To compare two electrolyte maintenance solutions in the postoperative period in children undergoing appendectomy, in relation to the occurrence of hyponatremia and water retention.
MethodsA randomized clinical study involving 50 pediatric patients undergoing appendectomy, who were randomized to receive 2,000mL/m2/day of isotonic (Na 150 mEq/L or 0.9% NaCl) or hypotonic (Na 30 mEq/L NaCl or 0.18%) solution. Electrolytes, glucose, urea, and creatinine were measured at baseline, 24h, and 48h after surgery. Volume infused, diuresis, weight, and water balance were analyzed.
ResultsTwenty-four patients had initial hyponatremia; in this group, 13 received hypotonic solution. Seventeen patients remained hyponatremic 48h after surgery, of whom ten had received hypotonic solution. In both groups, sodium levels increased at 24h (137.4±2.2 and 137.0±2.7mmol/L), with no significant difference between them (p=0.593). Sodium levels 48h after surgery were 136.6±2.7 and 136.2±2.3mmol/L in isotonic and hypotonic groups, respectively, with no significant difference. The infused volume and urine output did not differ between groups during the study. The water balance was higher in the period before surgery in patients who received hypotonic solution (p=0.021).
ConclusionsIn the post-appendectomy period, the use of hypotonic solution (30 mEq/L, 0.18%) did not increase the risk of hyponatremia when compared to isotonic saline. The use of isotonic solution (150 mEq/L, 0.9%) did not favor hypernatremia in these patients. Children who received hypotonic solution showed higher cumulative fluid balance in the preoperative period
Comparar duas soluções de manutenção hidroeletrolítica no período pós-operatório (PO) de crianças submetidas à apendicectomia, quanto à ocorrência de hiponatremia e retenção hídrica.
MétodosEstudo clínico randomizado envolvendo 50 pacientes pediátricos submetidos à apendicectomia, randomizados a receber 2000ml/m2/dia de solução isotônica (Na 150 mEq/L ou NaCl 0,9%) ou hipotônica (Na 30mEq/L ou NaCl 0,18%). Eletrólitos, glicose, ureia e creatinina foram mensurados no início do estudo, 24 e 48 horas após a cirurgia. Foram analisados volume infundido, diurese, peso e balanço hídrico.
Resultados24 pacientes apresentaram hiponatremia inicial, destes 13 receberam solução hipotônica. Dezessete pacientes permaneceram hiponatrêmicas 48 horas após a cirurgia, 10 haviam recebido solução hipotônica. Nos dois grupos os níveis de sódio aumentaram na 24ª hora PO (137,4±2,2 e 137,0±2,7), não havendo diferença entre eles (p=0,593). Níveis de sódio 48h após a cirurgia foram 136,6±2,7 e 136,2±2,3 no grupo isotônico e hipotônico respectivamente sem diferença significativa. Os volumes infundidos e diurese não diferiram entre os grupos durante o estudo. O balanço hídrico foi maior no período anterior à cirurgia no grupo de pacientes que receberam solução hipotônica (p=0,021).
ConclusõesNo período pós-apendicectomia, o uso da solução hipotônica não aumentou o risco de hiponatremia, quando comparado a uma solução salina isotônica. O uso da solução isotônica não favoreceu a hipernatremia nestes pacientes. Crianças que receberam solução hipotônica apresentaram maior balanço hídrico cumulativo no período pré-operatório.
Hyponatremia is an electrolyte disorder commonly seen in hospitalized patients, defined as serum sodium levels<136mmol/L.1–5 Its etiology has been related to fluid retention. If the infused fluid volume exceeds that of renal excretion capacity, dilution of extracellular solutes reduces osmolarity.1 The presence of hypotonicity promotes cerebral edema due to imbalance between the intracellular and extracellular osmolarity in neuronal tissue. In the occurrence of acute decrease in serum sodium (Na+< 130mmol/L), extracellular water penetrates the nerve cells, aiming to equalize the intra- and extra-cellular tonicities.2,6
The maintenance solution proposed by Holliday & Segar in 1957, still widely used, was based on the metabolism of healthy children and calculated based on body weight (< 10kg, 11-20kg,>20kg; 3 mEq/L of Na+ and 2 mEq/L of K+), resulting in a hypotonic solution and excessive fluid intake for critically-ill children, which may cause the onset of hyponatremia.7,8 The presence of stress (pain, fever, surgery), nausea, vomiting, anesthesia, intestinal manipulation, and hypovolemia are non-osmotic stimuli that increase the secretion and activity of the antidiuretic hormone (ADH) (arginine vasopressin).1 High ADH action limits free water excretion and acute disease leads to the production of endogenous water, increasing the extracellular volume and resulting in or worsening the occurrence of hyponatremia.9 A recent review involving more than 500 children in six prospective studies showed that the use of isotonic solutions prevents hyponatremia in the postoperative (PO) period and that the use of hypotonic fluids results in decreased sodium.10
Children submitted to surgical procedures are at greater risk of hyponatremia and its neurological consequences, both due to ADH stimulation and the increased possibility of endogenous water production.4,11,12 All these circumstances increase the chances of hyponatremia and neurological complications in previously healthy patients.
The use of isotonic solutions during and after surgery has been suggested as a mean to prevent hyponatremia in the PO period.13,14 Some authors defend that the incidence of hyponatremia may be associated with the administered solution volume rather than its sodium content.15 Moreover, a prospective, randomized trial compared isotonic versus hypotonic intravenous fluid and maintenance volumes of 50% or 100%, and concluded that the risk of hyponatremia was lower with the use of isotonic saline solution and not by use of water restriction.13
In the last decade, the prevention of hospital-acquired hyponatremia has been systematically debated, with some authors strongly recommending the use of isotonic solution, whereas others recommend the use of isotonic fluids associated with water restriction.6,16 Others oppose the use of isotonic fluid, claiming that hyponatremia is mainly the result of hemodilution and, therefore, fluid restriction could prevent hyponatremia.17 The aim of this study was to compare the use of hypotonic and isotonic solutions in fluid maintenance (2,000mL/m2) in the pre-operative and post-operative periods in children and adolescents undergoing appendectomy.
MethodsBetween March of 2012 and January of 2013, a prospective, double-blind, randomized trial was conducted after being approved by the Research Ethics Committee of Pontifícia Universidade Católica do Rio Grande do Sul (CEP 11/05688) and the Department of Teaching and Research of the Hospital Universitário de Santa Maria, where data collection was performed. An informed consent was signed by the childs parent/guardian prior to study enrollment, and whenever possible, the informed consent was also signed by the child.
Children aged 1-14 years with a diagnosis of acute appendicitis and eligible for surgical treatment were included. The type of appendicitis was classified as non-complicated in cases where the appendix was intact or complicated when there was organ perforation and/or peritonitis. The patients were weighed on admission and 48h after the surgical procedure. Patients that had severe hemodynamic disorder, shock, and/or were receiving vasoactive drugs on admission were excluded.
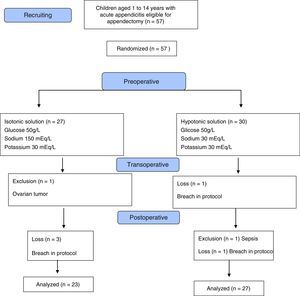
Participants were randomly assigned to receive isotonic or hypotonic solution at the time of admission to the pediatric emergency room. Aiming to maintain a balanced allocation in both groups at all times of the study, randomization was performed in groups of ten patients, five for each of the solutions. The researcher and medical assistants were blinded to the solution content and the emergency nursing staff prepared the solutions, labeled A or B, plus the infusion in mL/hour. The isotonic solution contained 150 mEq/L of sodium chloride, 30 mEq/L of potassium chloride, and 5% glucose, whereas the hypotonic contained 30 mEq/L of sodium chloride, with the same content of glucose and potassium. The total infused volume estimated for both solutions was 2,000mL/m2/24h (Fig. 1).
Test collection was performed at the time of randomization. All patients received initial fluid loss replacement with 0.9% saline solution with a volume of 20mL/kg before the specific solutions. The infusion during the intraoperative period was performed with 0.9% saline, with the volume established by the anesthesiologist and considered in the total volume of the study.
The solution was administered from admission to 48h of the PO period, except for the perioperative period. Samples for laboratory tests (Na+, K+, Ca++, chloride, glucose, urea, creatinine, and bicarbonate levels) were collected at the start of the infusion, 24h, and 48h after surgery, and then analyzed by the ion-selective method. Diuresis and fluid balance were performed at three intervals: from admission to surgery, surgery to 24h, and 24h to 48h after appendectomy. The other measures of patient care were performed by the assisting medical team.
The primary endpoint was serum sodium levels during the intervention and at the end of 48h of the protocol. Hypernatremia was defined as serum Na>145 mEq/L and hyponatremia as serum Na<136 mEq/L. Moderate hyponatremia was considered when serum Na was between 130 and 135 mEq/L, and severe when<130 mEq/L. Secondary outcomes were the presence of hypervolemia (estimated by the cumulative positive fluid balance and/or weight gain) and the presence of other electrolyte disturbances.
Quantitative variables with normal distribution were expressed as mean and standard deviation and compared by Student's t-test, whereas variables without a normal distribution were compared using the Mann-Whitney U test. Categorical variables were shown as absolute and relative frequencies and association was verified using the chi-squared test. Values were considered statistically significant with p-values<0.05. The analyses were performed using SPSS (SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago, USA).
ResultsDuring the study period, a total of 57 children aged 1 to 14 years submitted to appendectomy were admitted. These individuals were randomized to receive intravenous isotonic or hypotonic maintenance solution. One patient was excluded in the isotonic group due to ovarian tumor and there were three losses due to protocol breach, totaling 23 patients in this group. One patient was excluded from the hypotonic group due to sepsis and there were two losses, resulting in 27 subjects. Initial sodium was not measured in one patient and in four patients after 24h.
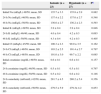
The anthropometric characteristics were similar in both groups (Table 1). For each individual, sodium levels were measured at admission, after 24h, and after 48h. There were no significant differences between the three measurement periods. At admission, 24 (49%) patients had moderate hyponatremia (Na+>130 and<135 mEq/L) and 25 (51%) had normal sodium (Na>136 mEq/L).
Characteristics of the two groups of patients undergoing appendectomy according to the administered solution.
| Isotonic (n=23) | Hypotonic (n=27) | p | |
|---|---|---|---|
| Age, years; mean, SD | 8.8±3.6 | 10.3±2.9 | 0.106a |
| Weight, kg; mean, SD | 35.1±14.0 | 37.1±12.2 | 0.596a |
| Male gender, n (%) | 13 (43.3%) | 17 (56.7%) | 0.643b |
| BMI; mean, SD | 18.5±3.4 | 20.7±4.7 | 0.205c |
| Complicated appendicitis, n (%) | 14 (45.1%) | 17 (54.9%) | 0.879b |
| Non-complicated appendicitis, n (%) | 9 (47.4%) | 10 (52.6%) | 0.880b |
| Preoperative fasting, hours, IQ | 5 (3-9) | 6 (4-12) | 0.190a |
| Postoperative fasting, hours, IQ | 33 (25-48) | 38 (28-48) | 0.748a |
| Hospital length of stay, days, IQ | 6 (4-8) | 6 (5-7) | 0.745a |
SD, standard deviation; BMI, body mass index; IQ, interquartile range.
p-values based on test.
After 24h, 12 patients had hyponatremia, of whom seven had received hypotonic solution. After 48h, 17 children had hyponatremia, of whom ten had received hypotonic solution. The anthropometric and biochemical characteristics are shown in Tables 1 and 2, respectively.
Initial electrolytes and osmolarity 24 and 48hours PO.
| Isotonic (n=23) | Hypotonic (n=27) | Pa | |
|---|---|---|---|
| Initial Na (mEq/L) 49/50; mean, SD | 135.7±3.3 | 135.8±2.9 | 0.882 |
| 24h Na (mEq/L) 46/50; mean, SD | 137.4±2.2 | 137.0±2.7 | 0.548 |
| 48h Na (mEq/L) 50/50; mean, SD | 136.6±2.7 | 136.2±2.3 | 0.593 |
| Initial K (mEq/L) 49/50; mean, SD | 3.9±0.4 | 3.9±0.4 | 0.846 |
| 24hK (mEq/L) 46/40; mean, SD | 4.0±0.4 | 4.2±0.3 | 0.093 |
| 48hK (mEq/L) 50/50; mean, SD | 4.3±0.4 | 4.2±0.3 | 0.405 |
| Initial Cl (mEq/L) 45/50; mean, SD | 100.3±2.3 | 99.0±3.5 | 0.162 |
| 24h Cl (mEq/L) 46/50; mean, SD | 103.2±2.5 | 101.4±2.7 | 0.797 |
| 48h Cl (mEq/L) 48/50; mean, SD | 101.0±3.0 | 99.7±2.2 | 0.085 |
| Initial creatinine (mg/dL) 49/50; mean, SD | 0.6±0.1 | 0.6±0.1 | 0.157 |
| 24h creatinine (mg/dL) 46/50; mean, SD | 0.5±0.1 | 0.5±0.1 | 0.797 |
| 48h creatinine (mg/dL) 50/50; mean, SD | 0.5±0.2 | 0.6±0.2 | 0.146 |
| 24h osmolarity (mOsm/L) 42/50; mean, SD | 281.7±4.5 | 280.2±5.4 | 0.356 |
| 48h osmolarity (mOsm/L) 50/50; mean, SD | 279.5±5.9 | 279.3± 4.2 | 0.853 |
SD, standard deviation.
The group of patients that received isotonic solution showed mean sodium increase of 1.7 mEq/L in the period between admission and the 24-hour measurement, whereas the group treated with hypotonic solution had an increase of 1.2 mEq/L. Between the 24- and 48-hourmeasurements, there was a decrease of 0.8 mEq/L in both groups. Between the initial Na+ and final Na+ (48h), there was an increase of 0.9 mEq/L in the isotonic group and of 0.4 mEq/L in hypotonic group. These differences were not significant (Table 3).
Infused volumes, fluid balance, and diuresis in both groups.
| Variables | Isotonic | Hypotonic | p |
|---|---|---|---|
| Weight, kg; mean±SD | 35.1±14.0 | 37.1±12.2 | 0.596a |
| Weight 48h; mean±SD | 35.62±14.6 | 37.56 ±12.5 | 0.615a |
| Preoperative expansion, mL/m2; median, IQ | 347.8 (285.7–500) | 363.6 (286.6–571.4) | 0.740b |
| Preoperative volume, mL/m2; median, IQ | 246.7 (86.3–653.3) | 353 (166.5–695.0) | 0.280b |
| Transoperative volume, mL/m2; median, IQ | 555.5 (384.6–750) | 649.4 (357.1–833.3) | 0.413a |
| 24h PO Volume, mL/m2; mean±SD | 1,956.3±369.7 | 2,029.4±252.0 | 0.290a |
| 48h PO Volume, mL/m2; mean±SD | 2,010.6±262.1 | 2,020±190.0 | 0.880a |
| Preoperative fluid balance, mL/kg; median, IQ | 12.00 (4–19.9) | 19.4 (12.6–24.9) | 0.021b |
| 24h PO fluid balance, mL/kg; median, IQ | 22.6 (8.7–33.6) | 24.8 (4.4–27.5) | 0.647 b |
| 48h PO fluid balance, mL/kg; median, IQ | 9.8 (-12.9 to +17.9) | 6.82 (-11.0 to +19.4) | 0.808b |
| Preoperative diuresis, mL/kg/h; mean±SD | 1.92±2.91 | 0.85±1.41 | 0.097a |
| 24h PO diuresis, mL/kg/h; mean±SD | 1.99±1.01 | 1.98±0.8 | 0.957a |
| 48h PO diuresis, mL/kg/h; mean±SD | 2.7±1.3 | 2.6±1.2 | 0.780a |
p-values based on a Student's t-test, b Mann-Whitney U test.
In the group of eight patients with normal initial sodium (> 136 mEq/L) and low final sodium (< 135 mEq/L), three received isotonic and five received hypotonic saline solution with an initial variation of 136 to 140 mEq/L and final (48h) of 132 to 135 mEq/L.
In the group admitted with low sodium (130-135 mEq/L), nine children remained hyponatremic (132-135 mEq/L) at the end, of whom four had received isotonic solution, and five hypotonic solution.
Of the 15 patients that had initial hyponatremia (130-135 mEq/L) and normal Na+ at 48h (136-140 mEq/L), seven received isotonic solution and eight hypotonic solution.
Of the 17 patients that showed normal sodium levels, eight received isotonic and nine hypotonic solution.
Regarding sodium evolution from 24 to 48h PO, eight children had normal sodium (136-142 mEq/L) after 24h, but had hyponatremia after 48h (132 to 135 mEq/L); half of them received isotonic solution, and half received hypotonic solution.
Eight patients remained hyponatremic (24h: 131-135 mEq/L and 48h: 132-135 mEq/L); four received isotonic and four hypotonic solution. The other 30 children had normal sodium 48h after surgery. Sodium level measurements were not performed in four patients 24h after surgery.
Four children required volume expansion in the PO period: three from the isotonic group and one from the hypotonic group; none of the children required electrolyte correction.
Both groups (isotonic and hypotonic) showed weight gain during the first 48h, but with no significant differences between them. However, the fluid balance in the preoperative period was significantly higher in the group receiving hypotonic solution (median 19.4ml/kg; IQ: 12.6–24.9) than in the group receiving isotonic solution (median 12.0ml/kg, IQ: 4–19.9) (p=0.021). During this interval, which was similar in both groups, the isotonic group showed a tendency towards higher diuresis (p=0.097).
Volume expansion after surgery was necessary in four patients: three receiving isotonic solution and one from the hypotonic group. On the second day of protocol, only one patient receiving isotonic solution required rapid volume expansion, which was carried out using saline solution (0.9% NaCl).
DiscussionIn this double-blind, randomized study involving children submitted to appendectomy, it was observed that: (a) the administration of hypotonic maintenance solution did not increase the chance of hyponatremia when compared to the isotonic solution; (b) the infusion of isotonic solution did not prevent the onset of hyponatremia in the PO period and did not increase the occurrence of hypernatremia in this period; (c) most of the group who had hyponatremia at admission (24 patients) had sodium levels normalized (n=15) irrespective of the type of administered solution; (d) fluid retention in the preoperative period was higher in patients that received the hypotonic solution.
These findings do not support the results of the investigation by Choong et al., where most of the patients were surgical, demonstrating significantly higher hyponatremia in the group receiving hypotonic solution.8 It is noteworthy that in the present study the patients used the same volume in the PO period (2,000mL/m2/day), with the exception of four children that required volume expansion: three from the isotonic group and one from the hypotonic group. The small number of patients and the lack of standardization of fluid infusion in the pre-hospitalization period may have prevented the appearance of final hyponatremia related to hypotonic solution infusion.
Hyponatremia was observed even in the group that received isotonic solution daily, which may be explained by the possible increase of ADH in all patients undergoing surgery, as previously suggested in the study by Choong et al., through serum measurement of this hormone and urinary electrolytes.8 Several randomized, controlled trials, blinded or not, have shown evidence of isotonic solution protection in relation to hyponatremia in the period close to surgery (before and after the procedure). Most of them had heterogeneous groups of patients, including clinical situations of varying severity and/or major or minor surgeries, making comparisons difficult with the present study.3–5,13,17 After the publication by Hoorn et al. in 2004, several authors have questioned the validity of evidence demonstrating the superiority of isotonic solution to prevent hyponatremia. In a recent meta-analysis conducted with ten randomized controlled trials, the use of isotonic saline solution was shown to be safer than the hypotonic solution, in relation to sodium levels.16
The present study demonstrated that patients with low sodium had received a larger solution volume and that hyponatremia could have been due to this factor.3,15 Greater fluid balance prior to surgery was also demonstrated in the group receiving hypotonic solution, whereas greater diuresis was observed in the isotonic solution group. Hyponatremia can be explained by the increase in extracellular content and consequent solute dilution.
The infused volume also plays an important role in the occurrence of hyponatremia; many studies, although focusing on the sodium content, also offer patients a higher volume than what is usually recommended.17,18 The cross-sectional study by Armon et al. evaluated hospitalized children that were receiving intravenous maintenance solution and reported that hypotonic solutions were administered in most cases (77/99), with 38% receiving maintenance that was higher than 105% of the recommended volume. Twenty-one of 86 patients had hyponatremia (< 135mmol/L).19 The solution proposed by Holliday & Segar for fluid maintenance in hospitalized children results in a hypotonic solution and should be reconsidered.20
The present study was designed to analyze the importance of hyponatremia prevention using an isotonic maintenance solution in a group of patients with similar characteristics and submitted to the same type of surgery. However, this group of patients showed a difference only in fluid retention (higher fluid balance in the hypotonic group and higher diuresis in the isotonic group), demonstrating possible interference of ADH action in these patients or lower expanding capacity of hypotonic solutions, requiring a higher offer to attain the same effect as an isotonic infusion.
The main limitation of the present study refers to sample size, with insufficient power to test whether the occurrence of hyponatremia was associated with the type of infused solution. Additionally, a large proportion of patients had complicated appendicitis (30/50), with prolonged evolution and prolonged fasting time, which could not be controlled. ADH and urinary electrolytes were not measured, which precluded inferences about the presence of hypertonic urine and fluid retention attributed to the hormone.
Even considering the methodological limitations, based on these results it can be suggested that fluid maintenance with either hypotonic or isotonic solution for a short period of time (less than 48h) in patients undergoing appendectomy does not increase the incidence of hyponatremia. However, the use of hypotonic solutions is associated with higher fluid retention than that observed with isotonic solutions. In this respect, it should be noted that positive cumulative fluid balance in critically-ill patients has been associated with higher mortality.21 Studies including a higher number of patients are required to assess both hyponatremia related to hypotonic solution infusion and the unfavorable evolution of patients receiving a higher fluid intake.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Valadão MC, Piva JP, Santana JC, Garcia PC. Comparison of two maintenance electrolyte solutions in children in the postoperative appendectomy period: a randomized, controlled trial. J Pediatr (Rio J). 2015;91:428–34.