Several reports claim that blood pressure (BP) in the radial artery may underestimate the accurate BP in critically ill patients. Here, the authors evaluated differences in mean blood pressure (MBP) between the radial and femoral artery during pediatric cardiac surgery to determine the effectiveness of femoral arterial BP monitoring.
MethodThe medical records of children under 1 year of age who underwent open-heart surgery between 2007 and 2013 were retrospectively reviewed. Radial and femoral BP were measured simultaneously, and the differences between these values were analyzed at various times: after catheter insertion, after the initiation of cardiopulmonary bypass (CPB-on), after aortic cross clamping (ACC), after the release of ACC, after weaning from CPB, at arrival in the intensive care unit (ICU), and every 6h during the first day in the ICU.
ResultsA total of 121 patients who underwent open-heart surgery met the inclusion criteria. During the intraoperative period, from the beginning to the end of CPB, radial MBPs were significantly lower than femoral MBPs at each time-point measured (p<0.05). Multivariate analysis showed that longer CPB time (>60min, odds ratio: 7.47) was a risk factor for lower radial pressure. However, discrepancies between these two values disappeared after arrival in the ICU. There was no incidence of ischemic complications associated with the catheterization of both arteries.
ConclusionThe authors suggest that femoral arterial pressure monitoring can be safely performed, even in neonates, and provides more accurate BP values during CPB-on periods, and immediately after weaning from CPB, especially when CPB time was greater than 60min.
Diversos relatos alegam que a pressão arterial (PA) na artéria radial poderá subestimar a PA precisa em pacientes gravemente doentes. Aqui, avaliamos diferenças na pressão arterial média (PAM) entre a artéria radial e femoral durante cirurgia cardíaca pediátrica para determinar a eficácia do monitoramento da PA da artéria femoral.
MétodoRealizamos uma análise retrospectiva de prontuários médicos de crianças com menos de 1 ano de idade submetidas a cirurgia de coração aberto entre 2007 e 2013. As PAs radial e femoral foram auferidas simultaneamente, as diferenças entre esses valores foram analisadas diversas vezes: após a inserção do cateter, após o início do bypass cardiopulmonar (CPB-on), após pinçamento cruzado da aorta (ACC), após a liberação do ACC, após desmame do CPB, na entrada na unidade de terapia intensiva (UTI) e a cada 6 horas durante o primeiro dia na unidade de terapia intensiva (UTI).
ResultadosUm total de 121 pacientes submetidos a cirurgia de coração aberto atenderam aos nossos critérios de inclusão. Durante o transoperatório, do início ao término do CPB, as PAMs da artéria radial foram significativamente menores do que as PAMs da artéria femoral em cada ponto de medição (p < 0,05). A análise multivariada mostrou que a duração mais longa do CPB (> 60 minutos, Razão de Chance = 7,47) representou um fator de risco de pressão radial mais baixa. Contudo, as diferenças entre esses dois valores desapareceram após a entrada na UTI. Não houve incidência de complicações isquêmicas associadas à cateterização de ambas as artérias.
ConclusãoSugerimos que o monitoramento da pressão arterial femoral pode ser realizado com segurança, mesmo em neonatos, e fornece valores da PA mais precisos durante períodos de CPB-on e imediatamente após o desmame do CPB, principalmente nos casos em que a duração do CPB foi superior a 60 minutos.
Invasive blood pressure (BP) monitoring is essential for patients during and after open-heart surgery (OHS), and the radial artery is the most common site of catheterization during OHS. However, many investigators have reported that, in adults, during the early phase of cardiopulmonary bypass (CPB), the femoral arterial pressure is significantly higher than the peripheral arterial pressure.1,2 However, to the best of the authors’ knowledge, few studies have investigated the difference between femoral and radial arterial BP during surgery and postoperative period in neonates and infants.
In the present study, the differences in BP between the radial and femoral arteries in neonates and infants during the perioperative period were evaluated to determine whether they were clinically relevant, and to identify the patient groups in which these differences occurred.
Materials and methodsThis was a respective review of data, and the study was approved by the Institutional Review Board (CNUH-2015-024). The authors retrospectively reviewed both surgical and medical data of patients under 1 year of age who had undergone open-heart surgery between January 2007 and December 2013. The exclusion criteria were as follows: OHS without ACC, CPB weaning failure, conversion to extracorporeal membrane oxygenation support, early hospital mortality (<24h), lack of simultaneous catheterization in the radial and femoral arteries, and congenital heart disease that could have affected the discrepancy in BP of these arteries, such as aortic arch anomalies. Demographic data, including age at diagnosis, age at surgery, sex, weight, height, and body surface area, were reviewed. Preoperative factors, such as cardiac diagnosis and medications were also reviewed in all patients. Among the intraoperative data, the duration of CPB and ACC time was assessed.
Radial and femoral arterial catheters were placed after induction of anesthesia. Radial cannulation was performed with a 24G Jelco® IV Radiopaque Catheter (Smith Medical International Ltd. – Rossendala, United Kingdom). Femoral arterial catheterization was performed using the Seldinger technique with a 22-G and 4.45-cm radiopaque catheter in a pediatric multi-lumen central venous catheterization set with a Blue FlexTip® catheter (Teleflex Medical – Plymouth, MN, USA). The arterial catheters were connected to two pressure transducers (Transpac® IV monitoring kit; ICU Medical – San Clemente, CA, USA). The pressure transducer was placed at the level of the right atrium. Systolic blood pressure (SBP), diastolic blood pressure (DBP), and MBP of each artery were measured continuously and simultaneously. All numbers were recorded in a digital chart by anesthesiologists every 5min in the operating room (OR) and by intensive care unit (ICU) nurses every 1h in the ICU. The detailed single digits were available.
BP values from both arteries were assessed at various times: preoperative (after catheter insertion following induction of anesthesia and prior to skin incision), intraoperative (after the beginning of CPB, after ACC, after release of ACC, and after weaning from CPB), and postoperative period (every 6h during the first day in the ICU). The MBP data between the two arteries were then compared. The patients were divided into subgroups according to age (neonates and early infants less than 3 months and older infants between 3 and 12 months), according to CPB time (<60min, 60–120min, >120min), and according to the vasoactive inotropic score (VIS) calculated from the mean VIS values within the first 24h in ICU (<20, 20–40, >40). Then, the differences between radial and femoral MBP were assessed in each subgroup. The VIS was calculated as follows: dopamine dose (mcg/kg/min)+dobutamine (mcg/kg/min)+100×epinephrine dose (mcg/kg/min)+10×milrinone dose (mcg/kg/min)+10,000×vasopressin dose (U/kg/min)+100×norepinephrine dose (mcg/kg/min).3
The t-test for independent samples was used to compare continuous variables between groups. Repeated measures analysis of variance (ANOVA) was used to compare the serial values between radial and femoral arterial pressure during the operation and ICU stay. Odds ratios with 95% confidence intervals were calculated by logistic regression analysis according to the risk of lower blood pressure in the radial artery during CPB weaning period. In all analyses, p-values <0.05 were considered to indicate statistical significance. The statistical software package SPSS (IBM Statistics for Windows, Version 21.0, NY, USA) was used for all data analyses.
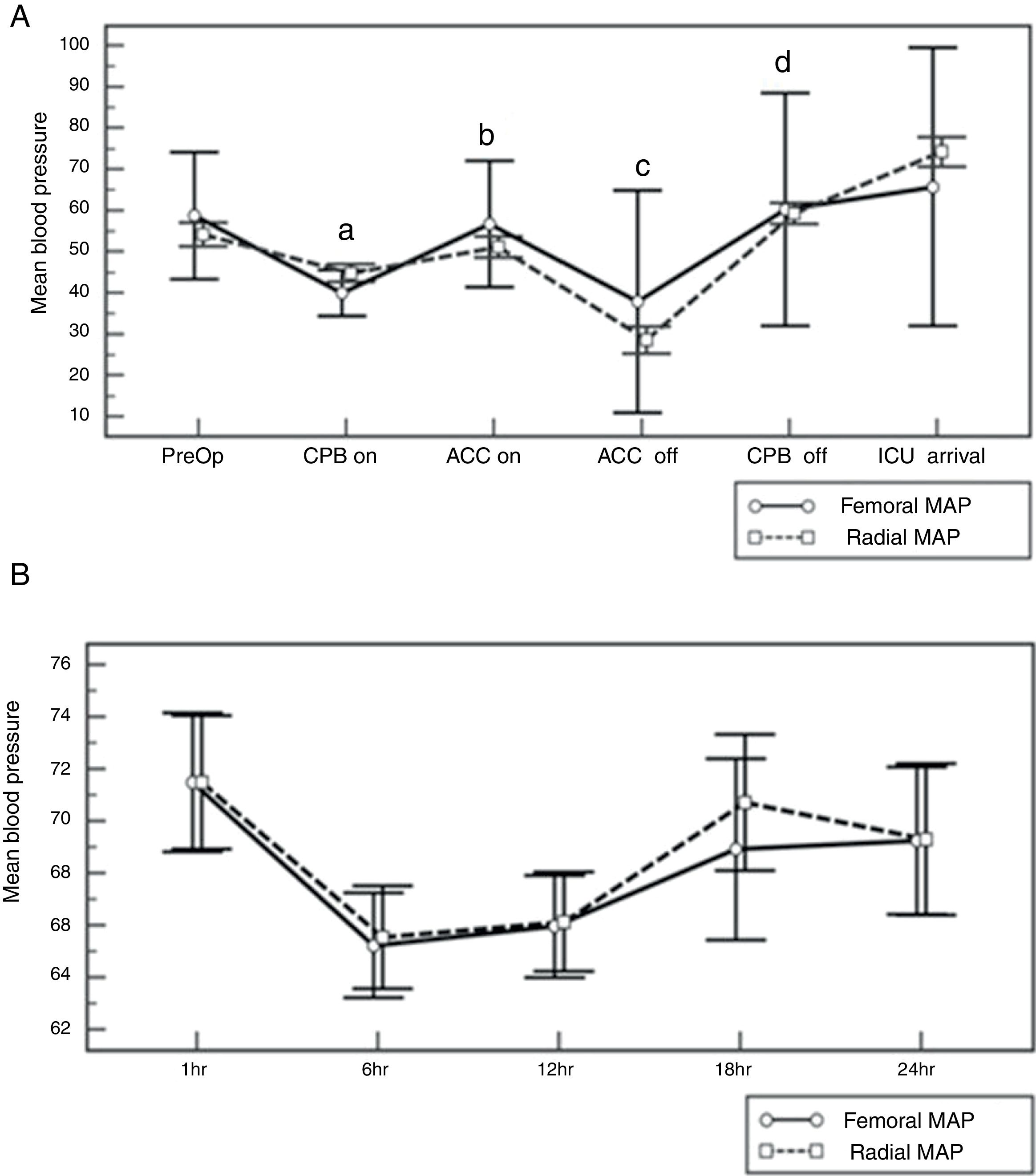
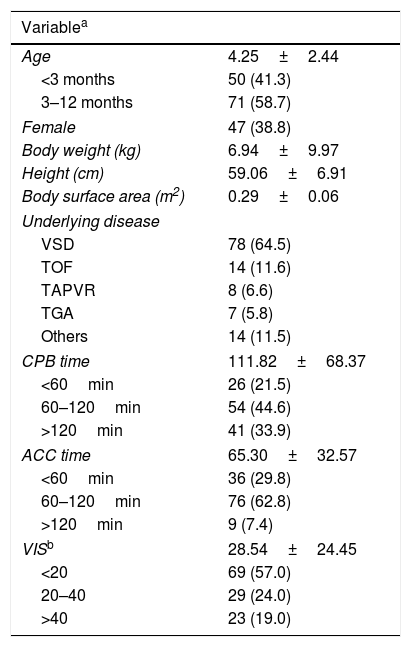
ResultsPatient demographics during preoperative periodA total of 121 patients who underwent open-heart surgery fulfilled our inclusion criteria. The study population consisted of 50 patients (41.3%) under 3 months of age and 71 patients (58.7%) between 3 and 12 months. Mean body weight was 6.94±9.97kg. Mean CPB time was 111.82±68.37min, mean ACC time was 65.30±32.57min, and mean VIS was 28.54±24.45 (Table 1). No significant differences were observed in BP between the femoral and radial arteries prior to the initiation of CPB (Fig. 1).
Patients’ characteristics during the perioperative period (n=121 patients).
| Variablea | |
|---|---|
| Age | 4.25±2.44 |
| <3 months | 50 (41.3) |
| 3–12 months | 71 (58.7) |
| Female | 47 (38.8) |
| Body weight (kg) | 6.94±9.97 |
| Height (cm) | 59.06±6.91 |
| Body surface area (m2) | 0.29±0.06 |
| Underlying disease | |
| VSD | 78 (64.5) |
| TOF | 14 (11.6) |
| TAPVR | 8 (6.6) |
| TGA | 7 (5.8) |
| Others | 14 (11.5) |
| CPB time | 111.82±68.37 |
| <60min | 26 (21.5) |
| 60–120min | 54 (44.6) |
| >120min | 41 (33.9) |
| ACC time | 65.30±32.57 |
| <60min | 36 (29.8) |
| 60–120min | 76 (62.8) |
| >120min | 9 (7.4) |
| VISb | 28.54±24.45 |
| <20 | 69 (57.0) |
| 20–40 | 29 (24.0) |
| >40 | 23 (19.0) |
ACC, aortic cross clamp; CPB, cardiopulmonary bypass; TAPVR, total anomalous pulmonary venous return; TOF, tetralogy of Fallot; TGA, transposition of great arteries; VIS, vasoactive inotropic score; VSD, ventricular septal defect.
Change of mean blood pressure in the radial and femoral artery according to time. (A) Comparison of mean blood pressure during the intra-operative period (a, b, c, d: p<0.05). (B) Comparison of mean blood pressure within the first post-operative 24h. ACC, aortic cross clamp; CPB, cardiopulmonary bypass; ICU, intensive care unit; MAP, mean arterial pressure; PreOp, preoperative.
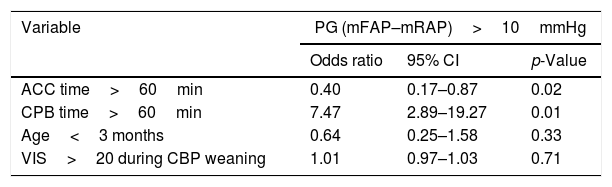
From the beginning to the end of CPB, radial MBPs were significantly lower than femoral MBPs at each time-pint measured (p<0.05; Fig. 1). The authors also analyzed the characteristics of the patients who had a radial MBP lower than 10mmHg compared with the femoral MBP during the CPB weaning period; this applied to 37 patients (30.1%). Multivariate analysis revealed that a longer CPB time (>60min) represented a risk factor for lower radial pressure (Table 2).
Multivariate analyses of lower blood pressure in the radial artery during the CPB weaning period.
| Variable | PG (mFAP–mRAP)>10mmHg | ||
|---|---|---|---|
| Odds ratio | 95% CI | p-Value | |
| ACC time>60min | 0.40 | 0.17–0.87 | 0.02 |
| CPB time>60min | 7.47 | 2.89–19.27 | 0.01 |
| Age<3 months | 0.64 | 0.25–1.58 | 0.33 |
| VIS>20 during CBP weaning | 1.01 | 0.97–1.03 | 0.71 |
ACC, aortic cross clamp; CI, confidential interval; CPB, cardiopulmonary bypass; FAP, femoral arterial pressure; m, mean; PG, pressure gradient; RAP, radial arterial pressure; VIS, vasoactive inotropic score.
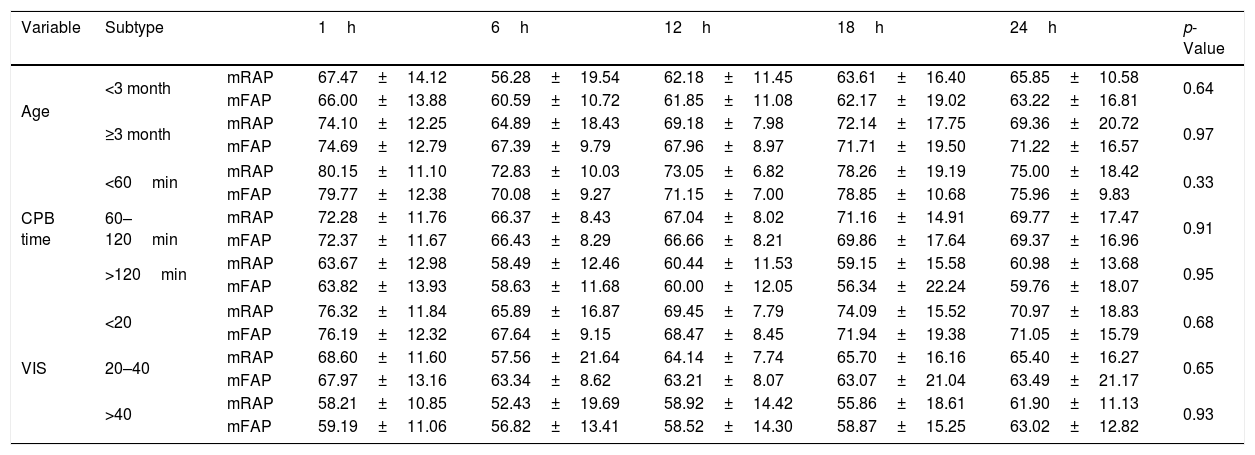
During the postoperative period, no significant differences in MBP were observed between the two arteries (Fig. 1). Even when patients were divided into subgroups according to age, CPB time, and VIS, the analysis showed no significant differences between the radial and femoral MAP for each subgroup (Table 3).
Comparison of radial and femoral arterial pressure within the first 24h postoperative.
| Variable | Subtype | 1h | 6h | 12h | 18h | 24h | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Age | <3 month | mRAP | 67.47±14.12 | 56.28±19.54 | 62.18±11.45 | 63.61±16.40 | 65.85±10.58 | 0.64 |
| mFAP | 66.00±13.88 | 60.59±10.72 | 61.85±11.08 | 62.17±19.02 | 63.22±16.81 | |||
| ≥3 month | mRAP | 74.10±12.25 | 64.89±18.43 | 69.18±7.98 | 72.14±17.75 | 69.36±20.72 | 0.97 | |
| mFAP | 74.69±12.79 | 67.39±9.79 | 67.96±8.97 | 71.71±19.50 | 71.22±16.57 | |||
| CPB time | <60min | mRAP | 80.15±11.10 | 72.83±10.03 | 73.05±6.82 | 78.26±19.19 | 75.00±18.42 | 0.33 |
| mFAP | 79.77±12.38 | 70.08±9.27 | 71.15±7.00 | 78.85±10.68 | 75.96±9.83 | |||
| 60–120min | mRAP | 72.28±11.76 | 66.37±8.43 | 67.04±8.02 | 71.16±14.91 | 69.77±17.47 | 0.91 | |
| mFAP | 72.37±11.67 | 66.43±8.29 | 66.66±8.21 | 69.86±17.64 | 69.37±16.96 | |||
| >120min | mRAP | 63.67±12.98 | 58.49±12.46 | 60.44±11.53 | 59.15±15.58 | 60.98±13.68 | 0.95 | |
| mFAP | 63.82±13.93 | 58.63±11.68 | 60.00±12.05 | 56.34±22.24 | 59.76±18.07 | |||
| VIS | <20 | mRAP | 76.32±11.84 | 65.89±16.87 | 69.45±7.79 | 74.09±15.52 | 70.97±18.83 | 0.68 |
| mFAP | 76.19±12.32 | 67.64±9.15 | 68.47±8.45 | 71.94±19.38 | 71.05±15.79 | |||
| 20–40 | mRAP | 68.60±11.60 | 57.56±21.64 | 64.14±7.74 | 65.70±16.16 | 65.40±16.27 | 0.65 | |
| mFAP | 67.97±13.16 | 63.34±8.62 | 63.21±8.07 | 63.07±21.04 | 63.49±21.17 | |||
| >40 | mRAP | 58.21±10.85 | 52.43±19.69 | 58.92±14.42 | 55.86±18.61 | 61.90±11.13 | 0.93 | |
| mFAP | 59.19±11.06 | 56.82±13.41 | 58.52±14.30 | 58.87±15.25 | 63.02±12.82 | |||
CPB, cardiopulmonary bypass; FAP, femoral arterial pressure; m, mean; RAP, systolic radial arterial pressure; s, systolic; VIS, vasoactive inotropic score.
The formation of small (<2cm) hematomas occurred in three patients and local infection was observed in one patient. There were no cases of perfusion-related limb ischemia in either of the arteries.
DiscussionMany investigators have reported the safety of femoral arterial catheterization during adult cardiac surgery4,5; however, studies on the characteristics of femoral arterial pressure monitoring in neonates and infants are few. In the present study, the authors examined the differences between femoral and radial blood pressure in neonates and infants and observed that radial arterial pressure was usually underestimated as compared to femoral arterial pressure during the CPB-on period in this population. However, this phenomenon did not extend into the ICU period.
In general, as the arterial pressure waveform moves toward the peripheral artery, the systolic pressure gradually increases and the systolic portion of the waveforms becomes narrower. Diastolic pressure usually decreases and mean pressure remains unchanged or decreases minimally.6 However, this phenomenon is influenced by the clinical condition of the patient, including the presence of peripheral vascular disease, the use of vasoactive agents, and body temperature.7–9
Cardiac surgery with CPB is the most important factor affecting discrepancies in intra-arterial pressure between central and peripheral arteries, and several studies have reported such findings during and after adult cardiac surgery; this has become an established pathophysiological feature of adult cardiac surgery.1,2 Vasomotor dysfunction after cardiac surgery with CPB results in reduced peripheral vascular resistance, which clinically manifests as an underestimation of BP in the peripheral arteries. This phenomenon occurs secondary to abnormal vascular permeability and tissue edema, which can contribute to dysfunction in the heart, lung, brain, kidneys, and other organs.10,11 Therefore, although the peripheral arterial pressure, such as that in the radial artery, is more commonly monitored during cardiac surgery, it tends to be underestimated and its reliability has been called into question.
Reduced radial arterial pressure can be caused by vasospasm as a result of certain thermoregulatory mechanisms; similarly, femoral to radial pressure gradients have been observed in patients with hypothermic circulatory arrest or in critically ill surgical patients treated with high doses of vasoactive agents.9,12,13 Chauhan et al.1 reported that FAP monitoring was more reliable during the initial part of CPB in 60 patients of all ages (range: 3–65 years) undergoing cardiac surgery. These authors found that femoral arterial pressure was higher than radial arterial pressure during CPB, especially during the initiation of CPB; however, the differences between the radial and femoral arterial pressure were lower after 60min of CPB. Their study population consisted of 60 patients, and included a wide age range; this represented a major difference when compared to the present study, which focused only on patients younger than 1 years of age and found that femoral arterial pressure was higher at the initiation of CPB and immediately after ACC release in all neonates and infants.
In the present study, the location of the distal tip of the femoral catheter was not confirmed. Nonetheless, the length of catheter for the femoral artery was 4.45cm; therefore, it can be assumed that in smaller patients, the distal tip would be located in the descending aorta, and in larger patients, it might be located in the descending aorta or in the bifurcation of iliac arteries. While femoral arterial pressure represents central aortic pressure more accurately, there have been some reports of complications caused by femoral arterial catheterization. Several studies have indicated a complication rate of 2.4–25.0% associated with femoral arterial catheterization in neonates and infants. Dumond et al.13 reported that the incidence of pedal pulse loss, distal to the catheter, in neonates and infants, was related to the size of the catheter and duration of use. Longer duration or larger size was directly related to perfusion-related complications from femoral arterial catheterization. In the present study, only transient and minor complications were observed, such as small hematomas and local erythema; no major complications such as limb ischemia associated with femoral arterial cannulation were observed. However, further prospective studies using serial ultrasonography are now needed to fully determine the safety of femoral arterial cannulation. Moreover, aseptic maneuvers should be performed by an experienced physician, and it is essential to carefully monitor the insertion site and limb color distal to the site of catheterization.
This study was limited by its retrospective study design, and by the fact that this was a single institutional study with a small sample size in patients with a variety of congenital heart diseases. In the ICU, BP was measured hourly, which does not always represent the pattern of BP during the entire hour. Furthermore, no objective diagnostic method such as ultrasound was used to assess complications. In the authors’ experience, the number of both radial and femoral attempts increases in sicker and smaller children. It could therefore be theorized that the increased number of radial attempts in sicker (longer bypass) and younger children could traumatize the artery and thus contribute to the lower readings obtained. Further studies are needed to investigate the number of cannulation attempts and the associated pressure differences.
The authors conclude that, in our this study population, radial arterial pressure was usually underestimated compared to femoral arterial pressure after the initiation of CPB, and that the differences between radial and femoral arterial pressure were more marked in patients with longer CPB time. It was also observed that these pressure differences were not apparent during the ICU period.
FundingThis study was supported by a grant (CRI 11083-33) from the Chonnam National University Hospital Biomedical Research Institute and by a grant (NRF-2016R1D1A1A02937493, NRF-2015R1C1A1A02037778 and NRF-2016R1D1A3B03935986) through the Ministry of Education of the Republic of Korea and National Research Foundation of Korea.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Cho HJ, Lee SH, Jeong IS, Yoon NS, Ma JS, Ahn BH. Differences in perioperative femoral and radial arterial blood pressure in neonates and infants undergoing cardiac surgery requiring cardiopulmonary bypass. J Pediatr (Rio J). 2018;94:76–81.