Sickle cell disease is a global health problem that affects>300,000 newborns per year, predominantly in Sub-Saharan Africa,1 where mortality is estimated to be>50% by age 5 years for those with homozygous hemoglobin S (HbSS).1 In Brazil, there are estimated to be>30,000 individuals with sickle cell disease and 2,500 newborns per year, making this the most common genetic disorder in the country.2 Advances in the management of sickle cell disease in the United States have led to a decline in mortality from about 26% to approximately 1-2% in the first 18 years of life, with the greatest progress demonstrated by a flattening of the mortality peak in the ages of 1-4 years from 13% to 2%.3,4 Much of this progress resulted from the implementation of universal newborn screening in all 50 states in the U.S. following publication of the results of the prophylactic penicillin study, which demonstrated a dramatic reduction in sepsis and mortality due to S. pneumonia in the first five years of life.5
Remarkable progress has also occurred in Brazil over the past two decades, during which newborn hemoglobinopathy screening was initiated in Campinas (1992), Minas Gerais (1998), Rio de Janeiro (2001), Pernambuco (2003), and other locations.6–9 This expansion of neonatal screening was promoted by a decree from the Brazilian Ministry of Health in 2001, calling for a multi-phased implementation of screening for congenital disorders including hemoglobinopathies. This effort resulted in a report in 2010 describing the remarkable heterogeneity in the prevalence of sickle cell trait (HbAS, 1.1-9.8%) and sickle cell anemia (HbSS, 2.2-172/100,000 population) in different regions of the country.2 The report from the Federal University of Minas Gerais in Belo Horizonte by Sabarense et al. in this issue of the Journal updates the results of neonatal hemoglobinopathy screening in this state.10 Disappointingly, the authors found no significant difference between the mortality rate in children born between March of 1998 and February of 2005 (5.4%) and those born between March of 2005 and February of 2012 (5.1%) (p=0.72). Characteristics of the 193 children who died in the combined period (1998-2012) included: residence in smaller towns, age less than 2 years (56.5%), median age at death 1.7 years, 22% of deaths occurring outside of the hospital (at home or while in transit), and remarkably low socioeconomic status of families (91.6% monthly per capita income ≤ minimum wage. In the first period, 72% of the deaths occurred before age 2 years, compared with 77% in the second period. Overall, the major causes of mortality were infection (including septicemia, acute chest syndrome, and gastroenteritis, 45%), “indeterminate” perhaps due to a lack of awareness of the underlying diagnosis (28%), and acute splenic sequestration (14%). Although it is not clear from the data as presented, a substantial portion of the infectious deaths were related to “pneumonia/acute chest syndrome”, which was also the leading cause of mortality in the report from the HEMORIO Center in Rio de Janeiro.11 No recording of the terms “sickle cell disease” or “sickle cell anemia” as a cause of death was found in 46% of the death certificates. Mortality occurred within the first 24hours in more than 40% of patients. In the later time period, there was a slight reduction in the proportion of patients whose death occurred at home or in transit, and a slight increase in the death certificates which mentioned the term “sickle cell”. Overall, the unchanged mortality rate in the first five years of life, and the continued occurrence of infection and splenic sequestration as the major causes of mortality, indicated that newborn screening for sickle cell disease, even when performed in a comprehensive and effective manner, was insufficient by itself to greatly modify the course of the disease.
What can be done to improve mortality in developing countries around the globe, in which increasing resources and interventions for the care of persons with sickle cell disease are becoming available? Sabarense et al. suggested that “social and economic development” in Minas Gerais was necessary to change the scenario.10 Consideration should be given to several areas in which preventive care for children with sickle cell disease and education of families may be improved. In September of 2014, the Expert Panel guidelines (Evidence-Based Management of Sickle Cell Disease) from the National Heart, Lung, and Blood Institute of the U.S. National Institutes of Health were published.12 These included recommendations in the areas of penicillin prophylaxis, pneumococcal immunization, appropriate response to fever, recognition and management of acute splenic sequestration, and prevention of stroke through transcranial Doppler ultrasonography (TCD) screening. For example, the panel had strong recommendations for the prevention of invasive pneumococcal infection, including the administration of oral penicillin prophylaxis for all children with HbSS at least until age 5, vaccination against pneumococcus for sickle cell patients of all ages, including a detailed vaccination schedule for PCV13 (Prevnar13) and PPSV23 (Pneumovax), and education of families and caregivers about the necessity to seek immediate medical attention whenever significant fever (temperature>38.5°C) occurs. These guidelines also made strong recommendations about the need for screening for increased stroke risk through TCD examinations according to a specified schedule. In the management of acute splenic sequestration, the guidelines acknowledged that there were no randomized clinical trials to provide an evidence base, but the need for education of families and healthcare providers regarding recognition of the symptomatology associated with splenic sequestration and the necessity for emergent management was emphasized.
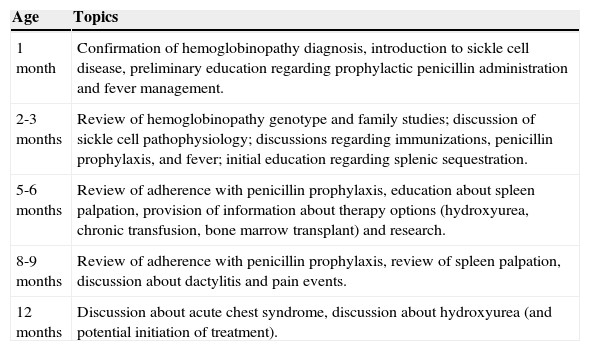
How can these recommendations be translated into comprehensive and consistent practice that will lead to diminished mortality in Minas Gerais and other regions around the globe with similar sickle cell populations and healthcare resources? One approach is to utilize a plan of care for sickle cell disease, which details the expectations at each clinic visit according to the age of the patient, thereby creating standardized expectations for both families and healthcare providers. For example, at our institution infants with sickle cell disease are managed with the goals in the Table 1 (among other goals) when they are seen at routine clinic appointments in the first year of life.
Plan of care for infants with sickle cell disease in first year of life.a
| Age | Topics |
|---|---|
| 1 month | Confirmation of hemoglobinopathy diagnosis, introduction to sickle cell disease, preliminary education regarding prophylactic penicillin administration and fever management. |
| 2-3 months | Review of hemoglobinopathy genotype and family studies; discussion of sickle cell pathophysiology; discussions regarding immunizations, penicillin prophylaxis, and fever; initial education regarding splenic sequestration. |
| 5-6 months | Review of adherence with penicillin prophylaxis, education about spleen palpation, provision of information about therapy options (hydroxyurea, chronic transfusion, bone marrow transplant) and research. |
| 8-9 months | Review of adherence with penicillin prophylaxis, review of spleen palpation, discussion about dactylitis and pain events. |
| 12 months | Discussion about acute chest syndrome, discussion about hydroxyurea (and potential initiation of treatment). |
An important recommendation of the Expert Panel report calls for increased use of hydroxyurea. Recent long-term follow-up reports of adult patients with sickle cell anemia from the U.S. Multi-center Study of Hydroxyurea (MSH) and the LaSHS study (Laikon Study of Hydroxyurea in Sickle Cell Syndromes) in Greece have shown substantial reduction in mortality related to the use of this drug.13,14 More similar to the population described by Sabarense et al.10 is the cohort from Rio de Janeiro, which included 1,760 subjects, ages 3-18 years, 267 of whom received hydroxyurea for a median of two years.11 Survival among the children treated with hydroxyurea was significantly greater than among the untreated (99.5 vs. 94.5%, p=0.01), primarily due to fewer deaths from acute chest syndrome and infection, and these patients had significantly fewer hospitalizations and emergency room visits. Toxicity was predominantly mild, reversible neutropenia. It was concluded that hydroxyurea reduces morbidity and is associated with decreased mortality in children with sickle cell disease. All three of the above studies were retrospective, but the BABY HUG study (Pediatric Hydroxyurea Phase III Clinical Trial), a multi-center prospective randomized double-blinded trial, demonstrated that infants receiving hydroxyurea had substantial clinical benefit from reduction of pain, dactylitis, acute chest syndrome, hospitalization, and transfusion, as well as significant increases in hemoglobin, mean corpuscular volume (MCV), and hemoglobin F levels.15 In part due to these data, the recommendation of the Expert Panel was: “In infants 9 months of age and older, children, and adolescents with sickle cell anemia, offer treatment with hydroxyurea regardless of clinical severity to reduce SCD-related complications (e.g., pain, dactylitis, acute chest syndrome, anemia)”. This was a “strong” recommendation with “high quality evidence” for ages 9-42 months, and a “moderate recommendation” with “moderate quality evidence” for children greater than 42 months and adolescents. Of note, the panel intentionally used the term “offer”, realizing that the patients’ and their caretakers’ values and preferences may differ particularly considering treatment burden (e.g., laboratory monitoring, office visits), availability of drug in a liquid form, and cost. Therefore, the panel strongly encouraged shared decision-making and discussion of hydroxyurea therapy with all patients and families. In addition, the Expert Panel provided a consensus treatment protocol for the implementation of hydroxyurea therapy. This recommendation, in conjunction with the data, albeit retrospective, from HEMORIO, suggest that hydroxyurea could have a major long-term benefit in decreasing mortality in children with sickle cell disease in Minas Gerais, as well as in other regions of the world where sickle cell healthcare is developing. Of course, there remain numerous barriers that must be overcome to accomplish widespread and proper utilization of hydroxyurea treatment, including providing appropriate education to both healthcare providers and families regarding the benefits and risks of the drug, the availability of clinics and laboratories that can provide the necessary infrastructure for regular evaluation of patients on treatment, and adequate financial support from the Health Ministry and other sources. One incentive for government support of the expanded use of hydroxyurea is the cost savings that result, primarily through decreased hospitalization, which more than offsets the increased cost of outpatient management and the cost of the drug itself.16 In addition, there remain questions to be addressed regarding the use of hydroxyurea in children with sickle cell disease, such as whether a fixed dose of the drug (at 20mg/kg/day) or an escalation to maximum tolerated dose (MTD) provides a greater benefit-risk ratio.17 An additional consideration might be “low dose” hydroxyurea, which might require less monitoring in a resource-limited environment.18
Can the approaches described above make a difference? It will be interesting to see the data on mortality in children with sickle cell disease in Minas Gerais in another ten years.
Conflicts of interestThe author declares no conflicts of interest.