Management of patent ductus arteriosus is still controversial. This study aimed to describe the impact of a more conservative approach on treatment rates and on main outcomes of prematurity, especially in preterm infants with <26 weeks of gestation.
MethodClinical charts review of infants ≤30 weeks with patent ductus arteriosus between 2009 and 2016 at two centers. In 2011, the authors changed patent ductus arteriosus management: in first period (2009–2011), patients who failed medical treatment underwent surgical closure; in second period (2012–2016), only those with cardiopulmonary compromise underwent surgical ligation. Medical treatment, surgical closure, mortality, and survival-without-morbidity were compared.
ResultsThis study included 188 patients (27±2 weeks, 973±272 grams); 63 in P1 and 125 in P2. In P2, significantly lower rates of medical treatment (85.7% P1 versus 56% P2, p<0.001) and surgical closure (34.5% P1 versus 16.1% P2, p<0.001) were observed. No differences were found in chronic lung disease (28.8% versus 13.9%, p=0.056), severe retinopathy of prematurity (7.5% versus 11.8%, p=0.403), necrotizing enterocolitis (15.5% versus 6.9%, p=0.071), severe intraventricular hemorrhage (25.4% versus 18.4%, p=0.264), mortality (17.5% versus 15.2%, p=0.690) or survival-without-morbidity adjusted OR=1.10 (95% CI: 0.55–2.22); p=0.783. In P2, 24.5% patients were discharged with patent ductus arteriosus. The subgroup born between 23 and 26 weeks (n=82) showed significant differences: lower incidence of chronic lung disease (50% versus 19.6%, p=0.019) and more survival-without-morbidity (20% versus 45.6%, p=0.028) were found.
ConclusionA conservative approach in preterm infants with patent ductus arteriosus can avoid medical and surgical treatments, without a significant impact in survival-without-morbidity. However, two-thirds of preterm infants under 26 weeks are still treated.
O tratamento da persistência do canal arterial ainda é controverso. Nosso objetivo foi descrever o impacto de uma abordagem mais conservadora em nossas taxas de tratamento e nos principais desfechos da prematuridade, especialmente em prematuros com<26 semanas de gestação.
MétodoRevisão de prontuários de lactentes com≤30 semanas e persistência do canal arterial entre 2009-2016 em dois centros. Em 2011, mudamos o manejo da persistência do canal arterial: no primeiro período (2009-2011), os pacientes que não apresentaram sucesso com o tratamento clínico foram submetidos a fechamento cirúrgico; no segundo período (2012-2016), apenas aqueles com comprometimento cardiopulmonar foram submetidos ao fechamento cirúrgico. Comparamos o tratamento clínico, fechamento cirúrgico, mortalidade e sobrevida sem morbidade.
ResultadosForam incluídos 188 pacientes (27±2 semanas, 973±272 gramas); 63 em P1 e 125 em P2. Em P2, foram observadas taxas significativamente mais baixas de tratamento clínico (85,7% no P1 versus 56% no P2, p<0,001) e fechamento cirúrgico (34,5% no P1 versus 16,1% no P2, p<0,001). Não foram encontradas diferenças em relação à doença pulmonar crônica (28,8% versus 13,9%, p=0,056), retinopatia grave da prematuridade (7,5% versus 11,8%, p=0,403), enterocolite necrosante (15,5% versus 6,9%, p=0,071), hemorragia intraventricular grave (25,4% versus 18,4%, p=0,264), mortalidade (17,5% versus 15,2%, p=0,690) ou OR ajustado pela sobrevida sem morbidade=1,10 (IC95%: 0,55-2,22); p=0,783. Em P2, 24,5% dos pacientes receberam alta com persistência do canal arterial. O subgrupo nascido entre 23 a 26 semanas (n=82) apresentou diferenças significativas, foram encontradas menor incidência de doença pulmonar crônica (50% versus 19,6%, p=0,019) e maior sobrevida sem morbidade (20% versus 45,6%, p=0,028).
ConclusãoUma abordagem conservadora em prematuros com persistência do canal arterial pode evitar tratamentos clínicos e cirúrgicos, sem um impacto significativo na sobrevida sem morbidade. No entanto, dois terços dos prematuros com menos de 26 semanas ainda são tratados.
Ductus arteriosus closure is frequently delayed in preterm infants, with an estimated incidence of patency in gestational ages below 30 weeks of up to 60%.1 The probability of patency is inversely proportional to the gestational age of the neonate.2 Although patency of ductus arteriosus (PDA) has historically been associated with increased morbidity and mortality in premature newborns,3 the cause–effect relationship between these unfavorable conditions has not been well established. PDA may merely be an intermediate stage among the hemodynamic changes taking place in the first weeks of life of the preterm infant.4
In recent decades many preterm infants have been treated either prophylactically or actively, with cyclooxygenase inhibitors or with surgical ligation. Therefore, the real significance of PDA and its natural evolution are difficult to determine. Conservative management of PDA has become increasingly common for preterm infants,5 but there is still controversy regarding evaluation and management of PDA, resulting in substantial heterogeneity in clinical practice.6,7 The main reasons for this approach are that PDA treatments are related to side effects and that almost 30% of preterm infants born at <1000g achieve spontaneous ductus closure in the first week of life.2 Moreover, the long-term improvement associated with treated PDA has yet to be proven.6 It is uncertain whether a more conservative approach can affect premature infants in the long term, and especially those born between 23 and 26 weeks of gestation. Taking into account these facts, in 2011 the authors adopted a more conservative approach to PDA.
This study was designed to evaluate the differences in treatment received and outcomes of prematurity because of a change in practice before and after the adoption of a new PDA protocol, and to analyze its impact on mortality and the main outcomes, especially in preterm infants born under 26 weeks of gestation.
The aims of the present study were:
- 1.
To evaluate the differences in treatment received because of a change in practice as the main outcome.
- 2.
To evaluate the differences in main outcomes because of a change in practice as secondary outcomes.
- 3.
To analyze the impact of a more conservative approach to PDA in the most immature subgroup of extreme preterm newborns (born less than 27 weeks of gestation).
Medical charts of inborn premature infants ≤30 weeks of gestation at birth diagnosed with PDA were reviewed. The study comprised patients admitted to the tertiary newborn intensive care units of Hospital Sant Joan de Déu and Parc Taulí Hospital from January 2009 to December 2016. Maternal, perinatal, and neonatal data were collected from medical charts. Patients who died before three days of life, those who had a congenital heart disease, and outborn patients were excluded. Ethical approval for data collection was obtained.
According to the definition of Vermont Oxford Network (VON),8 PDA was diagnosed based upon at least one of the following findings: left to right or bidirectional ductal shunt on Doppler echo and/or systolic or continuous murmur; and at least two of the following: hyperdynamic precordium, bounding pulses, wide pulse pressure, pulmonary vascular congestion, and cardiomegaly Cardiologists at both centers conducted a color Doppler study of ductal flow in two dimensions with parasternal axis and suprasternal views in all patients. They determined transductal diameter, pulmonary anterograd diastolic flow, left atrial: aorta ratio, aortic retrograde diastolic flow and transductal flow. The authors did not changed the PDA screening method between the periods.
The main outcome of survival-without-morbidity was a composite outcome defined by the absence of any of the secondary outcomes at discharge: chronic lung disease (CLD) defined as supplemental oxygen use at 36 weeks postmenstrual age; severe retinopathy (ROP) grade>2 or plus disease according to the international classification8; necrotizing enterocolitis (NEC) grade>2 according to the Bell classification,9 and severe intraventricular hemorrhage (IVH) grade>2 according to the Papile classification.10
A staging classification of PDA was used to decide whether or not patients received treatment. This classification, which ranges from mild to severe, is based predominantly on the severity and repercussions of the ductal shunting in the cardiovascular, respiratory, and gastrointestinal systems.11 Medical treatment was performed with intravenous ibuprofen at standard dose and surgical treatment implied a classical ligation or the use of a clip.
Additional strategies were also applied to modulate the ductal flow. The authosrs adjusted non-invasive ventilation to a higher positive pressure at the end of the expiration (6–8cm H2O). An accurate fluid balance (135–150mL/kg/day) was maintained, ensuring an optimal energy intake (at least 120kcal/kg/day). The administration of rapid volume bolus was avoided. The authors corrected anemia to a target hematocrit>35%. In the presence of any sign of heart failure or pulmonary edema at chest radiography, diuretics were considered.
In July 2011, the protocol was changed to a more conservative PDA approach as described below.
In the first period, or P1 (2009–2011): medical treatment with ibuprofen was administered if the patient had a PDA according to the VON definition.8 Surgical ligation was performed after failure of two courses of pharmacological treatment if the patient still needed respiratory support (invasive or non-invasive), and if PDA measured more than 2mm by ultrasound.
In the second period, or P2 (2012–2016): medical treatment with ibuprofen was administered if the patient had any of the following clinical signs of PDA: frequent desaturation (>6times/day) not related to another condition, need for respiratory support (invasive or non-invasive), systemic hypotension (mean arterial blood pressure below the 3rd percentile for corrected age), metabolic acidosis (pH<7.10), and pulmonary hemorrhage (evidenced discharge of bloody fluid from the upper respiratory tract or the endotracheal tube and new infiltrates in the chest X-ray) and a PDA of more than 2mm by ultrasound after the first week of life. Surgical ligation of PDA was performed after failure of two courses of pharmacological treatment in the presence of a PDA>3mm and cardiopulmonary compromise defined as two unsuccessful attempts of weaning from the respirator or sustained need of inotropic support attributable to the presence of PDA. Moreover, surgical ligation was postponed until the third or fourth week of life whenever possible. Prophylactic medical treatment was not used.
In both periods, the size of the patent ductus at diagnosis was recorded (in millimeters using color Doppler), postnatal age (in days) at the beginning of medical treatment, and surgical treatment, if performed. Death before 36 weeks postmenstrual age and composited outcome survival without morbidity were examined. The absence of transductal flow in Doppler ultrasound was considered as a marker of closure. Patent ductus at discharge was considered when the presence of a left to right shunt with a greater diameter than 1.5mm was detected in Doppler ultrasound. These patients were followed up by pediatric cardiologists and the date of definitive closure was recorded (spontaneous or surgical closure). If surgical closure was required, the type of device used was recorded. Finally, to analyze the impact of a more conservative approach in the most premature neonates (23–26 weeks), a stratified analysis was performed.
Perinatal and neonatal risk factors for PDA and outcomes were summarized using descriptive statistics (frequency distribution for categorical data and mean and standard deviation or median and interquartile range for continuous data). Univariate analysis included the chi-squared test and Fisher's exact test, as appropriate, for categorical comparisons, and Student's t-test or the Mann–Whitney test for continuous variables. An adjusted logistic regression model was used to assess the change in PDA management in survival without morbidity. All hypothesis tests were two sided and p-values <0.05 were considered statistically significant. All data were analyzed using SPSS (IBM Corporation, Statistical Package for the Social Sciences, version 20.0, USA).
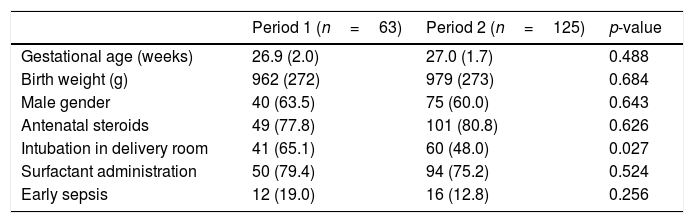
ResultsThe study sample included 188 infants (61% male) with a mean (±SD) gestational age of 27 (±1.8) weeks and a mean birth weight of 973 (±272)g; of these, 82 (43.6%) were born at ≤26 weeks. In the whole cohort, 80% received at least one dose of antenatal steroids, 54% required intubation in the delivery room, 77% received surfactant, and 15% were diagnosed with early sepsis. The authors did not find significant differences comparing the two periods in the main perinatal and clinical risk factors, except for the need for intubation in the delivery room (65.1% in P1 versus 48% in P2; p=0.027) (Table 1).
Patients’ clinical characteristics and prevalence of main perinatal and neonatal risk factors for patent ductus arteriosus.
| Period 1 (n=63) | Period 2 (n=125) | p-value | |
|---|---|---|---|
| Gestational age (weeks) | 26.9 (2.0) | 27.0 (1.7) | 0.488 |
| Birth weight (g) | 962 (272) | 979 (273) | 0.684 |
| Male gender | 40 (63.5) | 75 (60.0) | 0.643 |
| Antenatal steroids | 49 (77.8) | 101 (80.8) | 0.626 |
| Intubation in delivery room | 41 (65.1) | 60 (48.0) | 0.027 |
| Surfactant administration | 50 (79.4) | 94 (75.2) | 0.524 |
| Early sepsis | 12 (19.0) | 16 (12.8) | 0.256 |
Values are n (%) or mean (standard deviation).
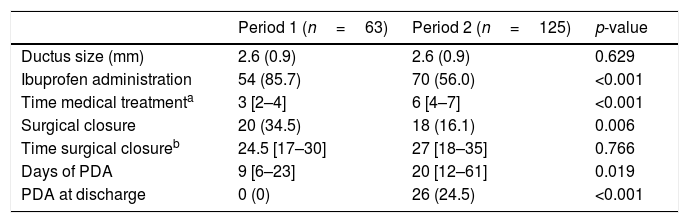
No differences in ductus size at diagnosis were found comparing the two periods. In P2, fewer patients received ibuprofen (number needed to harm=3 [95% CI: 2.5–6.2]) and were treated later (6th day), and fewer patients had surgical closure (number needed to harm=5 [95% CI: 3.1–20.3]). Treated patients in P2 were more immature (26.6±1.5 weeks vs 27.7±1.9 weeks, p<0.001) and had higher rates of CLD (23.3% versus 6.4%, p=0.017) and severe ROP (19% versus 2%, p=0.007), but these outcomes were not significant when adjusting for gestational age. A decrease in medical (77% in 2011 versus 40% in 2015) and surgical (18% in 2011 versus 10% in 2015) treatment was observed over time.
In P2, patients had more days of PDA, and 26 patients (24.5%) were discharged home with a patent ductus (Table 2). Of these, only two patients born before 26 weeks of gestation required transcatheter ductus closure during the follow-up (one at 4 years of age and the other at 10 months). PDA closure occurred before 12 months of life in 90% of the patients discharged home with a patent ductus, with a median patency of 157 days (122–241). None of the patients discharged home with PDA developed pulmonary hypertension during the follow-up.
Patent ductus arteriosus (PDA) treatment and duration of its administration. Days of PDA and PDA at discharge.
| Period 1 (n=63) | Period 2 (n=125) | p-value | |
|---|---|---|---|
| Ductus size (mm) | 2.6 (0.9) | 2.6 (0.9) | 0.629 |
| Ibuprofen administration | 54 (85.7) | 70 (56.0) | <0.001 |
| Time medical treatmenta | 3 [2–4] | 6 [4–7] | <0.001 |
| Surgical closure | 20 (34.5) | 18 (16.1) | 0.006 |
| Time surgical closureb | 24.5 [17–30] | 27 [18–35] | 0.766 |
| Days of PDA | 9 [6–23] | 20 [12–61] | 0.019 |
| PDA at discharge | 0 (0) | 26 (24.5) | <0.001 |
Values are n (%), mean (standard deviation), or median [p25–p75].
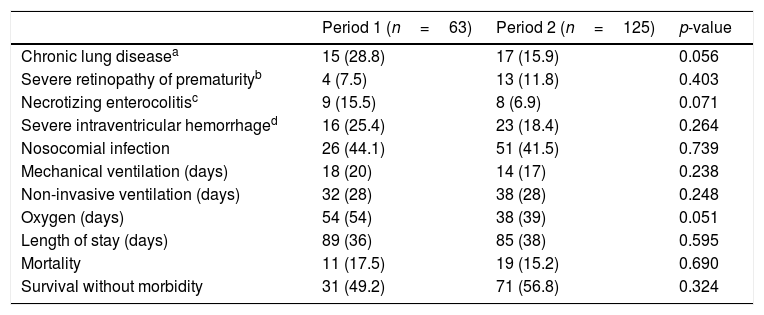
No significant differences between periods in main outcomes were found in the need for and duration of respiratory support, rate of nosocomial infection, or length of stay (Table 3). No differences were found in mortality rates (17.5% versus 15.2%; p=0.690). Survival-without-morbidity was similar in the two periods when adjusted for gestational age and intubation in the delivery room, adjusted OR=1.10 (95% CI: 0.55–2.22); p=0.783.
Main outcomes in both periods.
| Period 1 (n=63) | Period 2 (n=125) | p-value | |
|---|---|---|---|
| Chronic lung diseasea | 15 (28.8) | 17 (15.9) | 0.056 |
| Severe retinopathy of prematurityb | 4 (7.5) | 13 (11.8) | 0.403 |
| Necrotizing enterocolitisc | 9 (15.5) | 8 (6.9) | 0.071 |
| Severe intraventricular hemorrhaged | 16 (25.4) | 23 (18.4) | 0.264 |
| Nosocomial infection | 26 (44.1) | 51 (41.5) | 0.739 |
| Mechanical ventilation (days) | 18 (20) | 14 (17) | 0.238 |
| Non-invasive ventilation (days) | 32 (28) | 38 (28) | 0.248 |
| Oxygen (days) | 54 (54) | 38 (39) | 0.051 |
| Length of stay (days) | 89 (36) | 85 (38) | 0.595 |
| Mortality | 11 (17.5) | 19 (15.2) | 0.690 |
| Survival without morbidity | 31 (49.2) | 71 (56.8) | 0.324 |
Values are n (%) or mean (standard deviation).
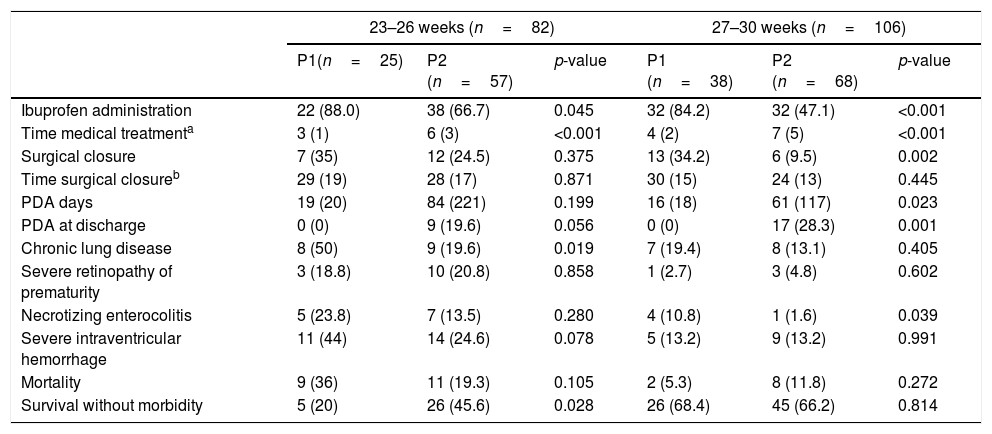
In a subgroup analysis performed to assess the impact of a more conservative approach in the most preterm neonates (23–26 weeks versus 27–30 weeks), it was found that patients born at 23–26 weeks of gestational age also received less medical treatment (88% versus 66.7%, p<0.045) and surgical treatment (35% versus 24.5%; p=0.375), although neither was statistically significant. Differences both in the incidence of CLD (50% versus 19.6%) and survival-without-morbidity (20% versus 45.6%) were found, although significance was not reached when adjusting by mechanical ventilation >24h, with an adjusted OR=2.24 (95% CI: 0.68–7.35); p=0.186 (Table 4).
Patent ductus arteriosus (PDA) treatment and main outcomes in each period according to gestational age.
| 23–26 weeks (n=82) | 27–30 weeks (n=106) | |||||
|---|---|---|---|---|---|---|
| P1(n=25) | P2 (n=57) | p-value | P1 (n=38) | P2 (n=68) | p-value | |
| Ibuprofen administration | 22 (88.0) | 38 (66.7) | 0.045 | 32 (84.2) | 32 (47.1) | <0.001 |
| Time medical treatmenta | 3 (1) | 6 (3) | <0.001 | 4 (2) | 7 (5) | <0.001 |
| Surgical closure | 7 (35) | 12 (24.5) | 0.375 | 13 (34.2) | 6 (9.5) | 0.002 |
| Time surgical closureb | 29 (19) | 28 (17) | 0.871 | 30 (15) | 24 (13) | 0.445 |
| PDA days | 19 (20) | 84 (221) | 0.199 | 16 (18) | 61 (117) | 0.023 |
| PDA at discharge | 0 (0) | 9 (19.6) | 0.056 | 0 (0) | 17 (28.3) | 0.001 |
| Chronic lung disease | 8 (50) | 9 (19.6) | 0.019 | 7 (19.4) | 8 (13.1) | 0.405 |
| Severe retinopathy of prematurity | 3 (18.8) | 10 (20.8) | 0.858 | 1 (2.7) | 3 (4.8) | 0.602 |
| Necrotizing enterocolitis | 5 (23.8) | 7 (13.5) | 0.280 | 4 (10.8) | 1 (1.6) | 0.039 |
| Severe intraventricular hemorrhage | 11 (44) | 14 (24.6) | 0.078 | 5 (13.2) | 9 (13.2) | 0.991 |
| Mortality | 9 (36) | 11 (19.3) | 0.105 | 2 (5.3) | 8 (11.8) | 0.272 |
| Survival without morbidity | 5 (20) | 26 (45.6) | 0.028 | 26 (68.4) | 45 (66.2) | 0.814 |
Values are n (%) or mean (standard deviation).
More conservative management of PDA in this population has shown a 30% reduction in medical and 20% in surgical treatment without changes in mortality or survival-without-morbidity.
Scientific evidence on management of PDA is wide-ranging and sometimes contradictory; even today this condition sees diverse approaches.12 In preterm <32 weeks of gestation age, lower rates of medical treatment (around 20%) and surgical ligation (<10%) have been previously reported.11,13–15 Chock et al. described similar rates as those of the present study; in era 1, 18% of infants had conservative management versus 39% in era 2 (p<0.01).16 On contrary, Bixler et al. found lower rates of medical treatment: between 20 and 38% use of indomethacin or ibuprofen for PDA treatment in infants <28 weeks of gestation in 2015, and 3–10% PDA ligation in infants <28 weeks of gestation in 2015.13 Thus, while the medical treatment rate of 56% and the surgical ligation rate of 16% may still be considered high, this population has a wide range of gestational age, with 43.6% of infants born at <27 weeks of gestational age. Perhaps different personal approaches among the neonatologists of these centers had influence on these results; some reticence, especially during the first months after the change in protocol, could have existed. Unfortunately, the authors did not supervise the adherence to the protocol, nor planned a washout period.
One relevant finding in this study that is worth highlighting is that surgery was avoided in one out of every five patients.
One of our objectives was also to explore treatment in the most immature patients (23–27 weeks). Despite the change of the protocol to a more conservative approach, two thirds of the patients were treated with cyclooxygenase inhibitors and 24.5%, surgically. Lee et al. reported a rate of surgical ligation of 43% in patients with birth weight <750g and of 24% in patients weighing between 715 and 1000g.17 Weisz et al. also reported a rate of 24% for surgical ligation of PDA in extremely premature infants.18
Significant delay in the administration of the first dose of ibuprofen was observed, from 3 days of life in P1 to 6 days in P2. In a population-based cohort study of infants born before 27 weeks of gestation from the EXPRESS study (Extremely Preterm Infants in Sweden Study), the authors found that a late start of medical treatment was associated with a lower risk of chronic lung disease.19 A significant delay in surgery was not detected as other authors have,12,16 probably because surgical closure was already performed around the third or the fourth week of life in P1.
The question of the role of PDA in respiratory, neurological, and gastrointestinal outcomes has been widely discussed6,18,20,21: a hemodynamically significant left-to-right shunt could result in a higher pulmonary blood flow and a compromised perfusion of vital organs. Some authors hypothesize that adverse outcomes historically associated with PDA may also be linked to prematurity itself or to some other co-existing condition, such as intrauterine infection or inflammation.22 Benitz concluded that there is no clear evidence that active treatment is beneficial for premature infants because it does not clearly improve mortality or morbidities such as chronic lung disease, necrotizing enterocolitis, intraventricular hemorrhage, and retinopathy.23 Chock et al. compared very low birth weight infants diagnosed with a PDA in two different eras and did not find an increase in adverse clinical outcomes.16 Statistically significant differences between P1 and P2 in the main outcomes classically related to prematurity have not been shown, as can be seen in Table 3.
A non-significant reduction in the global incidence of severe necrotizing enterocolitis from 15.5% to 6.9% was found. A significant reduction in the incidence of severe necrotizing enterocolitis from 10.8% to 1.6% was found in patients between 27 and 30 weeks of gestation between periods. In 2011, donor milk was introduced in these hospitals, so the reduction in NEC could more relate to this fact than directly to PDA treatment. Still, a lower use of cyclooxygenase inhibitors in P2 might have played a role.5,20
Classically, the ductal shunt is thought to have a negative influence on lung development; Mohamed et al. did not find differences in chronic lung disease between two PDA therapeutic periods,24 and Slaughter et al. identified no changes in mortality or moderate-to-severe bronchopulmonary dysplasia in preterm infants <29 weeks of gestation after medical treatment for PDA.25 Conversely, Bixler et al. observed a progressive reduction in all the main morbidities, except for bronchopulmonary dysplasia, in a large population of infants with <30 weeks of gestation from 2006 to 2015.11 In P2, reduction in the incidence of chronic lung disease and survival without morbidity was observed, especially in the most premature patients. Prenatal and postnatal improvement of care in premature infants in recent years, including less intubation in the delivery room and protective ventilatory strategies, probably had an impact on these results.
The authors detected a non-significant but worrying increase from 5.3% to 11.8% in mortality in the conservative period in patients between 27 and 30 weeks of gestation. Reviewing the medical charts of these infants, two of them born at 27 weeks of gestation died in the first week of life due to respiratory and hemodynamic instability in the context of severe bilateral intraventricular hemorrhage. Another four patients died of causes related to congenital or nosocomial infections.
With conservative management of PDA, neonatologists must face new challenges.26 PDA might be understood as a type of chronic condition during the hospital stay.27 It was shown in the present study that there was a remarkable increase in the duration of the patency of ductus arteriosus. This might lead in clinical practice to accurate respiratory management, fluid policy, enteral feeding, blood transfusion criteria, and subsequent clinical and echocardiographic monitoring. In this study, a remarkable number of patients were discharged from hospital with a PDA. A question to consider is how having a prolonged left to right shunt can affect brain perfusion and growth status. More follow-up studies are needed to learn what the long-term neurodevelopment outcomes of these infants will be.28
The authors acknowledge some limitations in the present study. As it is a retrospective clinical study, it is not possible to test the causality of relationships or determine whether changes in practice between periods affected the results. There was no washout period between the eras; it is likely that not all neonatologists made the immediate and complete change to a conservative approach. The authors compared the size of PDA between groups; the cohorts were not matched in terms of hemodynamic significance of the PDA, which could have been very interesting. The sample size of the most immature subgroups might have limited the power to detect statistically significant differences.
In conclusion, this study found that a conservative and more permissive approach in very low birth weight neonates with PDA can in some cases avoid medical and surgical treatments and their potential side effects, without relevant changes in mortality and in survival-without-morbidity. In the youngest patients, rates of medical and surgical treatments for PDA are still high, but more of these patients survive and with fewer associated morbidities. A notable group of patients were discharged home with a permeable ductus without apparent undesirable outcomes, but long-term follow-up is still needed.
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Borràs-Novell C, Riverola A, Aldecoa-Bilbao V, Izquierdo M, Domingo M, Iriondo M. Clinical outcomes after more conservative management of patent ductus arteriosus in preterm infants. J Pediatr (Rio J). 2020;96:177–83.