The first time I heard someone talk about zero tolerance toward death from asthma was at the World Allergy Organization (WAO) International Scientific Conference in Dubai in 2010. I was impressed by the vigor with which Professor Tari Haahtela presented the results obtained with the use of health education plans in the prevention of asthma mortality in Finland. Gary Wong had just affirmed the same concept in a different context.1 Under all the heavens then, including that of Latin America,2 there is no greater cost than the preventable death of a patient, in particular among children.
After its rise from a rate of 0.45/100,000 in 1974/5 to a peak rate of 0.62/100,000 in 1985/6, the mortality from asthma across the world has declined. In 2004/5, the mortality in developed countries – including the United States, Canada, New Zealand, Australia, Western Europe, Hong Kong, and Japan – was reduced to a rate of 0.23/100,000. This reduction was associated to the increasing use of inhaled corticosteroids.3
The drop in mortality has coincided with the introduction of increasingly precise guidelines for the management of asthma internationally and in specific countries, with the development of educational plans for practitioners, pharmacists, and other health professions, and with their implementation by the health authorities of each country.
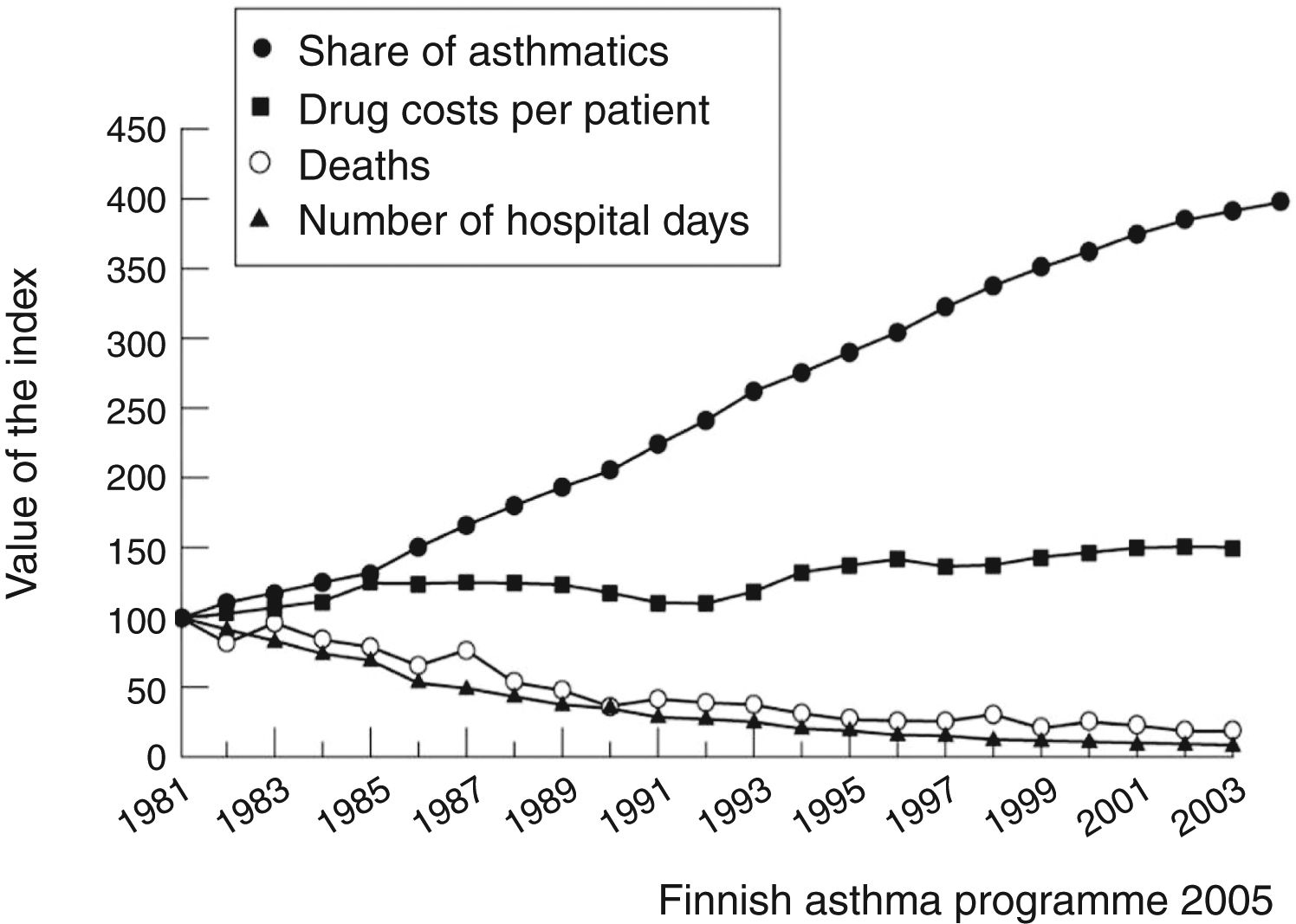
The prototype for models of disease management remains the Finnish asthma management program, which produced a huge effect in reducing asthma mortality and morbidity over the period 1994–2004. It was centered on early diagnosis, active anti-inflammatory treatment immediately after the diagnosis, information on the disease and its treatment, self-management, and effective networking among specialists, primary care physicians, and pharmacists. This program resulted in a reduction in asthma deaths from 100 to less than 20 per year in the Finnish population of 5 million, which could be largely attributed to early and more effective use of anti-inflammatory medication, especially inhaled corticosteroids (Fig. 1).4,5
Other countries (Australia, Ireland, Canada, Poland, Tonga, South Africa, New Zealand) followed the Finnish example, developing their own national asthma reduction strategies with good success.2,6 In Europe, the integrated plan ‘European Asthma Research and Innovation Partnership’ (EARIP) has been also put in place to harmonize asthma education activities across the continent, in order to develop a comprehensive approach focused on asthma control, to reduce asthma-related mortality and morbidity.7 Its ambition is to reduce asthma mortality in Europe by 25% within ten years and by 50% within 20 years.
Despite all the progress made with early therapeutic intervention, an incompressible mortality rate remains, even when the possibilities offered by conventional anti-inflammatory drugs have been saturated (Fig. 1). In developed countries, we are now experiencing signals of upward rebound in mortality,8 together with an increase in corticosteroid-induced adverse events in severe asthma patients,9 while the mortality from asthma has not been eliminated anywhere.
This scenario is applicable to some parts of Brazil, but not to the whole country. The data published in this issue of the Jornal10 are of particular interest as they arise from a solid reporting system in a young age range, where asthma mortality can be very accurately tracked due to absence of confounding diagnoses.11 In Brazil, the reduction in asthma mortality over 20 years is conspicuous, testifying to the great progress in pediatric pulmonology care in that country. The most important reduction was achieved in the group of children under the age of 4 years, which, however, remains the group that most contributes to asthma mortality in 2015. Indeed, the mortality for asthma in Brazilian children has not reached an optimal low level countrywide. Some areas of higher mortality still persist, in particular among children under 10 years of age and in some geographical areas, such as the North and the Northeast.10
The study calls for two areas of possible intervention: adolescents and preschoolers.
Brazilian adolescents with asthma incur the risk of under-hospitalization during attacks,10 perhaps as part of their denial of the disease, noncompliant therapeutic behaviors, smoking, and psychosocial issues. Some of these conditions are ameliorable with specific educational interventions, targeted toward the reasons for poor control of asthmatic symptoms: underestimation by patients and physicians, under-treatment – especially with anti-inflammatory drugs, overuse of bronchodilators in case of attacks, low compliance to medications, and poor skills in the use of prescribed devices.12 An important part could be the use of the now-available Portuguese version of the Test for Respiratory and Asthma Control in Kids (TRACK).13 A substantial part of the causes (for instance, low-income households14,15) would require complex interventions.
Of note, 68% of reported deaths happened in children under 4 years of age.10 In this age range, uncertainties remain about the possibility of labeling a child as asthmatic.16 We fully agree with the authors’ opinion that in preschool age asthma must be considered as such, beyond the difficulties of definition. Under its multifaceted phenotypes,17 preschoolers experience severe wheezing episodes resulting in emergency room visits, hospitalization, and oral steroid courses. Preschoolers merit asthma treatment, as an early intervention may decrease the number of exacerbations and promote lung growth. As part of this intervention, educational plans must not be spared.
A considerable obstacle for the realization of educational plans could be the territorial vastness and the socioeconomic heterogeneity of Brazil. This nation has one of the highest rates of inequality in the world, and the Gini index, measuring economic inequality within countries, has been associated with a high prevalence of allergies and asthma.18 It is also a country with high prevalence of sensitization to perennial allergens, associated with asthma mortality.19 However, Brazil offers opportunities for educational plans. It is the fifth country in smart phone usage in the world: as 54% of Brazilian adults own a smart phone, and families often share one device, it can be estimated that 120 million Brazilians have access to the internet.20 This could offer the infrastructural opportunities for modern, digital health-based interventions.21 An additional effort will be necessary on the part of the Brazilian medical community and health authorities to address, together with the health problems, the social issues that can be glimpsed under the data of the present study. After all, it is a question of facing one of the many aspects of the fragility of children in the preschool age and in adolescence, which recalls the need for recognition, care, and education.
Every asthma death is one too many. The interest of their Jornal shows that Brazilian pediatricians are ready to take up this challenge.
Conflicts of interestThe authors declare no conflicts of interest.