To estimate the coverage of the National Vitamin A Supplementation Program (Programa Nacional de Suplementação de Vitamina A) in children from Alagoas, to identify factors associated with this coverage, and to analyze the adequacy of nutrition education actions.
MethodsHousehold survey involving a representative probabilistic sample of children aged 6 to 59 months from Alagoas and their mothers (n=509). Coverage was defined by the percentage of children with supplementation records in the last semester. The association between the independent variables (socioeconomic, demographic, and health) and the National Vitamin A Supplementation Program coverage was analyzed based on the prevalence ratio and its 95% CI. The mothers’ knowledge of questions related to vitamin A was considered as an indicator of the adequacy of nutrition education actions.
ResultsProgram coverage was 91.9% in children aged 6-11.9 months and 38.6% in children aged 12-59 months. In the adjusted analysis, the factors that were associated with greater coverage were: age between 6-11.9 months (PR=2.50, 95% CI: 2.10-2.96), living in rural areas (PR=1.45, 95% CI: 1.20-1.76) and living in a house with ≤ 4 rooms (PR=1.33, 95% CI: 1.09-1.63). Only 26.1% of the mothers were able to mention some food source of vitamin A and only 19.2% were aware of the consequences of vitamin deficiency for health.
ConclusionsThe National Vitamin A Supplementation Program coverage is below the targets set by the Ministry of Health (except for children <12 months). The factors associated with greater coverage indicate an adequate focus of the program. The nutrition education activities have not demonstrated satisfactory results. This information should guide actions to improve the program.
Estimar a cobertura do Programa Nacional de Suplementação de Vitamina A em crianças de Alagoas, identificar fatores associados a essa cobertura e analisar a adequação das ações das ações de educação nutricional.
MétodosInquérito domiciliar que envolveu amostra probabilística representativa das crianças de 6 a 59 meses de Alagoas e suas mães (n=509). A cobertura foi definida pelo percentual de crianças com registro de suplementação no último semestre. A associação entre as variáveis independentes (socioeconômicas, demográficas e de saúde) e a cobertura do Programa Nacional de Suplementação de Vitamina A foi analisada com base na razão de prevalência e seu IC95%. O conhecimento das mães sobre questões relacionadas à vitamina A foi assumido como indicador da adequação das ações de educação nutricional.
ResultadosA cobertura do programa foi de 91,9% entre crianças de 6-11,9 meses e de 38,6% entre as de 12-59 meses. Na análise ajustada, os fatores que se associaram à maior cobertura foram ter idade entre 6-11,9 meses (RP=2,50; IC95%: 2,10-2,96), residir em zona rural (RP=1,45; IC95%: 1,20-1,76) e morar em domicílio com ≤ 4 cômodos (RP=1,33; IC95%: 1,09-1,63). Somente 26,1% das mães souberam citar algum alimento fonte de vitamina A e apenas 19,2% conheciam as consequências da deficiência dessa vitamina para a saúde.
ConclusõesA cobertura do Programa Nacional de Suplementação de Vitamina A encontra-se aquém das metas estabelecidas pelo Ministério da Saúde (exceto para crianças <12 meses). Os fatores associados à maior cobertura evidenciam adequada focalização do programa. As atividades de educação nutricional não ocorrem de forma satisfatória. Essas informações devem nortear ações de aperfeiçoamento do programa.
Vitamin A is an essential micronutrient in several physiological processes in the human body, being necessary for the adequate functioning of the immune system, visual acuity, cell proliferation/differentiation, and gene expression.1–4 Despite universal susceptibility, its deficiency is more frequent in children under five years, pregnant women, and lactating women, which is why these groups are considered biologically more vulnerable to this nutritional deficiency.5
Vitamin A deficiency (VAD) is a major public health problem in low- and middle-income countries, affecting 190 million children.6 In 2013, 29% of the children in these countries had VAD. In the same year, 94,500 deaths from diarrhea and 11,200 deaths from measles were attributed to VAD.7 In Brazil, data from a national survey carried out in 2006 showed a prevalence of 17.4% in children under 5 years of age, with this prevalence being 19.0% in the northeast of the country.8
The main consequences of VAD are blindness and immune system impairment, contributing to an increase in the prevalence of diarrheal and infectious diseases, mortality rate, and demand for health services.9 Additionally, due to its participation in several metabolic processes, VAD has been associated with other disorders, such as anemia.10
In 2005, the National Vitamin A Supplementation Program (Programa Nacional de Suplementação de Vitamina A [PNVITA]) was implemented in Brazil with the aim of reducing the prevalence of hypovitaminosis A in the most susceptible individuals, such as children aged 6 to 59 months. The program main action consists of bi-yearly supplementation with vitamin A megadoses. In parallel, nutrition education (NE) actions are recommended to improve vitamin A intake through food consumption.9,10 However, no strategies related to program evaluation activities have been defined, which is why, perhaps, there are so few works in the literature1,11–13 that address this issue.
Even though PNVITA has been in operation since 2005, subsequent studies have found high prevalence rates of VAD.14,15 In the state of Alagoas, located in the semi-arid region of Brazil, there was a prevalence of 45.4% in preschool children in 2007, which suggests the existence of problems in the program's performance.15 Identifying these problems is of great relevance for the evaluation and reorganization of PNVITA actions.
The aim of this study was to estimate the PNVITA coverage in children from Alagoas, identify factors associated with this coverage, and analyze the adequacy of the nutrition education actions.
MethodsSampling plan and data collectionThis was a cross-sectional study of data from a survey called “II Health Diagnosis of the Maternal-Child Population of the State of Alagoas,” in which the variable of interest used in sample size calculation was food insecurity in Alagoas, estimated at 34.7%. The other parameters were: population of 841,117 families, sampling error of 2.0%, 120 conglomerates (census sectors), and 1.5 for correction of the complex design effect. Thus, for a 95% CI and after including 10% to cover possible sample losses, 3,696 families were required. A detailed description of this procedure is available elsewhere.16
For the present study, all children aged 6 to 59 months residing in the randomly selected households were eligible, totaling 509 children. Considering this sample was not initially planned, the sampling error was calculated subsequently, using the StatCalc module of the EpiInfo software (Epi Info™, a database and statistics program for public health professionals. CDC, Atlanta, GA, USA, 2011). Based on the coverage rates identified in this study, the analyzed sample number allowed for estimation of the coverage with errors ranging from 2.3% (6-59 months) to 4.2% (12-59 months), depending on the age group considered.
The fieldwork was carried out by a properly trained and supervised team, from January 2014 to January 2015, through home visits, using structured forms pre-tested in a pilot study carried out in the municipality of Maceió in a low-income neighborhood, which was not part of the census sectors randomly selected for the survey. The tools were prepared by the researchers using the PNVITA Manual of Standards17 as a reference and critically evaluated by the team after the pilot study.
The study included the children whose mothers agreed to provide information after consenting to participate and signing the informed consent, according to the terms of the project approved by the Research Ethics Committee of Universidade Federal de Alagoas (process No. 09093012.0.0000.5013).
According to Donabedian,18 the evaluation of a program's effectiveness can be performed by analyzing its structure, its processes, and the achieved results. Aspects related to the program structure were not assessed in this study. The coverage attained by the program was investigated as a process indicator, i.e., the proportion of the target population that received vitamin A supplementation according to PNVITA recommendations. Regarding the analysis of the results, the mothers’ level of knowledge about basic information on adequate nutrition was considered, especially those related to the program focus: hypovitaminosis A prevention. The adequacy of this knowledge was assumed as an outcome indicator related to NE activities.
To define the coverage rate, the proportion of children from the target population who had a record of vitamin A supplementation over the past six months was considered, which is specified in the Program Manual for supplementation.17 This information was obtained by consulting the respective children's “health booklets.”
To analyze the adequacy of the NE actions, the mothers answered questions on aspects they should know about, if they had participated in nutrition education activities included in the program, considering that the “Promotion of adequate and healthy nutrition, ensuring information to encourage the consumption of foods that are sources of vitamin A by the population” is part of the PNVITA Manual activities,17 as one of the most important measures for VAD prevention. Aiming to avoid information bias, only the mothers (biological or not) were included in the study.
The question about foods that are rich in vitamin A was presented openly and the interviewee could mention up to three foods. To classify the adequacy of the responses, the PNVITA Manual of Activities17 was used as reference, which includes the following:
“Vitamin A is a micronutrient found in animal (retinol) and vegetable (provitamin A) food sources. Among the foods of animal origin, the main sources are: human milk, liver, egg yolk, and milk. Provitamin A is found in green leafy vegetables (such as spinach, kale, purslane, Indian spinach, and mustard greens), yellow vegetables (such as pumpkin and carrots) and yellow-orange fruits (such as mango, cashew fruit, guava, papaya, and persimmon) in addition to oils and oleaginous fruits (buriti fruit oil, pupunha palm, dende palm oil, and souari nut) which are the richest sources of provitamin A”.17
Socioeconomic, demographic and health assessmentQuestions were obtained that were related to demographics (area of residence, child's gender and age, number of residents per household, maternal age), socioeconomic factors (maternal level of schooling, per capita monthly family income, number of durable consumer goods, number of rooms in the household, number of rooms used for sleeping, source of the water used for drinking, family enrolled in the government's income transfer program) and health-related factors (whether the child had had diarrhea in the previous 15 days).
Data analysisThe collected data were entered in duplicate in a form created using the Epi Info 3.5.4 software and, after reviewing possible typing errors, the statistical analyses were carried out using Stata software (SPSS for Windows, version 12.0. Chicago, USA). Categorical variables were compared based on Pearson's chi-squared test (χ2). The prevalence of coverage (dependent variable) according to the different categories of independent variables was compared based on the prevalence ratio (PR) and its 95% confidence interval (95% CI). The independent variables of which crude PRs indicated association with coverage with a degree of significance of up to 20% (p <0.2) were submitted to the multivariate analysis, gradually excluding those variables with no statistical significance (backward elimination). The final model included only the variables that reached the significance level of p <0.05. The PRs and their respective 95% CIs, both in the crude and adjusted analyses, were calculated by Poisson regression with robust variance adjustment. In all situations, the statistical significance was set at p <0.05.
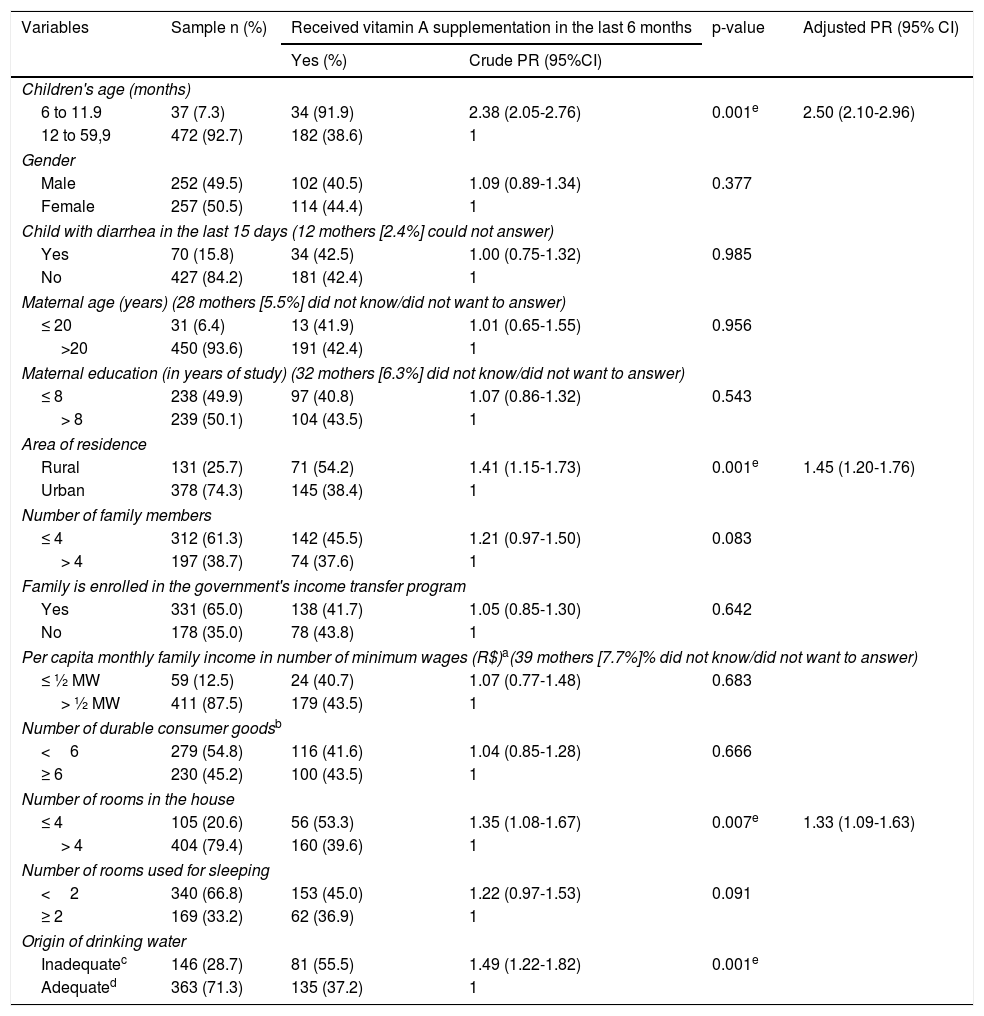
ResultsThe analyzed sample consisted of 509 children/mothers. Most of them (74.3%) lived in urban areas, 6.4% of the mothers were adolescents, 28.7% had no access to adequate drinking water, and 12.5% of the families had a per capita monthly family income ≤ ½ minimum wage (the minimum wage was R$ 724.00, or approximately US$ 272, at the time of the study). Approximately 2/3 of the families participated in the Bolsa Família Program, the Brazilian government income transfer program. These and other characteristics are shown in Table 1, which shows that the incidence of diarrhea in the children was 15.8%. Regarding this aspect, there was no difference between children supplemented and not supplemented with vitamin A.
Demographic, socioeconomic, and health characteristics of children aged 6 to 59 months, according to access to vitamin A megadose supplementation in the last six months. Alagoas, Brazil, 2015.
| Variables | Sample n (%) | Received vitamin A supplementation in the last 6 months | p-value | Adjusted PR (95% CI) | |
|---|---|---|---|---|---|
| Yes (%) | Crude PR (95%CI) | ||||
| Children's age (months) | |||||
| 6 to 11.9 | 37 (7.3) | 34 (91.9) | 2.38 (2.05-2.76) | 0.001e | 2.50 (2.10-2.96) |
| 12 to 59,9 | 472 (92.7) | 182 (38.6) | 1 | ||
| Gender | |||||
| Male | 252 (49.5) | 102 (40.5) | 1.09 (0.89-1.34) | 0.377 | |
| Female | 257 (50.5) | 114 (44.4) | 1 | ||
| Child with diarrhea in the last 15 days (12 mothers [2.4%] could not answer) | |||||
| Yes | 70 (15.8) | 34 (42.5) | 1.00 (0.75-1.32) | 0.985 | |
| No | 427 (84.2) | 181 (42.4) | 1 | ||
| Maternal age (years) (28 mothers [5.5%] did not know/did not want to answer) | |||||
| ≤ 20 | 31 (6.4) | 13 (41.9) | 1.01 (0.65-1.55) | 0.956 | |
| >20 | 450 (93.6) | 191 (42.4) | 1 | ||
| Maternal education (in years of study) (32 mothers [6.3%] did not know/did not want to answer) | |||||
| ≤ 8 | 238 (49.9) | 97 (40.8) | 1.07 (0.86-1.32) | 0.543 | |
| > 8 | 239 (50.1) | 104 (43.5) | 1 | ||
| Area of residence | |||||
| Rural | 131 (25.7) | 71 (54.2) | 1.41 (1.15-1.73) | 0.001e | 1.45 (1.20-1.76) |
| Urban | 378 (74.3) | 145 (38.4) | 1 | ||
| Number of family members | |||||
| ≤ 4 | 312 (61.3) | 142 (45.5) | 1.21 (0.97-1.50) | 0.083 | |
| > 4 | 197 (38.7) | 74 (37.6) | 1 | ||
| Family is enrolled in the government's income transfer program | |||||
| Yes | 331 (65.0) | 138 (41.7) | 1.05 (0.85-1.30) | 0.642 | |
| No | 178 (35.0) | 78 (43.8) | 1 | ||
| Per capita monthly family income in number of minimum wages (R$)a(39 mothers [7.7%]% did not know/did not want to answer) | |||||
| ≤ ½ MW | 59 (12.5) | 24 (40.7) | 1.07 (0.77-1.48) | 0.683 | |
| > ½ MW | 411 (87.5) | 179 (43.5) | 1 | ||
| Number of durable consumer goodsb | |||||
| <6 | 279 (54.8) | 116 (41.6) | 1.04 (0.85-1.28) | 0.666 | |
| ≥ 6 | 230 (45.2) | 100 (43.5) | 1 | ||
| Number of rooms in the house | |||||
| ≤ 4 | 105 (20.6) | 56 (53.3) | 1.35 (1.08-1.67) | 0.007e | 1.33 (1.09-1.63) |
| > 4 | 404 (79.4) | 160 (39.6) | 1 | ||
| Number of rooms used for sleeping | |||||
| <2 | 340 (66.8) | 153 (45.0) | 1.22 (0.97-1.53) | 0.091 | |
| ≥ 2 | 169 (33.2) | 62 (36.9) | 1 | ||
| Origin of drinking water | |||||
| Inadequatec | 146 (28.7) | 81 (55.5) | 1.49 (1.22-1.82) | 0.001e | |
| Adequated | 363 (71.3) | 135 (37.2) | 1 | ||
Of the 509 assessed children, it was observed that 216 of them had a record of vitamin A supplementation at some time in the previous six months, corresponding to a coverage of 42.4%.
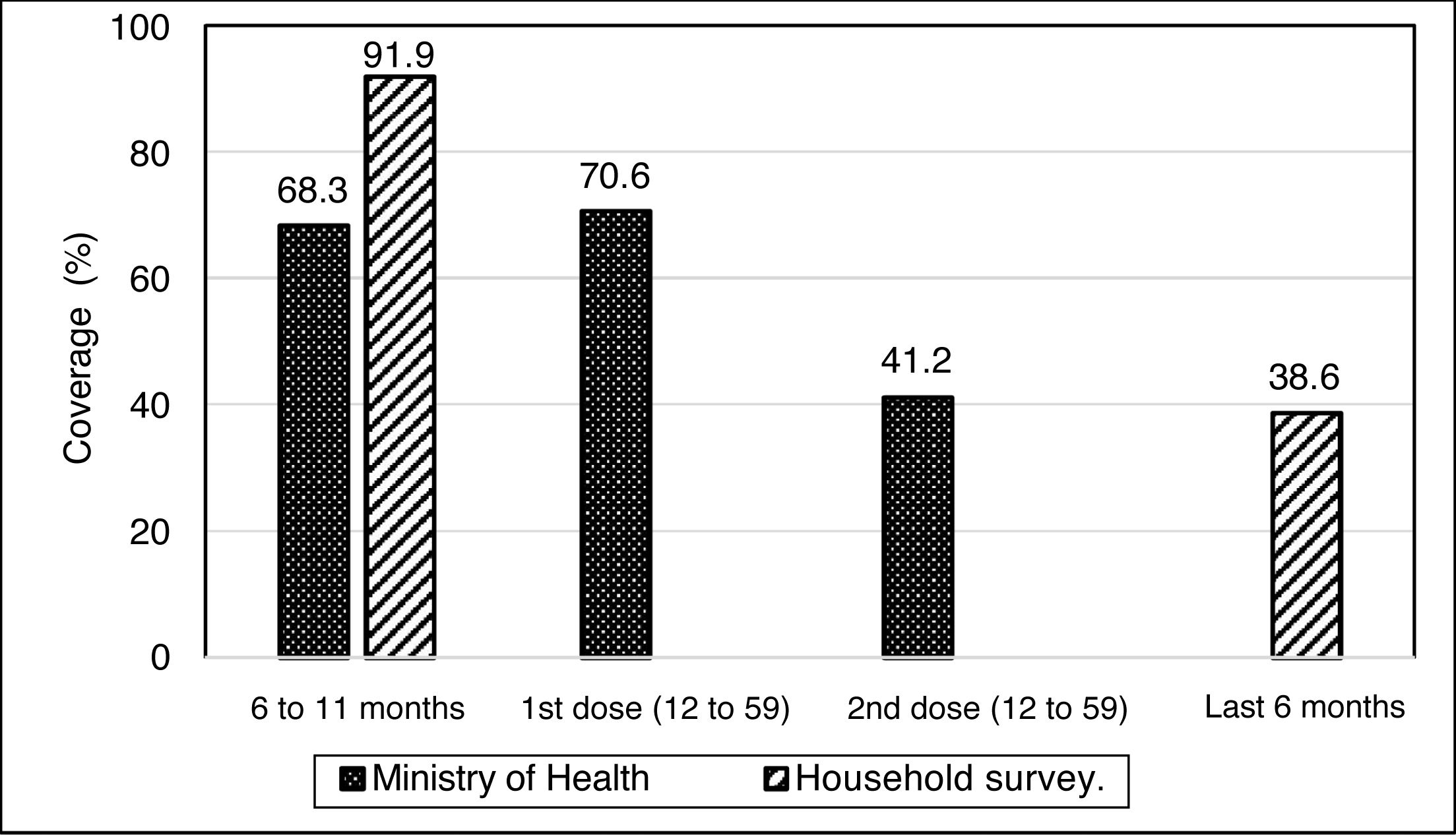
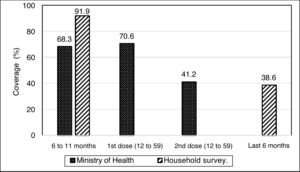
Considering the age groups with supplementation recommendation by PNVITA, it was verified that the percentage of coverage by the program in children aged 6 to 11.9 months was 91.9%, whereas it was 38.6% in those aged 12 to 59 months of age (Table 1). Fig. 1 shows the coverage verified through the present investigation in relation to the results published for the year 2014 by the Ministry of Health (MoH).19
National Vitamin A Supplementation Program coverage in the state of Alagoas, Brazil, in 2014, according to data from the Ministry of Health and a household survey involving children aged 6 to 59 months.
Source: Ministry of Health (Brazil, 2014); Household survey.
The results obtained through the household survey in the state of Alagoas for the age group of 12 to 59 months were obtained using a different method from those published by the Ministry of Health. The latter considered the coverage in relation to the accomplishment of a 1st and 2nd doses of vitamin A supplementation. In the household survey, coverage was defined according to the supplementation record in the child's “health booklet” dated up to six months before the interview.
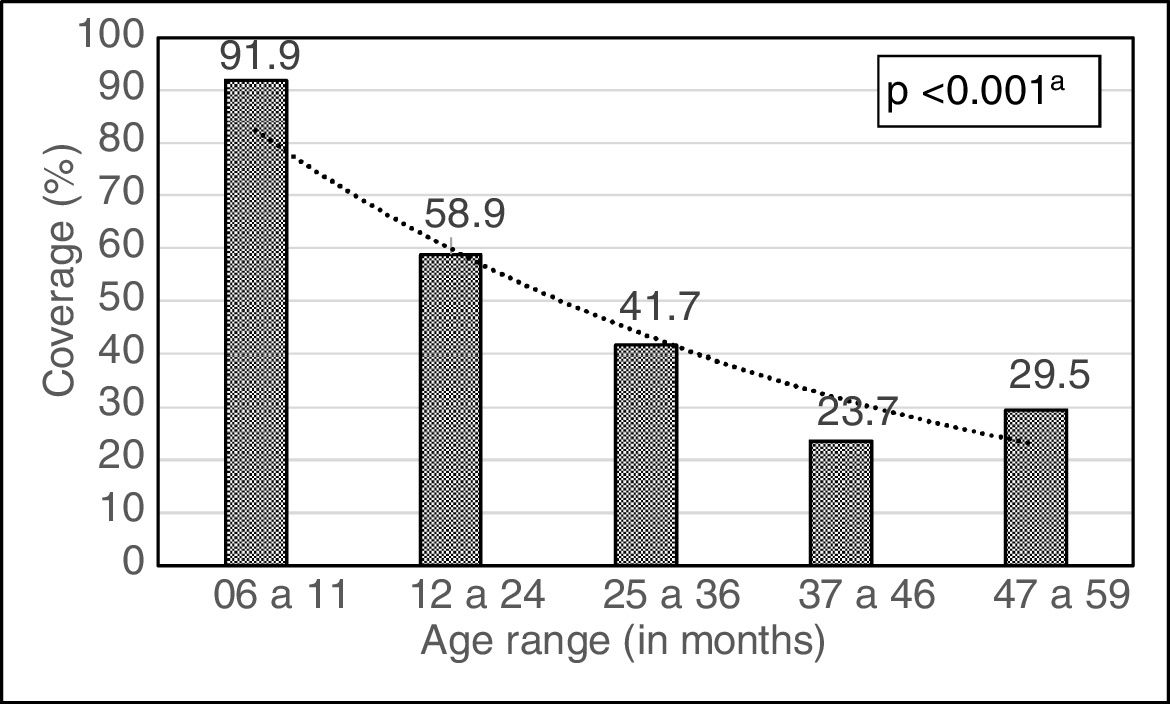
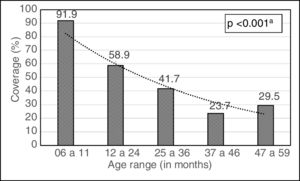
By further stratifying the age groups, it was possible to observe a steady decline in the coverage rate of the program as the children grew older; the coverage rate in the younger children was 91.9%, whereas it was 29.5% in those aged 47-59 months (Fig. 2).
The factors that were independently associated, contributing to a greater coverage of PNVITA were between age range between 6 and 11.9 months (PR=2.50, 95% CI: 2.10-2.96), living in rural areas (PR=1.45, 95% CI: 1.20-1.76) and living in a household with four or fewer rooms (PR=1.33, 95% CI: 1.09-1.63), as shown in Table 1.
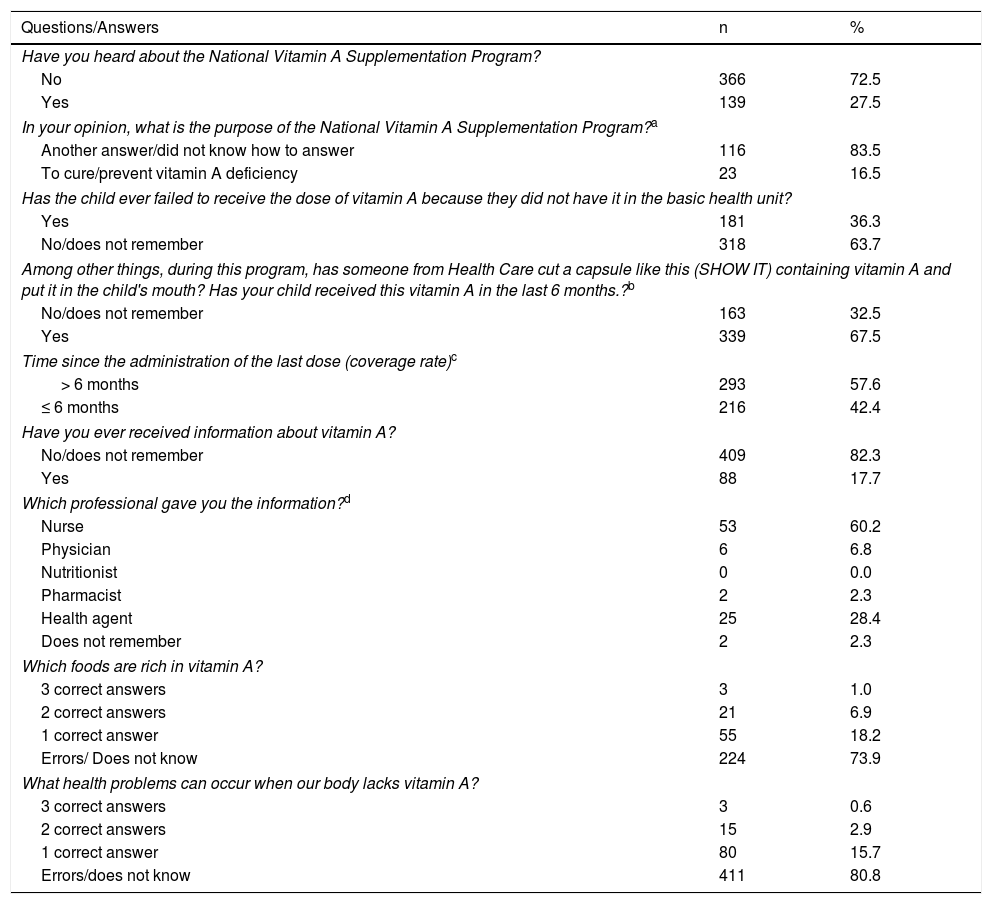
Table 2 shows the results related to the PNVITA questions applied to the mothers. Only 27.5% had heard about the program, and even so, only 16.5% of them knew about its purpose (curing or preventing vitamin A deficiency). When asked if they had ever received information about vitamin A, 88 of the 509 respondents answered affirmatively (17.7%). In this case, the nurse was the professional responsible for providing information in 60.2% of cases.
Frequency of responses given by mothers of children aged 6 to 59 months to questions related to the National Vitamin A Supplementation Program. Alagoas, Brazil, 2015.
| Questions/Answers | n | % |
|---|---|---|
| Have you heard about the National Vitamin A Supplementation Program? | ||
| No | 366 | 72.5 |
| Yes | 139 | 27.5 |
| In your opinion, what is the purpose of the National Vitamin A Supplementation Program?a | ||
| Another answer/did not know how to answer | 116 | 83.5 |
| To cure/prevent vitamin A deficiency | 23 | 16.5 |
| Has the child ever failed to receive the dose of vitamin A because they did not have it in the basic health unit? | ||
| Yes | 181 | 36.3 |
| No/does not remember | 318 | 63.7 |
| Among other things, during this program, has someone from Health Care cut a capsule like this (SHOW IT) containing vitamin A and put it in the child's mouth? Has your child received this vitamin A in the last 6 months.?b | ||
| No/does not remember | 163 | 32.5 |
| Yes | 339 | 67.5 |
| Time since the administration of the last dose (coverage rate)c | ||
| > 6 months | 293 | 57.6 |
| ≤ 6 months | 216 | 42.4 |
| Have you ever received information about vitamin A? | ||
| No/does not remember | 409 | 82.3 |
| Yes | 88 | 17.7 |
| Which professional gave you the information?d | ||
| Nurse | 53 | 60.2 |
| Physician | 6 | 6.8 |
| Nutritionist | 0 | 0.0 |
| Pharmacist | 2 | 2.3 |
| Health agent | 25 | 28.4 |
| Does not remember | 2 | 2.3 |
| Which foods are rich in vitamin A? | ||
| 3 correct answers | 3 | 1.0 |
| 2 correct answers | 21 | 6.9 |
| 1 correct answer | 55 | 18.2 |
| Errors/ Does not know | 224 | 73.9 |
| What health problems can occur when our body lacks vitamin A? | ||
| 3 correct answers | 3 | 0.6 |
| 2 correct answers | 15 | 2.9 |
| 1 correct answer | 80 | 15.7 |
| Errors/does not know | 411 | 80.8 |
Some mothers did not want to answer questions 1, 3, 4, 6 and 8, which is why the respective percentages were calculated considering only the total answers obtained. The non-response frequencies for these questions were, respectively: 0.8% (n=4); 2.0% (n=10); 1.4% (n=7); 2.4% (n=12); 40.5% (n=206).
It was verified that only 18.2% of the interviewees mentioned at least one vitamin A food source, whether of animal or vegetable origin,17 and that 80.8% of them did not know of any health problems caused by VAD.
DiscussionThe goal of PNVITA is to reach 75% coverage for children aged 6 to 11 months and 100% for the first dose and 60% for the second dose in children aged 12 to 59 months.20 Regarding this aspect, the results showed that the program exceeds the goal of coverage in the case of the younger children (91.9%), but falls short regarding children aged 12 months or older (38.6%). In this age group, the program recommends supplementation every six months.17,21 Thus, a child that received 100% of the doses according to this recommendation, considering the period comprised between 12 and 60 months, should have received eight doses. Therefore, this study adopted the record of supplementation that occurred in the previous six months as the criterion for defining coverage. Regardless of this methodological divergence, the coverage found herein for most of the assessed children demonstrates the need for investments aiming to improve the program's reach.
As for the criterion used by the Ministry of Health when considering the accomplishment of a 1st and 2nd dose, it appears inconsistent, as the Ministry itself determines that:17“Vitamin A supplementation should be offered to children aged 12 to 59 months of age every six months.” This recommendation is based on the assumption that megadoses are sufficient to ensure a good hepatic retinol reserve for approximately six months, at which time further supplementation should occur. Therefore, the appropriate program implementation should ensure that each child has a recorded supplementation that occurred at most six months before. Thus, the comparison with the MoH data is impaired.
Nevertheless, the coverage reported herein for the assessed age group (38.6%) was lower compared to that reported by the MoH: 70.6% and 41.2%, respectively, for the 1st and 2nd doses. Considering that this “1st dose” may have occurred long ago (its benefits would no longer be effective) and that the “2nd dose” is more likely to have been given more recently, which is closer to the criterion used in this article, it can be observed that the obtained values are very similar: 38.6% and 41.2%.
The adequate coverage observed in children aged 6 to 11 months could result from their more frequent contact with the health care services. This age group comprises the target population of several actions implemented in basic health units, such as childcare consultations and visits to comply with the vaccination schedule.22
As in the present investigation, Almeida et al.,12 in a study carried out in the municipality of Cabedelo (state of Paraíba, Brazil), also found greater PNVITA coverage in younger children and a declining trend with increasing age (stratified by semesters). The adequate coverage achieved in younger children is a very interesting aspect, as it provides vitamin A protection precisely to one of the groups biologically more vulnerable to morbimortality due to infections.9
Therefore, despite the excellent coverage observed in the age group of 6 to 11 months, the low coverage observed in children older than 12 months is a matter of concern, which suggests failures in the program's operation. According to Paiva,13 a strategy to increase coverage would be to improve the maternal level of information about the program and reinforce actions to increase adherence to scheduled health service visits. Additionally, the active search strategy is an alternative to achieve coverage goals in this age group, since, unlike younger children, those older than 12 months are generally less involved in routine visits to the health services.
No studies were found on the economic impact of the active search strategy. However, the Ministry of Health itself indicates it as a way to increase program coverage, as it can be incorporated into the routine of the family health teams and allows adjustments in the regularity of supplementation and the NE actions.11,12,17
The present study identified greater coverage of the program in the rural area, a situation that may be related to the more active search of health agents in these areas.12 There is a greater proportion of households registered in the family health units in rural areas in Brazil.23
Another variable that was associated with greater coverage of the PNVITA was living in a household with up to four rooms, a condition that may reflect unfavorable socioeconomic characteristics of the family and, therefore, would receive greater attention from health professionals. The adverse effect of living in a poor household can be mitigated when individuals receive more attention from the public authorities.24
The variables that were associated with the greater coverage of the PNVITA suggest the adequate focus of the program: children in the most biologically vulnerable age group, living in rural areas, who belong to families with unfavorable socioeconomic characteristics. Incidentally, unfavorable socioeconomic characteristics can interfere in the choice of foods consumed by the families, either due to their purchasing power or as a consequence of the maternal knowledge about adequate foods. Therefore, these children would be more susceptible to an inadequate intake of dietary vitamin A.25
It is part of the regulation that created the PNVITA that, during its operationalization, NE activities should be reinforced, with emphasis on healthy eating promotion.21 To support these activities, several materials are produced (leaflets, posters) containing information about the program, VAD and its consequences, and food sources high in vitamin A. If these resources are reaching the target audience and if the information is being transmitted, regardless of the strategies used (individual guidance, group meetings, lectures, dramatizations, videos), the mothers should recognize the existence of PNVITA and what its purpose is. However, only 27.5% of them reported having heard of the program, and of these, only 16.5% knew how to correctly answer about its purpose. Most of them reported having watched the administration of vitamin A to the child; however, they were unaware of its connection with the PNVITA. Considering these data and comparing them with the coverage rate observed herein, it is evident that the supplementation activity occurs while dissociated from educational guidelines, which, in addition to being outside the scope of the program, does not provide sustainability to the process, since without an adequate diet, the risk of VAD will always exist and, consequently, the need to maintain supplementation activities.
In support of these considerations is the fact that only 17.7% of the mothers answered that they had received information about vitamin A, 73.9% did not know any foods rich in vitamin A, and 80.8% did not know at least one consequence of vitamin A deficiency. Similar results were found in a sample of 2,546 children from municipalities located in the state of Bahia, Brazil,1 where 74.6% of the mothers had no knowledge about vitamin A. While studying children from a municipality located in northeastern Brazil, Almeida et al.12 observed that only 43.5% of the mothers had heard about PNVITA; however, of these, 86.2% did not know about the program's activities. Moreover, only 22.2% provided a correct answer about some function of vitamin A, and among those who claimed to know the food sources of retinol (40.7%), only 33.4% correctly mentioned some food with this characteristic. Considering these findings, they stated that the lack of knowledge related to vitamin A may interfere with adherence to PNVITA actions, making it difficult to achieve the established goals.
The nutritionist is the health professional whose work aims to provide dietary care at the individual or collective level.26 However, of the mothers who answered they received some information on vitamin A, none of them reported this information was provided by a nutritionist. In this scenario, in 60.2% of the cases, it was the nurse who provided such information. A study including professionals involved in the program operationalization in nine municipalities located in the state of Paraíba identified a low participation of nurses in NE activities, with health agents being the main performers of this activity.13
Marques et al.11 used a qualitative approach to identify practices related to PNVITA and disclose maternal social representations about vitamin A, its deficiency, and the program in a municipality located in Vale do Jequitinhonha. It was observed that supplementation has occurred in association with vaccination actions, which may favor an increase in supplementation coverage, but also may result in a passive participation in PNVITA, both by the target population and by the professionals, considering that supplementation is carried out as a secondary action to vaccination and is unaccompanied by an educational process, leading to the formation of distorted ideas, such as that vitamin A is a vaccine.
The misinformation contributes to bad choices regarding the individuals’ selection of foods. Graebner et al.,27 when investigating children from rural areas of the Federal District, found that, even when they had access to food sources of carotenoids, children had a high prevalence of VAD, which would not occur if these foods were regularly consumed.
Rodrigues and Roncada28 have stated that, since its implementation, PNVITA's main emphasis is on the distribution of vitamin A megadoses and that nutrition education activities are far behind the expected due to the lack of skilled human resources and the lack of effective implementation strategies. They believe that as the NE actions develop and are consolidated as part of an intersectoral public health promotion policy, there will be an evolution of the proposed contents and methodologies, which will be incorporated into its practice, promoting healthy eating and preventing not only diseases such as VAD, but also chronic noncommunicable diseases.
The results obtained allow us to conclude that the PNVITA coverage in children aged 12-59 months is below the established goals. However, the factors associated to greater coverage indicate an adequate focus regarding the target population. The NE activities have not demonstrated satisfactory results, jeopardizing the program's effectiveness. This information should guide health managers and professionals when planning improvement actions for the program.
FundingThis study received financial support from the Brazilian Conselho Nacional de Desenvolvimento Científico e Tecnológico – (National Council for Scientific and Technological Development - CNPq) (process No. 474381 / 2011-0) and the Fundação de Amparo à Pesquisa of the state of Alagoas (Alagoas Research Support Foundation– FAPEAL) under process No. 60030.000716/2013.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Lima RB, Ferreira HS, Cavalcante AL, Santos LG, Vieira RC, Assunção ML. Coverage and educational actions related to the national vitamin A supplementation program: a study in children from the state of Alagoas. J Pediatr (Rio J). 2020;96:184–92.
Study conducted at Universidade Federal de Alagoas (UFAL), Faculdade de Nutrição, Maceió, AL, Brazil.
Article based on Riquelane Bezerra Menezes Lima's Master's Degree Dissertation, from the Postgraduate Program in Nutrition, Universidade Federal de Alagoas, Maceió, AL, Brasil.