Approximately 6% of all cancers arise in adolescents and young adults. Currently, the ward type best placed to treat this patient group remains controversial. The aim of this study was to evaluate exactly where adolescents and young adults with cancer are treated in Brazil.
MethodsData were extracted from 271 Brazilian hospital-based cancer registries (2007–2011), including all five national regions (North, Northeast, Midwest, South, and Southeast). Variables included gender, age, ethnicity, National Code of Health Establishment, hospital unit state, and region. Tumors were classified according to the World Health Organization classification for adolescents and young adults with cancer. Odds ratios with 95% confidence intervals were computed by unconditional logistic regression.
ResultsMost patients were managed on medical oncology wards, followed by pediatric oncology and then by non-specialist wards. Of patients aged 15–19 years, 49% were managed on pediatric wards; most of the older patients (96%; aged 20–24) were managed on adult wards. Patients were more likely to be seen in medical oncology wards as their age increased (OR=2.03 [1.98–2.09]), or if they were based in the South (OR=1.50 [1.29–1.73]). Conversely, bone tumors were less likely to be treated (decreased OR) on medical oncology wards, regardless of age, gender, and region.
ConclusionAn elevated risk of treatment on medical oncology wards was observed for older patients and those treated in the South. Bone tumors were generally treated in pediatric oncology wards, while skin cancers were treated in medical oncology wards, regardless of age, gender, and region.
Aproximadamente 6% de todos os cânceres surgem em adolescentes e adultos jovens. Atualmente, o melhor tipo de enfermaria para tratar esse grupo de pacientes continua sendo controverso. O objetivo deste estudo foi avaliar exatamente onde os adolescentes e adultos jovens com câncer são tratados no Brasil.
MétodosForam coletados dados de 271 registros de câncer de base hospitalar (2007-2011), inclusive de todas as cinco regiões nacionais (Norte, Nordeste, Centro-Oeste, Sul e Sudeste). As variáveis incluíram sexo, idade, etnia, o Código Nacional de Estabelecimento de Saúde e o estado e a região da unidade hospitalar. Os tumores foram classificados de acordo com a classificação da Organização Mundial de Saúde para adolescentes e adultos jovens com câncer. As razões de chance com intervalos de confiança de 95% foram calculadas por regressão logística incondicional.
ResultadosA maioria dos pacientes foi tratada em enfermaria de oncologia médica, seguido da enfermaria de oncologia pediátrica e, então, a enfermaria sem especialidade. 49% dos pacientes com idades entre 15-19 anos foram tratados em enfermarias pediátricas; os pacientes mais velhos (96%, com idades entre 20-24) foram tratados em enfermarias de adultos. Os pacientes apresentaram maior propensão a serem vistos em enfermarias de oncologia conforme mais velhos (RC=2,03 [1,98-2,09]) ou caso morassem na região Sul (RC=1,50 [1,29-1,73]). Por outro lado, os tumores ósseos mostraram menor propensão a tratamento (redução da RC) em enfermarias de oncologia, independentemente da idade, sexo e região.
ConclusãoFoi visto um risco elevado de tratamento, em enfermarias de oncologia, de pacientes mais velhos e os tratados na região Sul. Os tumores ósseos foram, em geral, tratados em enfermarias de oncologia pediátrica, ao passo que os cânceres de pele foram tratados em enfermarias de oncologia médica, independentemente da idade, sexo e região.
Currently, no clear age definition exists in the literature for the patient group comprising adolescents and young adults (AYA). The World Health Organization (WHO) defines adolescence as the age bracket of 10–19 years, whereas the United Nations (UN) uses 15–24 years of age to define adolescence, using the term “young adult” to refer to those aged 20 and over.1 The Brazilian Children and Adolescents Statute defines adolescence as 12–18 years of age.2
The incidence of cancer in the AYA group has increased when compared with other age groups. Approximately 6% of all cancers now arise in AYA patients (aged 15–29 years); this incidence is 2.7-fold greater than in younger patients (aged<15 years.).3 In Brazil, the median incidence of cancer in this population is 218 cases per million for male patients, and 232 cases per million in female patients; the majority of cases is diagnosed as carcinomas, lymphomas, and leukemias.4
The AYA age group lies at the boundary of pediatric and medical oncology, and manifests unique biological and clinical characteristics. Pediatric tumors are mostly embryonic, while tumors in older adults tend to originate from epithelial tissue. The spectrum of cancer type therefore differs when comparing younger children and adults, which reflects the different pathologic mechanisms involved, as well as tolerance and response to therapy. Consequently, there is a growing awareness of the need for specialist adolescent treatment units within pediatric wards.
One of the considerable challenges with regard to cancer treatment for the AYA population is in determining where best to treat these patients, given the heterogeneity in biological/clinical behavior when comparing pediatric and medical oncology. Dedicated units specialized in treating AYA patients are needed, especially given the lack of any improvement in survival for this group when compared with children or adults aged 29 years of age and above.5 This disappointing failure to improve therapy for the AYA patient group may reflect a poor recognition of, and a lack of specialist attention to, the unique pathobiology exhibited by these patients, together with inadequate support for their psychosocial needs.6–9
The optimal treatment site for AYA patients remains controversial.10–13 Referral to pediatric wards appears to be associated with age, type of cancer, and the distance to pediatric oncology centers.14–16 Ideally a specialist adolescent cancer unit would be used. In Brazil, data on where AYA patients are treated is lacking. This shortcoming hampers the improvement of institutional practice and the development of specific treatment protocols.13
The aim of this study was to determine where the oncologic care for AYA patients takes place in Brazil.
Materials and methodsData sourcesData were extracted from thirteen thousand four hundred and seventeen cases of cancer in AYA patients aged 15 to 24 years from 271 Brazilian hospital-based cancer registries (BHCR; 2007–2011) across the five main regions of Brazil (North, Northeast, Southeast, South, and Midwest; data extracted from the Integrator System [IS – http://www.inca.gov.br]). Patient information from each registry included: gender, age, National Code of Health Establishment (NCHE), type of hospital unit, and geographic region. Tumors were classified according to the WHO AYA cancer classification.17 Data collection was by telephone contact with each hospital unit to determine the presence (or not) of a pediatric oncology ward, as well as the age group admitted by the ward.
Statistical analysesAll variables were subject to descriptive analyses. Crude and adjusted odds ratios (OR) with 95% confidence intervals (CI) were obtained by logistic regression analyses with gender, region, and AYA classification included as categorical variables. Patient age was included as a continuous variable (per year of age increase). Reference categories for variables were female, the Southeast region, and leukemia. All analyses were conducted using SPSS (IBM SPSS Statistics for Windows, version 20.0, NY, USA).
This study was approved by the Research Ethics Committee of Instituto Nacional de Câncer José Alencar Gomes da Silva (INCA).
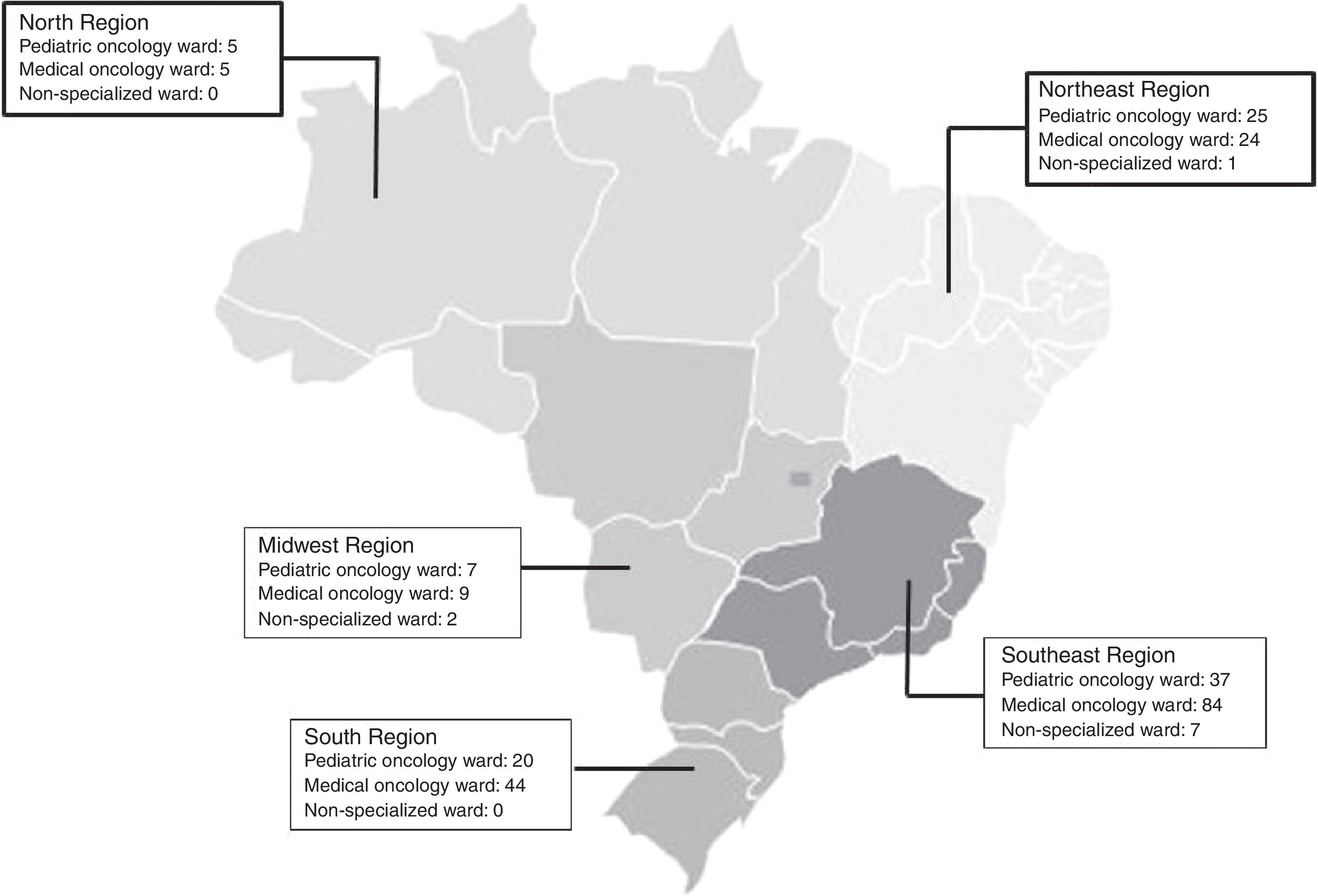
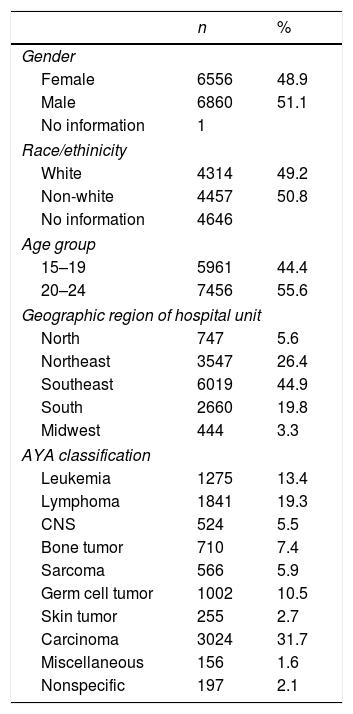
ResultsSociodemographic and tumor characteristics for this patient cohort are presented in Table 1. The majority of patients were diagnosed with carcinomas, then lymphomas, and leukemias. Most patients were managed in medical oncology wards (n=9399), followed by pediatric oncology wards (n=2907), and then by non-specialist wards (n=146). The Southeast region had the highest number of hospital units with pediatric oncology wards (n=37/28%), most specifically in São Paulo. The North and Northeast regions had the highest proportion of pediatric oncology wards, in 50% of their hospital units (Fig. 1). In 81 of 94 pediatric oncology wards, patients were aged 0–18 years (n=37/81; 45.7%). For patients aged 15–19 years, 49.6% of cases were managed in pediatric wards, while for those aged 20–24 years, the majority (96.1%) were referred to adult wards. For those aged 15–19, bone tumors (61%), central nervous system tumors (55.8%), and leukemias (53%) were managed, in general, in pediatric wards. In contrast, approximately 56% of carcinomas were managed in medical oncology wards.
Sociodemographic and tumor characteristics of adolescent and young adult (AYA) patients in Brazilian cancer hospital registries (2007–2011).
| n | % | |
|---|---|---|
| Gender | ||
| Female | 6556 | 48.9 |
| Male | 6860 | 51.1 |
| No information | 1 | |
| Race/ethinicity | ||
| White | 4314 | 49.2 |
| Non-white | 4457 | 50.8 |
| No information | 4646 | |
| Age group | ||
| 15–19 | 5961 | 44.4 |
| 20–24 | 7456 | 55.6 |
| Geographic region of hospital unit | ||
| North | 747 | 5.6 |
| Northeast | 3547 | 26.4 |
| Southeast | 6019 | 44.9 |
| South | 2660 | 19.8 |
| Midwest | 444 | 3.3 |
| AYA classification | ||
| Leukemia | 1275 | 13.4 |
| Lymphoma | 1841 | 19.3 |
| CNS | 524 | 5.5 |
| Bone tumor | 710 | 7.4 |
| Sarcoma | 566 | 5.9 |
| Germ cell tumor | 1002 | 10.5 |
| Skin tumor | 255 | 2.7 |
| Carcinoma | 3024 | 31.7 |
| Miscellaneous | 156 | 1.6 |
| Nonspecific | 197 | 2.1 |
CNS, central nervous system tumors.
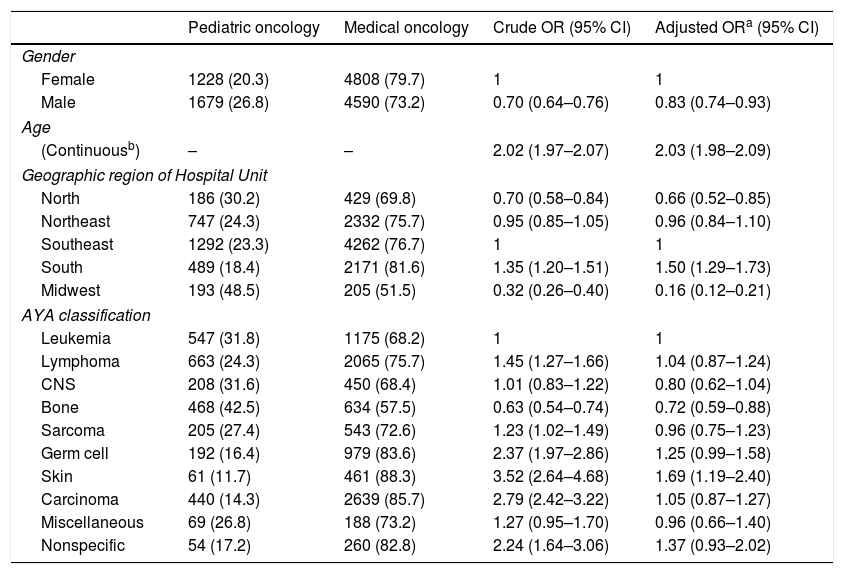
Table 2 shows the crude and adjusted ORs with 95% CIs for the site of patient treatment in terms of gender, age, region, and tumor type. Age, used as a continuous variable, showed (per year of increase) an independent association with medical oncology ward (OR=2.02 [95% CI: 1.97–2.07]). Bone tumors revealed a decreased chance of treatment on a medical oncology ward irrespective of gender, age, and region (OR=0.72 ([95% CI: 0.59–0.88]). Among patients from the South (region) of Brazil, there was an increased risk of being treated on a medical oncology ward (OR=1.50 [95% CI: 1.29–1.73]) while patients from the North (OR=0.66 [95% CI: 0.52–0.85]) were more likely to be treated on a pediatric oncology ward regardless of tumor type, age, or gender.
Risk estimate for treatment on a medical oncology ward by sociodemographic and tumor characteristics (data retrieved from Brazilian cancer hospital registries for 2007–2011).
| Pediatric oncology | Medical oncology | Crude OR (95% CI) | Adjusted ORa (95% CI) | |
|---|---|---|---|---|
| Gender | ||||
| Female | 1228 (20.3) | 4808 (79.7) | 1 | 1 |
| Male | 1679 (26.8) | 4590 (73.2) | 0.70 (0.64–0.76) | 0.83 (0.74–0.93) |
| Age | ||||
| (Continuousb) | – | – | 2.02 (1.97–2.07) | 2.03 (1.98–2.09) |
| Geographic region of Hospital Unit | ||||
| North | 186 (30.2) | 429 (69.8) | 0.70 (0.58–0.84) | 0.66 (0.52–0.85) |
| Northeast | 747 (24.3) | 2332 (75.7) | 0.95 (0.85–1.05) | 0.96 (0.84–1.10) |
| Southeast | 1292 (23.3) | 4262 (76.7) | 1 | 1 |
| South | 489 (18.4) | 2171 (81.6) | 1.35 (1.20–1.51) | 1.50 (1.29–1.73) |
| Midwest | 193 (48.5) | 205 (51.5) | 0.32 (0.26–0.40) | 0.16 (0.12–0.21) |
| AYA classification | ||||
| Leukemia | 547 (31.8) | 1175 (68.2) | 1 | 1 |
| Lymphoma | 663 (24.3) | 2065 (75.7) | 1.45 (1.27–1.66) | 1.04 (0.87–1.24) |
| CNS | 208 (31.6) | 450 (68.4) | 1.01 (0.83–1.22) | 0.80 (0.62–1.04) |
| Bone | 468 (42.5) | 634 (57.5) | 0.63 (0.54–0.74) | 0.72 (0.59–0.88) |
| Sarcoma | 205 (27.4) | 543 (72.6) | 1.23 (1.02–1.49) | 0.96 (0.75–1.23) |
| Germ cell | 192 (16.4) | 979 (83.6) | 2.37 (1.97–2.86) | 1.25 (0.99–1.58) |
| Skin | 61 (11.7) | 461 (88.3) | 3.52 (2.64–4.68) | 1.69 (1.19–2.40) |
| Carcinoma | 440 (14.3) | 2639 (85.7) | 2.79 (2.42–3.22) | 1.05 (0.87–1.27) |
| Miscellaneous | 69 (26.8) | 188 (73.2) | 1.27 (0.95–1.70) | 0.96 (0.66–1.40) |
| Nonspecific | 54 (17.2) | 260 (82.8) | 2.24 (1.64–3.06) | 1.37 (0.93–2.02) |
CNS, central nervous system tumors.
The incidence of cancer in the AYA patient group is higher than for children aged less than 15 years,3 with carcinomas, lymphomas, and leukemias being the most frequent tumor types in Brazil.4 How and where these patients are treated remain controversial issues that are further confused by the lack of clarity in defining this patient population. With these problems in mind, the authors sought to collate data for how this patient group is diagnosed and treated in Brazil.
The tumors most frequently registered in the BHCRs were similar to those described in population-based cancer registries, and consisted of carcinomas, lymphomas, and leukemias. Thyroid and cervical carcinoma were the most frequent in the AYA age group, with the latter tumor type predominant in young Brazilian women. The median incidence rate of cervical carcinoma in the AYA patient group, according to Brazilian population-based data, was 2.11 cases per 100,000 women aged 20–24 years.18 Thyroid tumors, which occur more frequently in female patients, showed a median incidence rate of 13.7 cases per million.4
The present data revealed that the majority of AYAs aged 15–24 years were managed on medical oncology wards; increasing age was shown to be a significant risk factor for being treated on this type of ward. The confusion wrought by the varying age definitions for the AYA patient group is reflected by a lack of standardization among the different hospital units. One limitation of this study is that there is no information on whether a patient admitted to an adult ward is always followed by an adult oncologist, mainly in hospital units that have both services (pediatric and adult oncology). Accordingly, some authors report that most AYAs with a cancer diagnosis are treated by non-pediatric oncologists.13,19
The medical, physical, psychological, and emotional needs vary for different patient groups, which poses a distinct challenge when deciding where AYA patients should be treated. Consequently, a multidisciplinary team is mandatory, and an oncologist with medical and psychosocial expertise relevant to this age group should be involved. Standardizing the site and type of care available to AYA patients with a cancer diagnosis may help to improve outcomes for this patient group, given that the spectrum of cancers for AYA and pediatric patients differs. Further, it is recognized that pediatric and adult cancers are best treated with protocols and centers dedicated to those patient groups. In the present population, pediatric tumor types such as bone and leukemia were more likely to be managed on a pediatric ward, while carcinomas and lymphomas were managed on adult wards.
The biological characteristics of tumors diagnosed in AYA patients present heterogeneous responses to different protocols; it is suggested that adherence to treatment is improved when patients are treated on pediatric wards. However, the lack of participation and exposure of AYA patients to clinical trials and protocols20–22 may explain, in part, the limited treatment options available for this age group, as improved protocols and therapies generally require trial participation and the subsequent development of well-established multidisciplinary protocols.16,19
The majority of reports observed improved results when treatment is performed on a pediatric oncology ward when compared with adult wards.23 A meta-analysis performed in 2012 assessing 11 publications revealed that AYAs treated with pediatric protocols achieved superior outcomes than those treated with adult protocols.10 Previous studies performed in different countries (United States, United Kingdom, and the Netherlands) demonstrated that in the setting of AYA patients with Acute Lymphoblastic Leukemia (ALL), treatment according to pediatric protocols showed a superior outcome compared to adult protocols.10,24–26 Regarding the treatment of other tumors, such as Ewing's sarcoma, it was also demonstrated that adolescents older than 15 years of age treated in pediatric wards presented an improved survival when compared with those treated on non-pediatric wards, despite receiving the same treatment protocol.27 The underlying reasons for these disparate outcomes remain unclear. However, a definitive association between medical specialty and outcome for adolescents with cancer has been demonstrated, despite the fact that the present study did not evaluate responses to specific treatments or protocols.
Confusingly, some studies have shown no differences in survival rates for specialized wards, as well as improved survival rates for AYA patients treated on adult oncology wards.19,28 The authors believe that these discrepancies may relate to the histological type of tumor. For example, carcinomas and skin tumors are more specific to adults and are best handled on medical oncology wards. In turn, bone tumors, as a tumor type, have also been shown to be a protective factor in terms of referral to medical oncology wards. According to GLOBOCAN (International Agency for Research on Cancer), this histological group of tumors comprises 5% of all neoplasias in the population aged 0–19 years. In other words, bone tumors are strongly associated with younger patients and therefore tend to be treated in pediatric wards, as shown by the present data.
A lower risk for management in medical wards was found for the Northeast region, which has a high proportion of hospitals with pediatric oncology wards. These data could imply a “geographic” protection factor in terms of management on medical wards.
While the literature remains controversial, most international findings demonstrate the importance of a pediatric oncologist in the prognosis and treatment of tumors for AYA patients. Pediatric oncology wards in Brazil care for children and adolescents until 18 years of age, as dictated by the Brazilian Children and Adolescent Statute, which defines adolescence as the age bracket of 12–18 years of age. However, currently, in Brazil, there is a lack of data for the effectiveness of specific treatments or protocols for AYA cases.
Clinical programs with appropriately trained healthcare professionals, as well as improved communication and collaboration between adult and pediatric oncologists are vital if the care provision for AYA patients with cancer is to be optimized. Several countries such as the United Kingdom, United States, Australia, and Germany have established collaborative care programs, although the development of a comparable AYA oncology program in Brazil remains a challenge.29,30
Further work is now needed in terms of evaluating treatment outcomes for the AYA patient age group in Brazil. With this in mind, the focus now should be on evaluating treatment response, protocols, and outcomes according to tumor type and site of care.
FundingHTGM and NVB were awarded scholarships from the Nacional Cancer Institute post-graduation program, and BDC receives a scholar grant from the National Council for Scientific and Technological Development (Conselho Nacional de Desenvolvimento Científico e Tecnológico, CNPq, Brasília; #306291/2014-2) and from the Foundation for Support of Research in the State of Rio de Janeiro (Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro, FAPERJ, Rio de Janeiro; #212989-2016).
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank all the BHCR coordinators in Brazil that contributed the datasets that made this work possible.
Please cite this article as: Martins HT, Balmant NV, Silva NP, Santos MO, Reis RS, Camargo B. Who cares for adolescents and young adults with cancer in Brazil? J Pediatr (Rio J). 2018;94:440–5.