To present the different aspects that may be involved in the genesis and maintenance of obesity in children and adolescents.
Data sourceNarrative review of articles published in the PubMed, Scielo, Lilacs, Scopus and Google Scholar databases, using the search terms: overweight, obesity, pre-conception, prenatal, infants, schoolchildren, children, and adolescents. The search was conducted in studies written in Portuguese, English and Spanish, including narrative, integrative or systematic reviews, meta-analyses, cross-sectional, case-control and cohort studies, published between 2003 and 2023.
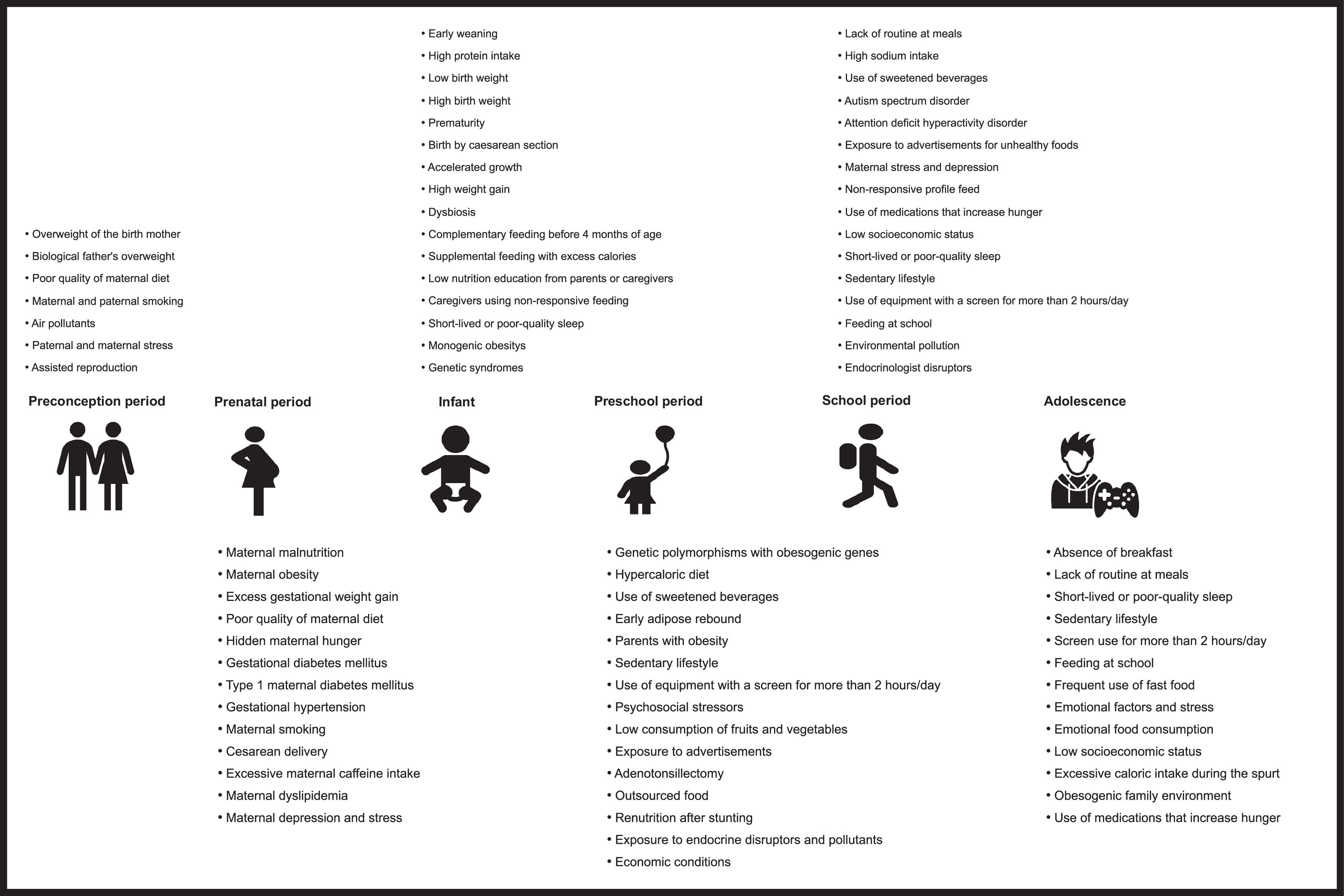
Data synthesisA total of 598 studies were initially screened and 60 of them, which showed the main biopsychosocial aspects related to greater risks of excessive adiposity in the pediatric age, were included in the review. The data were presented taking into account the incidence of risk factors and their consequences in six periods: pre-conception, pre-natal, infant, preschool, school age, and adolescence.
ConclusionsThe causal factors described in the scientific literature that have been shown to be related to obesity in childhood and adolescence are presented.
The global epidemic of obesity in the pediatric population is a direct consequence of the interaction between genetics and lifestyle. However, this apparent simplicity hides a complex network of biopsychosocial mechanisms that act at all stages of life, modulating the ways in which aspects linked to genes and the environment interact. The present review discusses, based on the available evidence, the most important of these mechanisms, aiming at providing the health professional with the best diagnosis that will lead to the individualization and optimization of treatment.
MethodThis is a narrative review of articles published in the PubMed, Scielo, Lilacs, Scopus and Google Scholar databases, using the following search terms: overweight, obesity, pre-conception, prenatal, infants, school-aged, children, and adolescents. The search comprised studies written in Portuguese, English and Spanish, comprising narrative, integrative or systematic reviews, meta-analyses, cross-sectional, case-control and cohort studies, published between 2003 and 2023. Of the 598 initially identified studies, 60 were chosen to constitute the theoretical framework of the review. The selection criteria took into account: the period of publication, with preference being given to the most recent ones; scope, prioritizing those of a population nature; studies published in journals indexed in the most recognized academic databases; narrative, integrative, and systematic reviews; and meta-analyses.
Preconception periodThe environment that mothers and fathers experience in the preconception period can influence the later emergence of adiposity in childhood. Environmental factors, such as nutrition, can induce changes in methylation patterns in the parental germline and reprogram the epigenome of cells, thereby transmitting susceptibility to obesity to future generations through transgenerational epigenetic inheritance. Maternal obesity before the start of the pregnancy is associated with a greater risk of obesity in the offspring, with an estimated three-fold greater risk.1
The preconception dietary pattern must also be considered and the low-quality index of the maternal diet is associated with higher percentages of body fat and BMI in children aged 8–9 years.2
Despite the strong associations attributed to the mother-child binomial, it is essential to highlight the importance of the father. The father's preconception excess weight is also a risk factor for overweight and obesity in childhood.3
Other environmental factors during the preconception period can influence excess childhood adiposity, such as maternal stress, exposure to air pollutants, assisted reproduction, and smoking habits. Smoking may be associated with childhood adiposity for several generations; the habit of smoking by paternal grandparents is positively associated with obesity in their grandchildren, through inheritance transmitted epigenetically through male germ cells.4
Prenatal periodThe period between conception and birth is characterized as a relevant window for the emergence of obesity and the identification of the factors involved can be important for prevention and treatment strategies.
Intrauterine environmentThe “thrifty phenotype” hypothesis proposes that a fetus that receives less than the necessary nutrition adapts through physiological changes that will allow survival in such a context. The metabolism is altered by an epigenetic mechanism, and changes can persist after birth, resulting in adverse consequences for long-term health, and contributing to the origin of chronic diseases, especially obesity. Therefore, the pathway that leads to obesity in childhood and adulthood may begin with intrauterine malnutrition, low birth weight, and small body size during childhood.5
On the other hand, it should be noted that increased gestational BMI can lead to the birth of large-for-gestational-age (LGA) infants, who are at greater risk of obesity in later life. Excess maternal weight gain during pregnancy also increases the risk of LGA babies, with a relationship between high gestational weight gain (GWG) and greater weight and length at birth and during childhood. The association between GWG and childhood adiposity is stronger in children born to women with pre-gestational obesity and when the greatest weight gain occurs early in the pregnancy.6
Maternal habits and dietPoor diet quality during pregnancy increases neonatal adiposity, regardless of pre-gestational maternal BMI and total energy intake, and diets with a pro-inflammatory profile during pregnancy are associated with a greater chance of LGA babies. Maternal dietary restriction of iron, zinc, calcium, and magnesium results in increased body fat in the offspring. The use of caffeine by pregnant women has been shown to increase the risk of low birth weight babies (and, therefore, the risk of future obesity) in a dose-dependent manner. The consumption of sweetened drinks during pregnancy is correlated with obesity at six years of age. Pregnancy maternal smoking and exposure to air pollutants have also been associated with excess weight in childhood. Pollutants act as endocrinological disruptors, with a positive association being observed between maternal exposure and concentrations of adipokines, adiponectin, and leptin in the umbilical cord of newborns.7,8
Maternal illnessesMaternal diabetes mellitus, whether gestational or type 1, can lead to fetal overnutrition as a result of maternal hyperglycemia during pregnancy.9 Dyslipidemia in early pregnancy is associated with adiposity in the offspring.10 Significant associations have also been found between gestational hypertension and excess weight in childhood and adolescence due to placental dysfunction, with compromised nutrient supply to the fetus, oxidative stress, inflammation, and impaired metabolism of glucocorticoids. These factors can lead to changes in adipose tissue morphology, metabolism and fetal hormone levels.11
Among psychiatric conditions, maternal depression and stress during pregnancy have been identified as risk factors for future obesity.12
InfantThe first two years of life are a period of high relevance for detecting and addressing causal factors linked to the risk of excess weight gain. Among the several causes associated with obesity in this age group, some factors described below can be highlighted.
Genetic and hereditary factorsThe genetic influence on obesity is complex and multifactorial and gene expression can be modified by environmental, behavioral and epigenetic factors. Genetic polymorphisms have been associated with a greater risk of obesity in infants and more than 900 genes have been linked to obesity. Genes play a crucial role in regulating aspects such as basal metabolic rate, leptin sensitivity, stress response, body fat distribution and even food preferences. Among monozygotic twins, children born to obese parents have a greater genetic predisposition to develop obesity, with a concordance of 40 to 75 %.13
There are variants related to non-syndromic monogenic forms that are associated with genes involved in appetite control (food intake), fat metabolism, and hormonal regulation, among other metabolic processes. The mutations involve the encoding of leptin and its receptor, proopiomelanocortin (POMC), melanocortin 4 receptor (MC4R), proprotein convertase subtilisin/kexin Type 1 (PCSK1), homolog of the single-minded (SIM) gene of Drosophila, brain-derived neurotrophic factor (BDNF) related to energy balance, neurotrophic receptor tyrosine kinase 2 (NTRK2) and some rare MC3R mutations.14
Birth and growth conditions in the first two years of lifeThere is an association between cesarean section birth and childhood obesity. Kuhle et al.15 showed a risk ratio of 1.34 for obesity between 2 and 15 years compared to vaginal birth.
Preterm children are more likely to have future obesity compared to full-term babies and this trend does not depend on weight adequacy, being similar for newborns who are small or appropriate for gestational age.16
Infants with a high BMI or those who experience rapid and excessive weight gain are more likely to develop obesity in later age groups. Additionally, children with an early onset of adiposity rebound gain fat more quickly when compared to those with a later onset of this physiological phenomenon.17
Interruption of breastfeedingShorter breastfeeding time has been associated with a higher risk of obesity. The risk is inversely proportional to the duration and for each month of breastfeeding there is a 4 % reduction in the risk of developing excess weight in later life. Lower protein concentration when compared to traditional infant formulas, more adequate self-regulation of appetite, and “later” introduction of solid foods into the infant's diet explain the protective effect.18 Additionally, breastfeeding causes epigenetic changes, promoting the methylation of certain genes that reduce the risk of developing obesity.19 The duration of maternal breastfeeding is positively associated with the consumption of fruits and vegetables at the preschool age, which is understood as a protective factor.20 Obese mothers tend to breastfeed their children for a shorter time when compared to non-obese mothers; more frequent complications in the peripartum period and changes in hormonal balance secondary to obesity help explain these findings.21
The microbiota of breastfed infants, consisting of Bifidobacterium, Streptococcus and Lactobacillus, is related to a healthy weight; changes through the introduction of milk other than human milk, or excessive use of antibiotics, may be implicated in changes in the profiles of Firmicutes and Bacteroidetes phyla/species, related to the development of dysbiosis, associated with obesity in both adults and children.22
Excess of protein consumptionFor non-breastfed children, the use of cow's milk or infant formulas with a high protein content promotes pathological acceleration of growth and a greater risk of obesity. This effect is mediated by higher concentrations of insulinogenic amino acids, derived from the greater protein supply, with an increase in some hormonal mediators, such as insulin and IGF-1, and a reduction in the beta-oxidation of fatty acids through the activation of the cell growth pathway mediated by mTOR. (Mammalian Target of Rapamycin). Methionine has also been implicated in the genesis of obesity, secondary to high protein intake early in life through mechanisms involving DNA methylation and decreased fat oxidation.23
Introduction of inadequate complementary feedingStarting complementary feeding before four months of age may be linked to excess weight in childhood. The dietary pattern is also related and the consumption of fried/fatty foods, fast foods, sweets, and drinks with added sugar, as well as a low fruit and vegetable intake, have been linked to being overweight.24
Low nutritional education of parents or caregiversA structured family environment has implications for the acquisition of good eating habits. Parents are the main guides of their children's eating habits. Lack of nutritional knowledge, passed from parent to child, determines a poor diet; verbal threats made at the time of feeding culminate in attitudes of repulsion towards that food on the part of the child; furthermore, unfavorable socioeconomic conditions, such as less access to healthy foods, can negatively influence eating habits and increase the risk of future obesity.25
Microbiota alterationsExposure to antibiotics during early childhood can increase the risk of childhood obesity and the main hypothesis for this phenomenon would be changes in the microbiota. Overweight mothers may be carriers of a microbiota that increases the risk of obesity in their offspring and other factors may be associated, such as the type of delivery and maternal diet pattern.26 To date, there is not enough evidence to propose any intervention (probiotics, for instance) to address dysbiosis associated to obesity, so prevention remains the priority.27
Preschool periodAlthough effects related to previous periods persist, since pre-conception, the environment and lifestyle start to exhibit greater relevance in the genesis of obesity in the preschool period.
Maternal and paternal factorsIncreases in the mother's BMI in the postnatal period are related to a concomitant increase in this index in preschool children. Children of obese mothers are more likely to also be obese, which could reflect an “obesogenic” environment secondary to greater caloric intake. Additionally, some behaviors regarding their children's nutrition are more observed in obese mothers, such as the use of food as a reward and as a response to negative feelings, lower perception of the child's satiety, and the adoption of restrictive dietary patterns. Maternal depression has also been linked to obesity in the preschool period. A less rigid control of time spent watching television, less encouragement for physical activity, and a low level of involvement with the child's health, in general, are possible explanations for this finding.28
Studies have shown that paternal BMI can also influence the risk of developing excess weight in children as much as the maternal BMI.29
Factors linked to growthChildren with stunting have reduced fat oxidation capacity and this finding could explain the excessive weight gain observed when the normal diet is reestablished.30
Hypothalamic obesityCranioencephalic injuries secondary to trauma and tumors increase the risk of being overweight after the event. Long periods of hospitalization, changes in behavior, and the development of hyperphagia secondary to lesions in the hypothalamus areas responsible for controlling satiety explain the phenomenon.31
Environmental factorsSome chemical substances present in daily life, such as phthalates and bisphenol A, present in plastics, are known to be obesogenic; these substances may eventually come into contact with humans through water, air, or skin. Some studies have shown that these molecules are capable of inducing the differentiation and increase of adipocytes in vitro, with one of the possible mechanisms of their action being the induction of epigenetic changes. Exposure to cigarette smoke and air pollution in the first years of life may also be related to obesity in preschool children.32
Psychosocial factorsSome behavioral factors have been associated with the development of excess weight. Impatience, extroversion, limited self-regulation, great suffering in the face of difficulties and “difficult” temperament (children who are easily distressed, inhibited, cry frequently, and have a low capacity to calm themselves) are among these behaviors. The parents of these children would try to control many of these behaviors by offering high-energy foods to their children. Time spent in front of the television, especially more than two hours a day, has been associated with excess weight among preschoolers. Exposure to advertising of unhealthy foods and/or foods with high caloric value and low nutritional value, in addition to its association with a sedentary lifestyle, would be among the explanations that would lead to prolonged contact with the television to constitute a risk factor. Restrictive eating patterns imposed by parents can also paradoxically exert an influence, as children tend to consume more “forbidden” foods than “allowed” ones when they are not under supervision.33
Children living in families from lower socioeconomic classes are more likely to become obese. High stress, low self-esteem, family dysfunction, food insecurity, and less access to healthier living and eating patterns would be “obesogenic” factors that would help explain this phenomenon in situations of economic and social vulnerability. Moreover, children who live in areas with little access to free space, which predisposes them to a sedentary lifestyle, and many places that sell “fast food” are at greater risk of being overweight.34
Psychosocial stressors, such as the absence of a social support network, parental unemployment, immigration and adverse childhood experiences (divorce, abuse of any kind, arrest of one of the housemates, living with a person with drug addiction problems and neglect) have also been associated to childhood obesity at preschool age. One of the hypotheses for this observation would be that children submitted to psychosocial stressors could “compensate” for their frustrations through food, in addition to having less incentive to perform physical activity. Additionally, many of these children can develop depression and anxiety, situations that are often associated with eating habit disorders.35
Children living in families that receive assistance from food distribution programs, but who are not in a situation of food insecurity, are at greater risk of developing excess weight during the preschool period,36 which is also observed when care is outsourced, especially when it is carried out informally (for example, at the grandparents' house).37
School periodSchool-age children also suffer the consequences of the causes of obesity from previous ages, but the most notable influences now come from the environment in which they live, with an impact on their nutritional condition.
Eating patternsEating patterns associated with obesity have been identified: skipping breakfast, excess intake of fat and refined carbohydrates, and low intake of dairy products, fruits, and vegetables. De Amicis et al.,38 in a systematic review, highlighted four longitudinal studies in children (4 to 10 years old) with follow-up for more than four years in which they found a positive association between the consumption of unhealthy foods and adiposity. Atanasova et al.39 highlight the importance of the food environment when evaluating the effect of incentives on children (6 to 12 years old), reporting that toy prizes significantly increased purchases of less healthy and low-calorie meals in fast-food restaurants.
Grimes et al.40 report a positive association between sodium intake and overweight/obesity, specifically among Australian schoolchildren aged 4 to 12 years, citing that each additional 1 g/day of salt was associated with a difference in BMI z-score of 0.10, adjusted for sex, age and socioeconomic status. They also observed an association between sodium intake and the consumption of sugary drinks in children aged 2 to 18 years.
Kaisari et al.41 demonstrated that a higher eating frequency was associated with lower body weight in children and adolescents.
Sugary drinksAbbasalizad Farhangi et al.42 show in 33 studies with 121,282 individuals, that excessive intake of sugary drinks was associated with an increase of 0.75 kg/m2 in BMI and abdominal circumference in children and adolescents. Jakobsen et al.43. concluded that greater intake of sugary drinks increased the chances of overweight/obesity by 1.20.
Social aspectsAspects of family function, such as poor communication, low behavioral control, high levels of family conflict and low family hierarchy values are associated with an increased risk of obesity. The organization of the family environment (routines for meal times, sleep, limits on time spent in front of screens, family crowding) was analyzed in schoolchildren by Bates et al.,31 who found a lower frequency of family meal practices associated with higher BMI, showing the protective impact of family meal routines. They observed a higher BMI among children with a low frequency of eating breakfast at home (≤ 2 times/week), and more time spent watching TV and screens; moreover, they found that fewer people in the child's living space (5–12 years) and fewer siblings were risk factors for childhood obesity. An increase in the prevalence of overweight and obesity is also observed after exposure to food advertisements.44
Children from families with higher socioeconomic levels and those who attend private schools tend to be more overweight and obese. Higher parental level of schooling, more minutes of recess and physical education, urban housing, greater parental involvement in school, and healthy school food environments are significantly associated with lower rates of obesity in children aged 7 to 12 years. Schoolchildren cared for by grandparents may have a 30 % higher risk of overweight/obesity. Cultural values, beliefs, and food-related behaviors, especially, those related to eating habits, kinship, and social factors strongly influence the obesity-related lifestyles of children aged 5 to 11 years.45
SleepSleep hours are directly related to obesity during school years and there is a positive association between inadequate quantity and quality of sleep and a greater chance of obesity. Insulin resistance, a sedentary lifestyle and unhealthy eating patterns, typical of children with inadequate sleep, lead to excess weight gain in children and adolescents.46
Sedentary lifestyleEating while watching TV is positively associated with excess weight in school children. There is a significant and positive association between greater internet use and obesity, with a dose-response effect, with each additional hour/day of internet use resulting in an 8 % increase in the chances of obesity. The Covid-19 pandemic clearly showed the relevance of a sedentary lifestyle for the onset and maintenance of obesity among schoolchildren.47
Other factorsAutism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) may increase the risk of childhood obesity. Li et al.48 found that the combined estimates of the prevalence of obesity, overweight and underweight were 21.8 %, 19.8 %, and 6.4 % in individuals with ASD and 14.7 %, 20.9 %, and 4.0 % in individuals with ADHD. In subgroup analyses, an increasing trend in the prevalence of unhealthy weight was observed among children aged 6 to 12 years to adults with ADHD. Hendrix et al.49 observed that children with developmental coordination disorder seem to be at greater risk of being overweight and obese. This risk may be higher for boys and seems to increase with age and the severity of motor impairment between 4 and 14 years of age.
Da Silva Fernandes et al.,50 in a systematic review, concluded that human adenovirus, subtype 36 (Adv36), is an adipogenic agent and causes metabolic changes. Strong evidence suggests a positive association between viral infection and obesity.
Jeyakumar et al.,51 in a systematic review, concluded that body mass index increased postoperatively in 50 to 75% of children undergoing adenotonsillectomy (T&A).
AdolescenceDue to the changes that occur at this stage of life, adolescents are considered to be at high nutritional risk, not only due to the large and specific needs that must be met but also due to their emotional and social characteristics.52
Increased food intakeDuring the pubertal growth period, adolescents need to increase their energy intake, and caloric intake that exceeds energy use is the main mechanism that can cause an increase in body fat. Additionally, there are other dietary factors that contribute to obesity, such as changes in eating patterns, consumption of foods high in fat and energy, decreased intake of fruits and vegetables, and increased consumption of sugary drinks. This pattern is directly related to the conditions of modern life, which highlights the need for time aimed at various daily activities to the detriment of time reserved for meals in the family environment, preference for having meals with peers, increased availability of prepared foods, and excessive exposure to fast food chain marketing.44
Emotional factorsAlternating periods of anxiety and depression, associated with stress, are part of adolescents' daily lives as a form of emotional maturity. Studies have demonstrated an association between experiencing stressful situations and a higher risk of obesity and metabolic syndrome. Stress and depression have been related to dysregulation of the hypothalamic-pituitary-adrenal axis, contributing to the emergence of metabolic changes and weight gain. Stress stimulates the hypothalamic-pituitary-adrenal axis, with consequent secretion of cortisol which, in turn, promotes eating by increasing intake, reduces the brain's sensitivity to leptin, and promotes fat deposition. Eating patterns associated with the intake of highly palatable and tasty foods, which activate dopaminergic pathways, are observed after a stressful event, thanks to the increase in cortisol levels. Moreover, stress reduces executive functions while increasing emotional reactivity, leading to dependence on habits that may include, for instance, obesogenic eating.53
Another condition that can be observed among adolescents is the so-called “emotional eating”, defined as the use of food as a coping mechanism for stressful situations or negative feelings. Although emotional eating has been primarily related to a type of response to negative feelings, it has been found that people can also act this way when faced with positive feelings, such as joy or excitement. Regardless of the type of feeling to which adolescents respond, emotional eating has been associated with other behaviors, such as binge eating and loss of control over eating, large consumption of high-calorie foods with low nutritional density, with a consequent increase in adiposity and body mass index.54
Family factorsAdolescents' eating habits begin to be shaped during childhood, under the influence of parents and family. The preference for and consumption of healthy foods depends on accessibility, recurring exposure, and the relevance of these foods in the context of family meals. The eating styles of parents and other family members play important roles, since imposed food offerings, when parents make decisions and restrict unhealthy foods, can have the opposite effect, due to the contesting and challenging characteristics that predominate during adolescence, increasing their desire for such foods. Parental permissiveness, on the other hand, regarding the purchase of food, eating out, and watching TV can lead to obesogenic eating patterns. Conflictive family environments and unstable relationships favor access to unhealthy foods and predispose people to eat without feeling hungry, increasing the consumption of sweets/candy, snacks, unhealthy foods and sugary drinks.55
Social factorsThe availability of high-calorie foods in cafeterias and around schools can also contribute to an increase in adolescents' daily caloric intake. Studies carried out in several countries show greater dependence on takeaway food or food purchased in convenience stores or fast food chains.56
Excess weight in adolescents is more prevalent among individuals with worse socioeconomic conditions. Low socioeconomic status can be considered a social stress factor for adolescents, who are subject to food insecurity, which can significantly influence their diet and eating habits. Even in developed countries, a higher prevalence of obesity is observed among adolescents who live in underprivileged socioeconomic areas.57
Sedentary lifestyleThe new profile of sedentary leisure is growing rapidly, associating the decrease in physical activities with the increase in the consumption of snacks and “automatic eating”. The reasons are varied and include greater involvement in the digital world, less time dedicated to outdoor recreational activities, concerns about the safety of public places and greater pressure from academic activities and good school performance.44
The decrease in opportunities to be physically active is also associated with the development of motorized transportation, with fewer teenagers walking or using bicycles to get to school. Concerns about safety and the potential risks offered by the urban environment also end up leaving adolescents with fewer and fewer opportunities to spend energy.58
SleepThe relationships between sleep duration and body weight are complex and involve several mechanisms, since sleep, like appetite, is governed by a diurnal circadian rhythm. From a biological point of view, the short sleep duration is associated with changes in the hormonal metabolism that regulates appetite, with a reduction in leptin and an increase in ghrelin levels, leading to greater food intake.59
Diseases and medicationsAlthough it is uncommon for them to start in this age group, some diseases, such as hypothyroidism and Cushing's syndrome, can favor the onset of obesity. The side effects of some medications such as thiazolidinediones, sulfonylurea, tricyclic antidepressants, lithium, antipsychotics, anticonvulsants, antihistamines, beta-blockers, selective serotonin reuptake inhibitors and corticosteroids, prescribed in specific conditions, will contribute to the increase in body weight through various mechanisms, such as: stimulating appetite, interfering with metabolism and glucose storage, decreased energy expenditure and water retention, among others.60
ConclusionsThe present review addressed the main mechanisms evidenced by science capable of influencing the development of obesity in childhood and adolescence. Figure 1 summarizes the most relevant findings.
Institution or official service to which the study is linked for registration purposes in the Index Medicus/MEDLINE database: Universidade Federal de São Carlos – UFSCAR.