To examine the effect of initiating very early feeding on time-to-reach full feeding in stable, small for gestational age (SGA) preterm infants.
MethodPreterm infants with gestational age below 37 weeks and birth weight below the 10th percentile were randomly allocated to a very early (within 24hours of birth) feeding regimen or delayed (after 24hours of birth) feeding. All infants had in utero evidence of absent or reverse diastolic flow. Infants unable to start early feeding were excluded. Time-to-reach full feeding, feeding progression, and related morbidity were compared. Electrogastrography (EGG) was used to measure pre- and postprandial gastric motility on the second and seventh day after feeding initiation.
ResultsSixty infants were included in the study, 30 in each group. Infants included in the very early feeding regimen achieved full enteral feeding sooner than controls (98±80-157 vs. 172±123-261hours of age, respectively; p= 0.004) and were discharged home earlier (p=0.04). No necrotizing enterocolitis (NEC) was documented in both study groups. Gastric motility was improved at day seven after feeding initiation in both study groups, with no difference between groups.
ConclusionsStable SGA preterm infants on a very early feeding regimen achieved full enteral feeding and were discharged home significantly earlier than those on a delayed regimen, with no excess morbidity.
Examinar o efeito da nutrição precoce sobre o tempo para atingir a nutrição completa em neonatos prematuros (PIG) estáveis pequenos para a idade gestacional.
MétodoOs neonatos prematuros com idade gestacional inferior a 37 semanas e peso ao nascer inferior a 10% foram alocados aleatoriamente para um regime de nutrição precoce (nas primeiras 24 horas de vida) ou tardia (após as primeiras 24 horas de vida). Todos os neonatos apresentaram uma evidência intrauterina de fluxo diastólico reverso ou ausente. Os neonatos incapazes de iniciar uma nutrição precoce foram excluídos. O tempo para a alimentação completa, a progressão da nutrição e morbidez correspondente foram comparados. A eletrogastrografia (EGG) foi utilizada para mensurar a motilidade gástrica pré e pós-prandial no segundo e no sétimo dias após o início da nutrição.
ResultadosForam incluídos 60 neonatos no estudo, sendo 30 em cada grupo. Os neonatos incluídos no regime de nutrição precoce atingiram a nutrição enteral completa antes dos neonatos do grupo de controle (98±80-157 em comparação a 172±1 23-261 horas de idade, respectivamente; p=0,004) e recebiam alta hospitalar antes (p=0,04). Nenhuma enterocolite necrosante (ECN) foi comprovada em ambos os grupos de estudo. A motilidade gástrica melhorou no sétimo dia após o início da nutrição em ambos os grupos de estudo, sem diferença entre eles.
ConclusõesOs neonatos prematuros PIG estáveis em regime de nutrição precoce atingiram alimentação enteral completa e receberam alta hospitalar significativamente antes que aqueles em regime de nutrição tardio, sem morbidez excedente.
Early enteral feeding in very low birth weight (VLBW) infants is associated with reduced incidence of sepsis, improved milk tolerance, postnatal growth, and shorter hospital stay.1,2 However, based on available data, a word of caution about early initiation and advancement of enteral feeding in VLBW infants was issued, especially for small for gestational age (SGA) infants, arguing that it may predispose them to feeding intolerance and greater risk of necrotizing enterocolitis (NEC).3 The incidence of NEC was found to be increased in SGA infants4,5 who exhibited abnormal fetal umbilical artery Doppler velocities.6 These abnormalities of the splanchnic blood flow during fetal life persist postnatally and only partial recovery is achieved in the first week after birth.7 For these reasons, the 1999 survey of feeding practices for SGA infants suggested the possibility of delaying feeding from one to seven days after birth (unpublished data: Dorling JS, McClure RJ. Survey of feeding practices for infants with AREDFV in the Eastern Region. Eastern Region Neonatal Conference, October, 1999).
Several authors have investigated early and delayed feeding of SGA infants, born after absent or reverse diastolic flow velocity in the umbilical artery based on intra-uterine Doppler. They found no differences in the incidence of NEC or feeding intolerance.8,9 No advantage in withholding feeding in SGA preterm infants was shown in the 2011 updated Cochrane review (n=600).10 The effect of early (day two) versus delayed (day six) feeding on time-to-full enteral feeding and NEC incidence was examined in another recent multicenter trial of SGA preterm infants with abnormal Doppler fetal umbilical flow. The data showed that infants who were fed from postnatal day two achieved full feeding faster than those who were fed on day six (median age 18 vs. 21 days, respectively). This effect was significant only in stable preterm infants with a gestational age of 29 weeks or more. No difference was observed in the incidence of NEC.11 The effect of earlier full feeding was also associated with shorter need for parenteral nutrition and lower incidence of cholestatic jaundice; no advantage of weight gain or earlier discharge was reported.
The present study aimed to evaluate very early feeding, starting less than 24hours after birth, in stable SGA preterm infants, and to determine whether this regimen of feeding, as opposed to delayed feeding, is associated with earlier full enteral feeding and no excess morbidity. Electrogastrography (EGG) was used to further understand the effect of very early feeding regimen on the gastric motility of stable SGA preterm infants.
MethodsStudy populationA total of 313 preterm infants admitted to the neonatal intensive care unit (NICU) between February 1, 2009 and November 26, 2011 were screened for this randomized, prospective study. Inclusion criteria were clinically and hemodynamically stable conditions, a birth weight less than the 10th percentile of median birth weight standards, as defined by the Israel National Data Registry,12 and gestational age less than 37 weeks, with in utero evidence for absent or reverse diastolic flow. Exclusion criteria were systemic disease, need for mechanical ventilation, major congenital anomalies including known chromosomal abnormality, enteral feeding before study entry, use of anti-reflux medication or special diet before or during the study period, Apgar score 0 to 3 for>5minutes, arterial cord blood pH<7.0 or base deficit 12 to 16 mmol/L, need for resuscitation, or significant multi-organ failure. Of 71 infants initially included in this study, 11 were excluded due to parental refusal (n=5), change in feeding regimen to continuous feeding (n=3), and surplus artifacts in the EGG measurements making analysis impossible (n=3).
The study protocol was approved by the institutional ethics committee. An informed consent was obtained from all parents. Clinical Trials registration: NCT00819715.
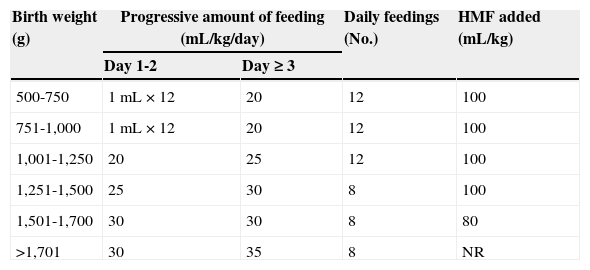
Feeding regimenMothers were encouraged to provide their infants with breast milk; otherwise, infant formula was provided orally or by tube feeding. An informed consent for the trial was obtained from the parents in the first six hours after birth, before starting the first feeding. The parents were given a verbal explanation of the study and a written information sheet. If consent was given, and no contraindications occurred, the infant was then randomized using random number tables, to one of the study groups, either “early” (within 24h of birth) or “late” (24h after birth) commencement of enteral feeding. Caregivers were not blinded to the randomized allocation, but the personnel involved in data collection and analysis were blinded to the study assignment. Both study groups were progressed with the same feeding protocol (Table 1). Feedings were stopped or delayed when clinical signs of abdominal distention/tenderness, visible bowel loops, or emesis were present or gastric residuals were greater than 50% of a three-hour feeding volume. If feed volumes were withheld, the clinician was free to start again from day one with the volume previously tolerated and then increase, or remain for one or more days at a given volume and then increase. Feeding was stopped for three hours after blood transfusion or treatment with non-steroidal anti-inflammatory drugs for patent ductus arteriosus.
Study group scheduled feeding regimen.
| Birth weight (g) | Progressive amount of feeding (mL/kg/day) | Daily feedings (No.) | HMF added (mL/kg) | |
|---|---|---|---|---|
| Day 1-2 | Day ≥ 3 | |||
| 500-750 | 1mL×12 | 20 | 12 | 100 |
| 751-1,000 | 1mL×12 | 20 | 12 | 100 |
| 1,001-1,250 | 20 | 25 | 12 | 100 |
| 1,251-1,500 | 25 | 30 | 8 | 100 |
| 1,501-1,700 | 30 | 30 | 8 | 80 |
| >1,701 | 30 | 35 | 8 | NR |
HMF, human milk fortifier; NR, not required.
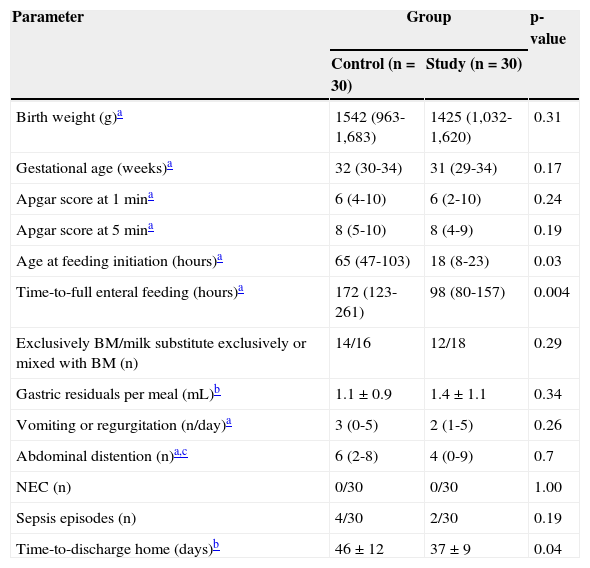
Data were collected at trial entry, during hospital stay, and at discharge home, using computerized medical records and nurses’ charts. Birth weight; gestational age; Apgar scores at one and five minutes; age at feeding initiation (hour); time-to-reach full enteral feedings (150mL/kg); type of diet; number of vomiting or regurgitation events per 24hours; mean gastric residuals per meal (mL); and number of episodes of abdominal distention, leading to feeding cessation during the first seven days of life, were collected (Table 2). Possible morbidity related to early feeding (NEC, sepsis episodes, abdominal distention, vomiting) and time-to-discharge were documented.
Patient characteristics.
| Parameter | Group | p-value | |
|---|---|---|---|
| Control (n=30) | Study (n=30) | ||
| Birth weight (g)a | 1542 (963-1,683) | 1425 (1,032-1,620) | 0.31 |
| Gestational age (weeks)a | 32 (30-34) | 31 (29-34) | 0.17 |
| Apgar score at 1mina | 6 (4-10) | 6 (2-10) | 0.24 |
| Apgar score at 5mina | 8 (5-10) | 8 (4-9) | 0.19 |
| Age at feeding initiation (hours)a | 65 (47-103) | 18 (8-23) | 0.03 |
| Time-to-full enteral feeding (hours)a | 172 (123-261) | 98 (80-157) | 0.004 |
| Exclusively BM/milk substitute exclusively or mixed with BM (n) | 14/16 | 12/18 | 0.29 |
| Gastric residuals per meal (mL)b | 1.1±0.9 | 1.4±1.1 | 0.34 |
| Vomiting or regurgitation (n/day)a | 3 (0-5) | 2 (1-5) | 0.26 |
| Abdominal distention (n)a,c | 6 (2-8) | 4 (0-9) | 0.7 |
| NEC (n) | 0/30 | 0/30 | 1.00 |
| Sepsis episodes (n) | 4/30 | 2/30 | 0.19 |
| Time-to-discharge home (days)b | 46±12 | 37±9 | 0.04 |
NEC, necrotizing enterocolitis; BM, breast milk.
Surface EGG, a noninvasive and well-tolerated tool for examining gastric myoelectric activity, was performed with a sampling frequency of 4Hz and analyzed by a commercial software program (Electrogastrogram, version 6.3, Gastrosoft Inc., Synectics Medical - Stockholm, Sweden). The signal was stored on a portable recording device (Electrogastrogram, Synectics Medical – Stockholm, Sweden).13 At the end of each study, data were uploaded to a computer. Normal gastric slow waves measured from the EGG were defined as the percentage of time during which waves of two to four cycles per minute were observed on the preprandial or postprandial EGG recording. EGG was recorded on day two and seven after feeding initiation, during the 30-minute fasting state (preprandial) and the 30-minute feeding state (postprandial), when an adequate amount of expressed breast milk or milk substitute was consumed. Days two and seven after feeding initiation instead of days two and seven after birth were chosen, because gastric motility maturation is related to feeding in the neonatal period.14
Outcome measuresThe primary outcome measure was the time after birth (in hours), when full enteral feeding (≥ 150mL/kg) was achieved and sustained for 48hours. Secondary outcome measures were the occurrence of NEC or sepsis, abdominal distention or gastric residuals of more than 50% of the previous meal, vomiting, the correlation between pre- and post-prandial EGG normal waves and the time to achieve full enteral feeding, and time (in days) from hospitalization to discharge.
Data analysisThe gestational age at birth was estimated from the calculated delivery date and based on the last menstrual period or first trimester ultrasound and physical examination of the infant at birth. Infants were discharged if they were gaining at least 1% of their body weight per day per week, sucking all feeds, maintaining their temperature in a cot, and the parents were willing and comfortable taking the infant home.
Statistical analysisUnless otherwise indicated, measurements were expressed as mean±SD. Parametric or nonparametric statistical tests were performed for continuous or discrete clinical variables, respectively. Data from different recording periods of the same infant were compared by Friedman's analysis of variance test. In case of significance, the Wilcoxon matched-pairs test was applied. Spearman's rank correlation coefficient was calculated for EGG activity and the time-to-reach full enteral feeding. Unpublished local data of stable SGA preterm infants reaching full feeding at seven to 14 days after birth were used to detect a statistically significant difference in time of 72hours to reach full enteral feeding. At least 56 infants (28 in each group) were required to achieve a power of 0.8 and α of 0.05.
ResultsAnalysis of patient characteristics (Table 2) showed no significant differences in birth weight, gestational age, one- and five-minute Apgar scores, gastric residuals per meal, type of diet, and abdominal distention, reflux, and sepsis episodes between the study and control groups. Maternal prenatal steroid treatment was given to 26 of 30 mothers (87%) in each group. Age at feeding initiation (Table 2) and time-to-full enteral feeding were significantly less in the study group than in the control group (98±80-157 vs. 172±123-261hours, p=0.004). The time-to-discharge was also significantly earlier in the study group (p=0.04). No case of suspected or proven NEC was documented. Two infants of the study group needed blood transfusions, and there was a temporary deviation from the feeding protocol in two others from the study group. None of the infants developed major postnatal adverse effects or needed treatment with non-steroidal anti-inflammatory drugs.
On day two of feeding, the percentage of normal gastric waves in the study and control groups was not different at pre- and post-prandial measurements, and was around 30% of recorded time. On day seven, there was an increase in normal postprandial waves in both groups, but no difference between the study and the control groups (40.1±14.5% vs. 42.6±17.3% respectively). There was no correlation between EGG normal waves and gastric residuals per meal, reflux episodes, and time-to-full enteral feeding in either groups (Spearman's rank correlation, r>0.3 for all).
DiscussionThis clinical trial aimed to demonstrate the potential benefits of a very early progressive feeding regimen as a means of achieving full enteral feeding in stable, SGA preterm infants. The present data, which were consistent with these suggestions, showed that very early scheduled feedings in stable SGA infants was related to a significantly shorter time-to-reach full feeding and earlier discharge from the NICU. The early feeding regimen was safe, with no differences between the very early group and the delayed group regarding episodes of NEC, sepsis, abdominal distention, or vomiting, although the trial was not powered for these variables.
To the best of the authors’ knowledge, this trial is unique in that it compared SGA infants fed at days three to five with those fed much earlier (i.e., within the first 24hours of life) and, in fact, significantly earlier than in other studies.2,9–11 No concomitant improvement in gastric electrical activity was recorded in infants who were fed in the early regimen.
Potential patho-physiological mechanisms can be involved that might influence the primary outcome results. Studies have shown that early enteral feeding prevents gut atrophy, appears to stimulate maturation of the gastrointestinal system, enhances serum gastrin concentrations, and therefore improves eventual feeding tolerance.8
Although enteral feeding is commonly delayed in high-risk infants, there is little evidence to support this approach. A recent Cochrane review, which incorporated data from 600 SGA infants, showed no increase risk of NEC in early vs. delayed feeding.10 The case-control study by Beeby and Jeffrey15 of 82 infants with NEC revealed that contrary to formula feeding, which was shown to be a significant risk factor for NEC, time of first feed (3.1 vs. 2.5 days for study group patients and controls, respectively) was not a risk factor for NEC even in SGA infants of less than 30-weeks gestation. Infants with poor intrauterine growth and abnormal circulation, shown as absence or reversal of end diastolic flow, comprise a subgroup of SGA infants. It was argued that, for a group of infants with restricted growth and prenatal abnormalities of splanchnic blood flow that can persist postnatally with partial recovery during the first week of life, there is physiological justification for delayed and careful introduction of enteral feeding.16 Other authors stated that such a policy would expose babies to prolonged total parenteral nutrition with its associated complications, mainly sepsis and parenteral nutrition-related liver disease.17
On day seven of feeding, normal gastric waves increased to approximately 41% postprandially, which indicates that gastric electric maturation begins soon after birth. These findings are in agreement with those of a longitudinal study by Zhang et al.,14 who reported a progressively increasing percentage of normal gastric waves in the first two months of life, with an increase in normal postprandial wave fraction and no difference in the percentage of normal gastric waves for different gestational ages.
The present study's population comprised only stable SGA infants who had absent or reverse diastolic flow in utero, with no acute co-morbidities. Although this might limit the scope of the findings, it emphasizes the fact that SGA infants with acute postpartum co-morbidities such as respiratory distress, suspected sepsis, and metabolic acidosis should be the subject of further studies to determine whether they are suitable for an early scheduled feeding regimen.
In conclusion, this study demonstrated that introducing enteral feeding within the first 24hours of life to stable SGA infants is associated with earlier full enteral feeding and shorter hospitalization, with no increase in adverse gastrointestinal effects. Potential patho-physiological mechanisms that influence the primary outcome might be involved. However, they were not investigated in this study and deserve further evaluation.
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank Nava Jelin, MA, Meir Medical Center, Kfar Saba, for statistical consultation.
Please cite this article as: Arnon S, Sulam D, Konikoff F, Regev RH, Litmanovitz I, Naftali T. Very early feeding in stable small for gestational age preterm infants: a randomized clinical trial. J Pediatr (Rio J). 2013;89:388–93.