To characterize the deaths of 193 children with sickle cell disease screened by a neonatal program from 1998 to 2012 and contrast the initial years with the final years.
MethodsDeaths were identified by active surveillance of children absent to scheduled appointments in Blood Bank Clinical Centers (Hemominas). Clinical and epidemiological data came from death certificates, neonatal screening database, medical records, and family interviews.
ResultsBetween 1998 and 2012, 3,617,919 children were screened and 2,591 had sickle cell disease (1:1,400). There were 193 deaths (7.4%): 153 with SS/Sβ0-talassemia, 34 SC and 6 Sβ+thalassemia; 76.7% were younger than five years; 78% died in the hospital and 21% at home or in transit. The main causes of death were infection (45%), indeterminate (28%), and acute splenic sequestration (14%). In 46% of death certificates, the term “sickle cell” was not recorded. Seven-year death rate for children born between 1998 and 2005 was 5.43% versus 5.12% for those born between 2005 and 2012 (p = 0.72). Medical care was provided to 75% of children; 24% were unassisted. Medical care was provided within 6hours of symptom onset in only half of the interviewed cases. In 40.5% of cases, death occurred within the first 24hours. Low family income was recorded in 90% of cases, and illiteracy in 5%.
ConclusionsAlthough comprehensive and effective, neonatal screening for sickle cell disease was not sufficient to significantly reduce mortality in a newborn screening program. Economic and social development and increase of the knowledge on sickle cell disease among health professionals and family are needed to overcome excessive mortality.
Caracterizar os 193 óbitos de crianças com doença falciforme diagnosticadas por programa de triagem neonatal entre 1998-2012 e comparar os primeiros com os últimos anos.
MétodosOs óbitos foram identificados pela busca ativa das crianças ausentes nas consultas agendadas nos hemocentros. Dados clínicos e epidemiológicos provieram dos documentos de óbito, banco de dados da triagem neonatal, prontuários médicos e entrevistas com familiares.
ResultadosEntre 1998-2012 foram triadas 3.617.919 crianças, 2.591 com doença falciforme (1:1.400). Ocorreram 193 óbitos (7,4%): 153 com SS/Sβ0-talassemia, 34 SC e 6 Sβ+-talassemia; 76,7% em crianças com menos de 5 anos; 78% faleceram em hospitais e 21% em domicílio ou trânsito. Causas principais do óbito: 45% infecção, 28% indeterminada, 14% sequestro esplênico agudo. Em 46% dos documentos de óbito, não houve registro do termo “falciforme”. A taxa de mortalidade até sete anos das crianças nascidas entre 1998-2005 foi 5,43% versus 5,12%, entre 2005-2012 (p=0,72). Receberam assistência médica 75% das crianças; 24% ficaram desassistidas. Pelas entrevistas, atendimento médico teria ocorrido nas primeiras seis horas do início dos sintomas em metade dos casos. O óbito ocorreu em 40,5% dos casos, nas primeiras 24 horas. Baixa renda familiar foi registrada em 90% dos casos e analfabetismo em 5%.
ConclusõesA triagem para doença falciforme, mesmo abrangente e eficaz, não foi suficiente para reduzir significativamente a mortalidade no Programa de Triagem Neonatal. Necessita-se de desenvolvimento econômico e social do estado e ampliação, pela educação continuada, do conhecimento sobre a doença falciforme entre os profissionais de saúde e familiares.
Sickle cell disease (SCD) comprises a group of hematologic disorders of genetic origin, whose main feature is the predominance of hemoglobin S (HbS) in red blood cells. SCD has great clinical and epidemiological importance, being considered a public health problem in Brazil.1–3HbS in homozygous form (HbSS), called sickle cell anemia (SCA), is the most common genotype and the most severe clinical presentation of the disease. The concept of SCD also includes double heterozygosity for HbS with other hemoglobin variants (HbSC, HbSD-Punjab, and others) and the interaction of HbS with beta thalassemia (HbS/β0 and HbS/β+ thalassemias).4,5 The main determinants of the clinical manifestations of the disease are the vaso-occlusive phenomena and chronic hemolysis.4
Hemoglobinopathies are responsible, worldwide, for 3.4% of deaths in children under 5 years.6 Patients with SCD have high rates of morbidity and mortality, mainly in developing countries.7 Even in developed countries, although mortality in children has decreased, SCD is still a significant cause of mortality in adolescents and adults.8
A prevalence of 25,000-30,000 individuals with SCD is estimated in Brazil, with an incidence of 3,500 cases per year.9 In the state of Minas Gerais (MG), the incidence of SCD is 1:1,400 screened newborns, based on data from the Neonatal Screening Program (NSP-MG).10
A study conducted in MG10 characterized the death of 78 children with SCD screened by the NSP-MG in the period of 1998-2005 and concluded that most deaths occurred in children under 2 years and individuals with HbSS, mainly due to infection (septicemia and pneumonia). A predominance of in-hospital deaths was observed; however, the occurrence of at home or in-transit deaths was still significant. An indeterminate cause of death on the death certificate was frequent, which would indicate a lack of knowledge among physicians regarding SCD and acute events that are determinants of death.
This study aimed to characterize the deaths of children with SCD that had been screened by the NSP-MG between 1998 and 2012. Whenever possible, comparative analysis of deaths of children born between March of 1998 and February of 2005 with those born between March of 2005 and December of 2012 was performed to describe possible changes regarding the quality of care provided to these children.
MethodsThe population investigated in this study consisted of 117 children diagnosed with SCD at the NSP-MG, followed-up in the Blood Banks of Fundação Hemominas, and who died in the period from March 1, 2005 to February 29, 2012. In several analyses, 76 deaths that occurred between March of 1998 and February of 2005 were added to the sample (of the 78 deaths reported, two children were excluded, whose birth was prior to March 1,1998),10 totaling 193 deaths and thus complementing the 14 years of the study.
The NSP-MG performs screening for SCD since March of 1998. All 853 state municipalities are registered. In 2010, 91.44% of the infants born in the state of Minas Gerais were screened at the Center for Diagnostic Support Action and Research (Núcleo de Ações e Pesquisa em Apoio Diagnóstico [NUPAD]), and free medical treatment and follow-up was offered to those born with SCD.
The information on death results from an investigation conducted by the Control and Treatment Department of NUPAD due to non-attendance at scheduled consultation at the Blood Bank. The active searches performed encompass all screened patients with SCD followed-up at the outpatient clinic of Fundação Hemominas throughout the state. Therefore, it can be stated that all deaths that occurred during the study period were recorded.
The data for this research came from the NUPAD database, death certificates, the Brazilian Unified Health System database (DATASUS), the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística [IBGE]), medical records of Fundação Hemominas, and from interviews with the children's family members.
The information in the NUPAD database was used to perform an active search of the 117 families whose children had died between 2005 and 2012. The interview was performed with the child's guardian, using a semistructured form used by Fernandes et al.10 A total of 81 families were interviewed by the researcher and three families were interviewed by nurses from the referral Basic Health Units.
Five families refused to be interviewed, one was unable to talk about the subject, and 27 were not located. The interview covered five aspects: (1) death-related circumstances; (2) follow-up of SCD and the occurrence of other acute events; (3) family's socioeconomic and cultural conditions, which considered per capita income, education, parents’ occupation, and housing conditions; (4) considerations about their experience with the child; (5) applying the scale of knowledge on SCD to the families, consisting of 20 questions with answer options: “right”, “wrong”, or “I don’t know.” The interview was performed only after the informed consent form was signed, which encompassed the objectives, purpose, and benefits of the research.
Regarding the causes of death, they were considered as indeterminate when the physicians showed ambiguity in the medical records of the death certificate, regardless of where the death occurred and whether the child received assistance, thus making it impossible for researchers to determine its cause.
For the statistical analysis, comparisons of frequencies between nominal variables were made using the chi-squared test without continuity correction. Tests with a probability of alpha error ≤ 0.05 were considered significant.
The study was approved by the Ethics Committee of Universidade Federal de Minas Gerais (UFMG) and Fundação Hemominas.
ResultsMarch of 1998 to February of 2012 (193 deaths)A total of 3,617,919 children were screened through the NSP-MG. Of these, 2,591 children had a hemoglobin profile compatible with SCD and 193 of them died (7.4%), of whom 97 (50.3%) were males. Regarding genotypes, 153 had SS/Sβ0 thalassemia (79.3%), 34 had SC- (17.6%), and six had Sβ+ -thalassemia (3.1%).
Most children who died 150 (77.7%) lived in urban areas of the municipalities. When the municipalities in the state of Minas Gerais that recorded deaths are considered, 98 of 378 children diagnosed with SCD (25.9%) died in the small municipalities, i.e., towns with up to 50,000 inhabitants. This is in contrast with the 93 deaths among 1,228 children (7.6%) from medium or large-sized municipalities, plus the large cities (p < 0.000001). Two children died out of the state.
The median age at blood collection for screening was 6 days; 75% of the children were screened at up to 8 days of life. The median age at the first visit to the Blood Bank Clinical Center was 1.4 months. Twelve children (6.2%) died prior to the first consultation; nine died before reaching 60 days, the maximum period of waiting until the first consultation in Blood Banks, mostly due to prematurity and its complications, according to the death certificates assessed by the researchers. Three children died at 105, 122, and 131 days of age, two of them with severe congenital cardiomyopathy. The other child died with acute splenic sequestration in the city of Vitória (ES), without undergoing the consultation at the Blood Bank in Valadares (MG); two families were interviewed by the researchers.
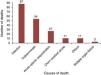
It was observed that 56.5% of deaths occurred in children younger than 2 years of age and 76.7% occurred in children younger than 5 years. The median age at death was 1.7 years. Fig. 1 shows the distribution by age range.
According to information obtained from the death certificates and interviews with family members, there was a prevalence of in-hospital deaths (78%), but the occurrence of 21 home (11%) and 19 in-transit (10%) deaths should be emphasized.
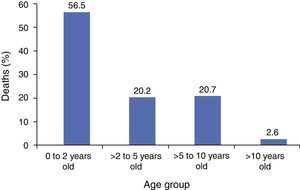
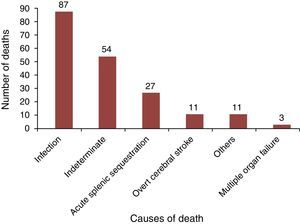
Infection, including septicemia, pneumonia/acute chest, and gastroenteritis, was the leading cause of deaths in this group (45%), followed by indeterminate causes (28%). Acute splenic sequestration (ASS) was the third cause of death (14%), as shown in Fig. 2. Among the children with SS/Sβ0-thalassemia, ASS was the cause of death in 17.6%.
Most children (75%) received medical care before death; however, the number of children that went unassisted (24%) was significant. There was no recording of the terms “SCD” or “SCA” as cause of death in a significant number of death certificates (46%).
March of 2005 to February of 2012 (117 deaths)The interviews (n = 84) showed that 46.4% of children were treated within the first 6hours after symptom onset during the event that caused the death; 64.3%, within 24hours; and 26.2% died without medical attention. Death occurred within 12hours of symptom onset in 30% of cases and, in 40.5%, within the first 24hours. Fever, pain, pallor, and vomiting were the most common initial symptoms related to death, as reported by family members. The hospital was the first health care service sought by approximately 60% of families, followed by Basic Health Units (12%).
After the first consultation, 30 children were referred to other care units, 24 by ambulance. Of these, three died during transfer and one died before transport arrived. Only 13.8% of the children were transported while on medication.
Regular use of prophylactic antibiotics and folic acid was reported by 90% of the families. Approximately 74% of the children received special immunobiologic agents. Regarding the clinical evolution prior to death, 58.3% of the children had been admitted to the hospital at least once and 23.8%, more than three times. Painful crisis had occurred in almost 60% of the children before the event which resulted in the death, and 46.4% had received transfusions. ASS had already occurred in 27.4% of the children.
Regarding the socioeconomic status of families, 91.6% had a monthly per capita income equal to or smaller than one minimum wage and 50% received federal benefits. As for education, 5% of the families were illiterate.
Only 54.8% of the families received regular visits of the Family Health Program (FHP) agents while the child was alive. The cognitive questionnaire applied to the families (n = 41) showed that 85.4% obtained over 60% of correct answers.
Considering the total of 1,733 appointments scheduled in blood centers for the 117 children who died, 359 appointments (20.7%) were not attended because the families failed to come. All appointments were rescheduled, but the control system does not inform the success of such procedure.
Comparisons between the study periodsIn the first seven years, a total of 1,399 children were screened and 76 deaths occurred until February 28, 2005, with a mortality rate of 5.43%. In the last seven years, 1,192 children were screened and 61 died, with a mortality rate of 5.12% (p = 0.72). In the first period, 55/76 deaths (72.4%) occurred before the age of 2 years; in the second period, 47/61 (77.0%, p = 0.53). The remaining 56 deaths, totaling 193, occurred in children born in the first seven years, but died in the second period and thus, were not included in the statistical calculations.
In the first seven-year period, 25.3% of the deaths occurred at home or in transit; in the second, the mortality rate decreased to 18.1% (p = 0.28). The lack of medical care at the time of death also decreased from 28.0% to 21.6% (p = 0.39). The mentioning of the term “sickle cell” in death certificates was significantly more frequent (60.5%) in the last seven-year period, when compared to the first period (42.1%, p = 0.017).
DiscussionThe sample reflects the overall health reality of children with SCD screened during the 14 years of the NSP-MG, as all deaths of children followed at Blood Bank Clinical Centers were informed. This represents the total number of deaths, which configures a population-based study.
The present study, as others,11,12 observed no significant difference between genders in the incidence of deaths in the assessed age range.
This and several other studies11,13–17 have demonstrated that the highest frequency of deaths occurred in patients with HbSS (79.3%), the most common and most clinically severe genotype. The relatively high frequency of deaths in children with Sβ+ thalassemia (6.5%) does not correspond to reality, as only from 2010 onwards all suspected cases of SCD in NSP-MG were confirmed by molecular biology techniques. The diagnosis of this subtype of SCD may be overestimated in the neonatal period due to blood transfusions not reported by family members or errors in the interpretation of small concentrations of HbA.
Three quarters of the children diagnosed between 2005 and 2012 underwent neonatal screening for SCD in up to 8 days of life, less time than the 18 days in the initial period between 1998 and 2005,10 which shows improvement of the NSP-MG.
The distribution of children per age range at the time of death shows increased occurrence of deaths in those younger than 5 years, similar to that observed by other authors.11,18–22 Nonetheless, some authors4,8,12,16,23,24 have reported that infant mortality rate due to SCD is decreasing and the median age of death is increasing. In the present study, the high mortality in children younger than 5 years is explained by the higher incidence of potentially fatal events in this age group, such as infections and ASS.
Although in-hospital deaths were the most prevalent, it is noteworthy that one-fifth of them occurred at home or in-transit. This can be explained by several factors, such as family residence located far from the health service, difficulty getting to the service, low socioeconomic and educational levels, in addition to the family's incapacity to identify risk situations for the child. The statistically non-significant increase of 11% in the number of in-hospital deaths shows improvement, albeit small, in the health care of children with SCD in the last six years. A study conducted in Angola25 concluded that patients with SCD who lived in the countryside or in rural communities were three times more likely to die during hospitalization, due to socioeconomic factors and lack of immediate access to medical care.
In the present study, as in many others,11,14,15,18,25–27 infection appears as the main cause of death, considering the age groups studied. The high number of indeterminate causes suggests a difficulty for physicians and health care professionals to recognize SCD and its severe acute events determinants of death, as in the study by Alves,28 given that most of the records came from in-hospital deaths. ASS was the third most common cause, which reflects the difficulty by health teams and families to identify this complication. The proportion of deaths caused by ASS in SS children was similar to that reported in a previous study, restricted to SS children.29 Other authors13,15,19 indicated ASS as the main cause of death in children younger than 3 years.
A significant number (46%) of death certificates did not mention the term “sickle cell” as the cause of death. However, the number of certificates that mention this term has increased significantly over the past seven years, indicating greater visibility and awareness of the disease by physicians.
Most children received medical care before death, but 25% of them were unassisted. An increase, albeit non-significant, of 13% in the frequency of medical care provided to children with SCD before death was observed, which once again indicates a probable increase of the knowledge about SCD by physicians.
Medical care occurred within the first 6hours in almost half the cases and two-thirds in the period of up to 24hours. Death occurred within the first 24hours of symptom onset in approximately 40% of cases. Manci et al.15 demonstrated that the first 24hours after the onset of the pathological process represent the period of greatest risk of death for patients with SCD. This emphasizes how fast the clinical condition worsens, culminating in death.
High adherence to antibiotic prophylaxis and folic acid, in addition to the regular use of special immunobiologic agents indicates that these data may be overestimated, as they were obtained a posteriori and in the presence of an “authority figure”, i.e., the interviewer. A study conducted at the Blood Bank Clinical Center of MG showed lower levels of adherence to antibiotic prophylaxis.30 The incorporation of “special vaccines” to the basic vaccination schedule occurred only recently, and may have contributed to the low adherence of families. This is probably due to the lack of awareness by health professionals regarding the special immunization schedule and the lack of priority when requesting special immunobiologic agents by the municipalities.
At the time of the child's death, only little more than half of the families regularly received visits from the FHP team. Considering that SCD is a chronic disease with the possibility of severe acute events, in addition to the fact that it affects low-income families, better monitoring by the FHP through home visits was expected, in order to ensure the inclusion of these patients in the health care system.
Lack of priority and/or delay in treatment, lack of knowledge by the team and poor health service infrastructure were difficulties reported by the families that may have contributed to death. Low parental educational level and low income constitute additional barriers. A study conducted in Gabon, Africa,21 also reported that the vast majority (91.3%) of children with SCD who died were from families of low socioeconomic status. Inadequate transport conditions were also reported by some families, such as oxygen cylinder with insufficient or absent volume for the entire transfer, inadequate oxygen mask size for the child, among others.
The cognitive questionnaire administered to 41 families indicates that knowledge about SCD is still precarious, even after the occurrence of such an important event as the death of a child.
The main limitation of the study was its retrospective design, as locating the families becomes more difficult over the years, as well as their incapacity to accurately report some of the data. The interviews added a more accurate qualitative character to the study, rather than a simple assessment of death certificates. In the authors’ opinion, the absence of 33 interviews, in 117, did not impair the desired goals.
It can be concluded that low socioeconomic and educational levels of families, difficulties in access to health services, lack of transportation, lack of priority in health care, and lack of knowledge about SCD by health professionals were aggravating factors for the clinical status of the child.
Screening for SCD, even when performed in a comprehensive and effective way, was still not enough to reduce the mortality rate observed at the NSP-MG. Social and economic development in the state are necessary to change this scenario. Care of acute events, consultations with specialists, adequate transportation of patients, and continuing education for families and health care teams should be recognized as a priority in the care of patients with SCD.
FundingConselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Núcleo de Ações e Pesquisa em Apoio Diagnóstico (Nupad).
Conflicts of interestThe authors declare no conflicts of interest.
To all the families who agreed to be interviewed in their homes, despite the grief aroused by the remembrance of their children's death. To NUPAD/UFMG, for logistical and financial support at the different stages of the research. To CNPq, which used part of the proceeds from the Universal Demand Project No. 471019/2011-9 to allow the performance of some visits for data collection. To Dr. Ana Paula Fernandes Pinheiro Chagas for suggesting the topic, as well as her assistance and encouragement at all stages of the research.
Please cite this article as: Sabarense AP, Lima GO, Silva LM, Viana MB. Characterization of mortality in children with sickle cell disease diagnosed through the Newborn Screening Program. J Pediatr (Rio J). 2015;91:242–7.
Study conducted at Núcleo de Ações e Pesquisa em Apoio Diagnóstico (Nupad), Faculdade de Medicina, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil.