) corresponded to the pre-intervention period, from 01/01/2012 to 02/28/2014, and the second period (PII) corresponded to the post-intervention period, from 04/01/2014 to 11/30/2016. The month of March 2014 was excluded from the analysis because it was the beginning of the intervention period.
The assessed outcome was the rate of AH, verified before and after the intervention. AH was defined as axillary temperature <36°C, measured by digital thermometer, when the newborn arrived at the NU.
To evaluate the intervention effect on the AH outcome, in addition to the temperature of the VLBW infants in the intensive care unit, maternal, delivery, and newborn characteristics were evaluated aiming to verify variables that could interfere with this response.
The maternal variables analyzed were: ethnicity, type of pregnancy (single or twin), type of delivery, prenatal care, use of magnesium sulfate, antenatal use of corticosteroids, maternal fever (>37.8°C), antepartum hypertension, diabetes mellitus, congenital infection, chorioamnionitis,10 and peripartum hemorrhage.
The delivery and neonatal variables analyzed were: gender, birth weight, gestational age, need for resuscitation (defined as the need for positive pressure ventilation in the delivery room), advanced resuscitation (defined as the need for tracheal intubation followed by chest compression and/or medication use), surfactant use in the delivery room, Apgar score at the 1st and 5th minutes, use of oxygen during transport, and early death (<7 days).
Maternal and neonatal data were retrieved from an internal, computerized database of the Brazilian Neonatal Research Network (Rede Brasileira de Pesquisas Neonatais [RBPN]).
The intervention consisted in a continuous education process on hypothermia prevention measures in the delivery room and during the transport of newborns to the NU. Prevention measures have been used since 2011, based on the guidelines of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics7 and included, among other measures: placement in a crib with a radiant heat source, permanently adjusted between 35 and 36°C; keeping the room doors always closed; use of polyethylene plastic bag for the newborn's body without drying it; covering the head with a plastic cap and a cotton cap after drying the fontanelle region; maintenance of the temperature in the resuscitation room at 24–27°C; and transportation to the hospital admission unit in a heated incubator permanently on and adjusted to a temperature of 35–37°C.
The plastic body bag used was made of polyethylene, measuring 30cm×40cm, with a T-shirt-type opening and a border that allowed closure at the other end.
In March 2014, the medical and nursing staff underwent training, requalification, and sensitization regarding the measures. In addition to the abovementioned measures, implementing the practice of not opening the plastic bag was included in the entire reception process, even if advanced resuscitation was required; anthropometric data collection, anti-hepatitis B vaccination, and non-essential procedures stopped being performed in the delivery room and were performed at the ward.
As the results were collected, they were periodically presented to the team by e-mail, administrative announcements, and face-to-face meetings, at six-month intervals, with positive reinforcements in cases of success and requesting compliance with the standards in case of AH.
Categorical variables were expressed by absolute and relative frequencies and evaluated by the chi-squared test, whereas continuous variables were expressed by medians and interquartile ranges and compared by Mann–Whitney test. The final accepted significance level was 5% and the statistical package used was the SPSS (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY, USA).
The study was approved by the research ethics committee (CONEP – Plataforma Brasil), Opinion No. 1.018.827 de 09/04/2015.
ResultsA total of 475 infants with very low-birth weight were assessed, after being divided into two groups according to the periods: 218 in the PI and 257 in the PII.
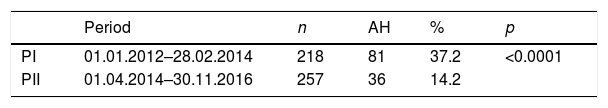
The incidence of AH decreased significantly in PII, with a reduction from 37.2% to 14.2% (p<0.0001). In the annual distribution of the AH rate, high values of AH were observed in the PI years, with a decrease and maintenance of the annual values during the three years of PII. Although there was an increase in the rate in 2016, this difference did not reach statistical significance when compared with the years 2014/2015 (19.4 vs. 13.0%; p=0.179; Table 1).
Percentage distribution of admission hypothermia according to the periods and years.
| Period | n | AH | % | p | |
|---|---|---|---|---|---|
| PI | 01.01.2012–28.02.2014 | 218 | 81 | 37.2 | <0.0001 |
| PII | 01.04.2014–30.11.2016 | 257 | 36 | 14.2 |
| Years | n | AH | % |
|---|---|---|---|
| 2012 | 102 | 41 | 40.2 |
| 2013 | 97 | 35 | 36.1 |
| 2014 | 84 | 12 | 14.3 |
| 2015 | 115 | 14 | 12.2 |
| 2016 | 77 | 15 | 19.4 |
PI, period I; PII, period II; AH, admission hypothermia.
A significant improvement was observed in the median temperature at hospital admission in PII (36.1 vs. 36.5°C; p<0.001). In PII, among the patients with AH, 23 weighed less than 1000g, representing 63.9% of the group, and 17 had less than 28 weeks of gestational age, representing 47.2%. Hyperthermia was not observed in PI, whereas 11 cases (4.3%) were observed in PII.
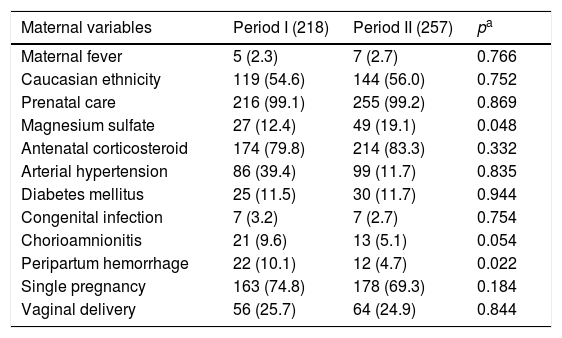
When analyzing maternal and obstetric variables in PI and PII, a significant increase in the use of magnesium sulfate (12.4% vs. 19.1%, p=0.048) and a decrease in the incidence of peripartum hemorrhage (10.1 vs. 4.7%; p=0.022) were observed, as shown in Table 2.
Percentage distribution of maternal and delivery variables according to the periods.
| Maternal variables | Period I (218) | Period II (257) | pa |
|---|---|---|---|
| Maternal fever | 5 (2.3) | 7 (2.7) | 0.766 |
| Caucasian ethnicity | 119 (54.6) | 144 (56.0) | 0.752 |
| Prenatal care | 216 (99.1) | 255 (99.2) | 0.869 |
| Magnesium sulfate | 27 (12.4) | 49 (19.1) | 0.048 |
| Antenatal corticosteroid | 174 (79.8) | 214 (83.3) | 0.332 |
| Arterial hypertension | 86 (39.4) | 99 (11.7) | 0.835 |
| Diabetes mellitus | 25 (11.5) | 30 (11.7) | 0.944 |
| Congenital infection | 7 (3.2) | 7 (2.7) | 0.754 |
| Chorioamnionitis | 21 (9.6) | 13 (5.1) | 0.054 |
| Peripartum hemorrhage | 22 (10.1) | 12 (4.7) | 0.022 |
| Single pregnancy | 163 (74.8) | 178 (69.3) | 0.184 |
| Vaginal delivery | 56 (25.7) | 64 (24.9) | 0.844 |
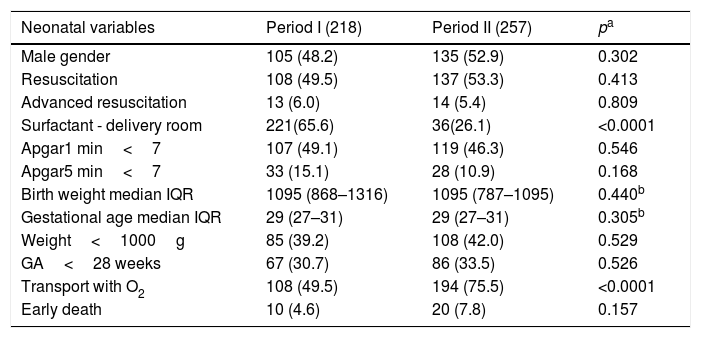
Regarding the neonatal variables, surfactant use in the delivery room decreased significantly in the comparison between the two periods (65.6% vs. 26.1%; p<0.0001) and the need for O2 during transport increased significantly in the PII (49.5% vs. 75.5%; p<0.0001), as shown in Table 3. The other variables analyzed were quantitatively similar in both periods.
Distribution of neonatal variables according to the periods.
| Neonatal variables | Period I (218) | Period II (257) | pa |
|---|---|---|---|
| Male gender | 105 (48.2) | 135 (52.9) | 0.302 |
| Resuscitation | 108 (49.5) | 137 (53.3) | 0.413 |
| Advanced resuscitation | 13 (6.0) | 14 (5.4) | 0.809 |
| Surfactant - delivery room | 221(65.6) | 36(26.1) | <0.0001 |
| Apgar1 min<7 | 107 (49.1) | 119 (46.3) | 0.546 |
| Apgar5 min<7 | 33 (15.1) | 28 (10.9) | 0.168 |
| Birth weight median IQR | 1095 (868–1316) | 1095 (787–1095) | 0.440b |
| Gestational age median IQR | 29 (27–31) | 29 (27–31) | 0.305b |
| Weight<1000g | 85 (39.2) | 108 (42.0) | 0.529 |
| GA<28 weeks | 67 (30.7) | 86 (33.5) | 0.526 |
| Transport with O2 | 108 (49.5) | 194 (75.5) | <0.0001 |
| Early death | 10 (4.6) | 20 (7.8) | 0.157 |
IQR, interquartile range (p25-p75); O2, oxygen.
The maintenance of normothermia at birth and at hospital admission is a challenge in neonatal practice, especially when caring for preterm newborns.
The study showed successful prevention of AH in VLBW newborns using standardized care in the delivery room, in addition to continuing training and a team dedicated to strictly following the standards. The set of measures resulted in a sharp rate decrease in the period immediately after the intervention, persisting in the following years, because the training continued and the results were periodically reported to the teams. It is noteworthy that not only did the AH rates decrease, but also the median admission temperature improved, in agreement with the World Health Organization's standard of normothermia (36.5 to 37.5°C).1
To the best of the authors’ knowledge, this is the first Brazilian publication to present an intervention process to fight AH in very low-birth weight infants.
Similarly, Pinheiro et al.8 used a set of measures for hypothermia reduction in the delivery room in a study with 641 VLBW newborns and obtained a considerable reduction in the AH rates, which previously reached values as high as 60%, to approximately 10% after the training; this reduction persisted in the following three years. Data by Manani et al.11 were also of interest, showing reduction in AH in VLBW infants from 44% to 0% from 2006 to 2009; after a slight increase to 6% in 2010, the rate returned to 0% in 2011 through continuous retraining and reporting of results to the team.
When analyzing the maternal variables, a significant increase was observed in the number of pregnant women who used magnesium sulfate as a consequence of a new practice used by the obstetrics team in 2015, aiming at the neuroprotection of the newborns with gestational age <32 weeks. This fact could result in an increase in the AH rates due to the side effects that hypermagnesemia can cause in the newborn, such as myorelaxation and respiratory depression,12 increasing the need for neonatal resuscitation and prolonging the newborn's length of stay in the delivery room. However, the study showed no significant differences between the periods regarding the resuscitation rates and the Apgar scores at the 1st and 5th minutes.
Other recent studies have also shown that the use of magnesium sulfate for neuroprotection in VLBW preterm infants did not increase the occurrence of a 5-minute Apgar score <7, the need for positive pressure ventilation through mask or tracheal tube, chest compressions in the delivery room, and either hypotonia or hypotension at admission.13,14
In the present study, inversely to the increased use of magnesium sulfate for neuroprotection, a decrease in AH rates was observed in the same period; the authors attributed to this result the improvement in care caused by the implementation of the preventive method set.
A significant reduction in peripartum maternal hemorrhage was observed during the second period. Although maternal bleeding may be related to perinatal suffering and increased need for resuscitation, leading to the newborn's greater exposure to environmental factors for heat loss, no differences were observed in the study.
When analyzing the neonatal variables, the use of surfactant in the delivery room significantly decreased from 2013, due to the discontinuation of its prophylactic use in infants <30 weeks of gestational age. This fact may have contributed to the reduction in the number of cases of AH, since this practice kept the newborn for longer periods in the delivery room exposed to conditions favorable to hypothermia.8
Among the neonatal variables, there was a significant increase in the use of oxygen (O2) during the transport of VLBW newborns to the NU in PII. The authors were unable to identify a hypothesis to justify the finding. This fact could contribute negatively to the maintenance of normothermia in these newborns exposed to cold O2 and compressed air, since the inhalation gases used in resuscitation in the delivery room and during transport have a temperature of approximately 21±1.5°C and are not humidified. To solve this problem, heat moisture exchange (HME), single-use disposable devices that are attached to the tracheal tube and maintain the patient's own temperature and humidity, could be used; alternatively, adequate humidifiers and heaters that allow connection to the tubular systems of manual mechanical ventilators with a T-piece could be used, but they are costly and rarely available in Brazil.
Meyer et al.15 also observed a reduction of 35% in the AH after the adoption of heated and humidified gases used in the resuscitation and transport of the newborns, which was beneficial for infants with <32 weeks and mainly for those with <28 weeks of gestational age. In another study, Pas et al.16 demonstrated that the offer of heated humidified gas during respiratory support from birth to admission increased the mean body temperature of the VLBW infants by 0.5°C.
The current neonatal resuscitation program of the SBP suggests the use of chemical thermal mattress for newborns weighing <1000g, associated with the use of plastic bag and double cap.17 Exothermic mattresses contain sodium acetate gel and are activated by pressing a metal disc, which causes the gel to crystallize and produce latent heat. These mattresses require activation before their use.18
There is controversy over the routine use of thermal mattresses.19 McCarthy et al.18 compared the admission temperature of infants placed in the polyethylene bags and newborns received with exothermic mattresses together with plastic bags in the delivery room and found that the admission temperature was similar between the groups. Hypothermia and hyperthermia occurred more frequently in infants placed in plastic bags and on mattresses, and a higher normothermic index was observed in the group in which only the plastic bag was used.
However, Pinheiro et al.6 and Chawla et al.20 obtained favorable results with the use of chemical thermal mattresses in association with the other recommended measures, and observed a reduction in the hypothermia rate and an increase in the mean temperature of the infants at admission, with this increase being 0.4°C in the first study and 0.5°C in the second.
In the present study, even without the use of the thermal mattress, a marked reduction in the AH rate was achieved, demonstrating that the absence of this resource did not directly interfere with the intervention success. Care should also be taken for undesired outcomes, such as hyperthermia, which occurred in 11 cases after the intervention, as it also contributes to the morbidity and mortality of the newborns.8
One of the reasons that may have favored the present results is the short distance between the delivery room and the local admission unit, which requires approximately 5min of transport, carried out in double-wall transport incubators, maintaining the temperature between 35 and 37°C, with the newborns enveloped in a plastic bag and a double cap. The removal of the plastic bag and caps only occurred after thermal stabilization at admission, with axillary temperature between 36.5 and 37.5°C, as recommended by the SBP National Neonatal Resuscitation Program.17
However, one of the study limitations, considering it was a retrospective study, was the non-availability of real-time evaluation between birth, transport, and admission to the NU, making it impossible to infer whether a shorter time spent for the infant's admission could have contributed to rate improvement.
In conclusion, with the measures implemented in the service, a significant reduction in the AH rate and an improvement in the median temperature at the time of hospital admission were observed.
With the perspective of improvement, much can still be done to eliminate hypothermia in VLBW infants, reducing the rate of AH to less than 10%. The standardization of evidence-based care requires an extensive and continuous education of the teams, with periodic result presentation, thus improving adherence to practices. Moreover, the use of a thermal mattress and heated and humidified gas may be beneficial for this population and further increase the rate of hypothermia improvement found in this study.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Caldas JP, Millen FC, Camargo JF, Castro PA, Camilo AL, Marba ST. Effectiveness of a measure program to prevent admission hypothermia in very low-birth weight preterm infants. J Pediatr (Rio J). 2018;94:368–73.
Study carried out at Universidade Estadual de Campinas (UNICAMP), Faculdade de Ciências Médicas (FCM); e Universidade Estadual de Campinas (UNICAMP), Centro de Atenção Integral à Saúde da Mulher (CAISM), Hospital da Mulher Prof. Dr. José Aristodemo Pinotti, Divisão de Neonatologia, Campinas, SP, Brazil.