To know the distribution of births of very low birth weight infants by day of the week, and whether this distribution affects the morbidity and mortality in this group of patients.
MethodsThis was a retrospective analysis of data collected prospectively in the Spanish SEN1500 network (2002–2011). Outborn infants, patients with major congenital anomalies, and those who died in the delivery room were excluded. Births were grouped into “weekdays” and “weekends.” A multivariate logistic regression analysis was conducted to evaluate the independent effect of the birth moment on outcomes, and Cox regression for survival.
ResultsOut of a total of 27,205 very low birth weight infants born at and/or admitted to the participating centers, 22,961 (84.4%) met inclusion criteria. A reduction of 24% in the number of births was observed during the “weekends” compared with “weekdays”. In the raw analysis, patients born on weekends exhibited higher morbidity and mortality (mortality rate: 14.2% vs. 16.5%, p<0.001), but differences were no longer significant after adjusting for confounding factors.
ConclusionsThe present results suggest that current care practices reduce the proportion of births during the weekends and tend to cluster some high-risk births during this period, increasing crude morbidity and mortality. However, after adjusting for confounding factors, the differences disappear, suggesting that overall care coverage in these centers is appropriate.
Conhecer a distribuição dos partos de neonatos com muito baixo peso ao nascer durante a semana e se essa distribuição afeta a morbidez e a mortalidade nesse grupo de pacientes.
MétodoEsta é uma análise retrospectiva de dados coletados prospectivamente na rede espanhola SEN1500 (2002-2011). Foram excluídos neonatos nascidos em outro local, pacientes com grandes anomalias congênitas e pacientes falecidos na sala de parto. Os partos foram agrupados em “Dias úteis” e “Final de semana”. Foi realizada uma análise de regressão logística multivariada para avaliar o efeito independente do parto sobre os resultados e uma regressão de Cox para avaliar a sobrevida.
ResultadosDo total de 27.205 neonatos com muito baixo peso ao nascer nascidos e/ou internados nos centros participantes, 22.961 (84,4%) atenderam aos critérios de inclusão. Houve uma redução de 24% no número de partos no “Final de semana” em comparação aos “Dias úteis”. Na análise bruta, os pacientes nascidos em finais de semana apresentaram maior morbidez e mortalidade (Taxa de mortalidade: 14,2% em comparação a 16,5%, p<0,001), porém as diferenças não eram mais significativas após o ajuste aos fatores de confusão.
ConclusõesNossos resultados sugerem que as práticas atuais de atendimento reduzem a proporção de partos em finais de semana e tendem a agrupar alguns partos de alto risco nesse período, aumentando a morbidez e mortalidade brutas. Contudo, após o ajuste aos fatores de risco, as diferenças desaparecem, sugerindo que a cobertura de atendimento geral em nossos centros é adequada.
Over several decades, different studies have pointed out a reduction in the number of births during the weekend, along with an increase in mortality among babies born at this time1–6; this has been termed “the weekend effect.”7 However, these findings have not been consistent in all studies.8 Greater severity or a possible decrease in the quality of care during the weekends have been suggested as possible causative factors.9–11 This effect may also be due to the selective effect of obstetrical intervention during delivery.6,12 Although healthcare policies in many countries have focused on the appropriateness and universality of perinatal care everyday and year-round, there is a lack of contemporary evaluations of perinatal results adjusted by pattern of daily births, obstetrical interventions, and sociodemographic factors, which could allow the characterization of this phenomenon, as well as its magnitude and potential relevance. In addition, most evaluations in literature have referred mainly to mortality, without analyzing morbidity. The objectives of the present study were to determine whether there are significant variations in the number of births according to the day of the week (weekday or weekend) and whether these variations influence the morbidity and neonatal mortality of VLBW infants.
MethodsThe authors retrospectively analyzed data prospectively collected in the national network SEN1500 for ten consecutive years (2002–2011). The characteristics of the database have been described elsewhere,13 and the protocol for data collection and processing previously approved by the institutional review board of each center. Outborn patients and newborns with major congenital anomalies were excluded. Patients who died in the delivery room (DR) were also excluded to avoid selection bias related to elective limitation of therapy in patients born at the limit of viability or in very poor condition. Births that took place from 08:00 am on Monday until 11:59 pm on Friday were considered as weekday births, and those that took place from 00:00 am on Saturday until 07:59 am on Monday were considered weekend births. Gestational antecedents, type of delivery, perinatal interventions, and neonatal morbidity and mortality were studied. Potential confounding factors based on literature review and those available in this hospital's database were selected for multivariate analysis.
Statistical analysisSPSS (IBM SPSS Statistics for Windows, version 20.0, NY, USA) was used for statistical analysis. Continuous variables with normal distribution were expressed as means and standard deviations (SD), and differences between groups were studied with the Student's t-test. Qualitative variables and variables with non-normal distributions were expressed as median and interquartile range (IQR). Inter-group comparisons were carried out using the chi-squared test (χ2), Fisher's exact test, and the Mann-Witney U test, as appropriate. To evaluate the independent effect of the time of birth, a multivariate logistic regression analysis was carried out and the results were expressed as adjusted odds ratios (aOR) with 95% confidence intervals (95% CI). To study the probabilities of survival, the Cox proportional hazards regression model was used, and the results were expressed as adjusted hazards ratios (aHR) with 95% CI. All hypotheses were two-tailed tested, and statistical significance was established at p<0.05 for all comparisons.
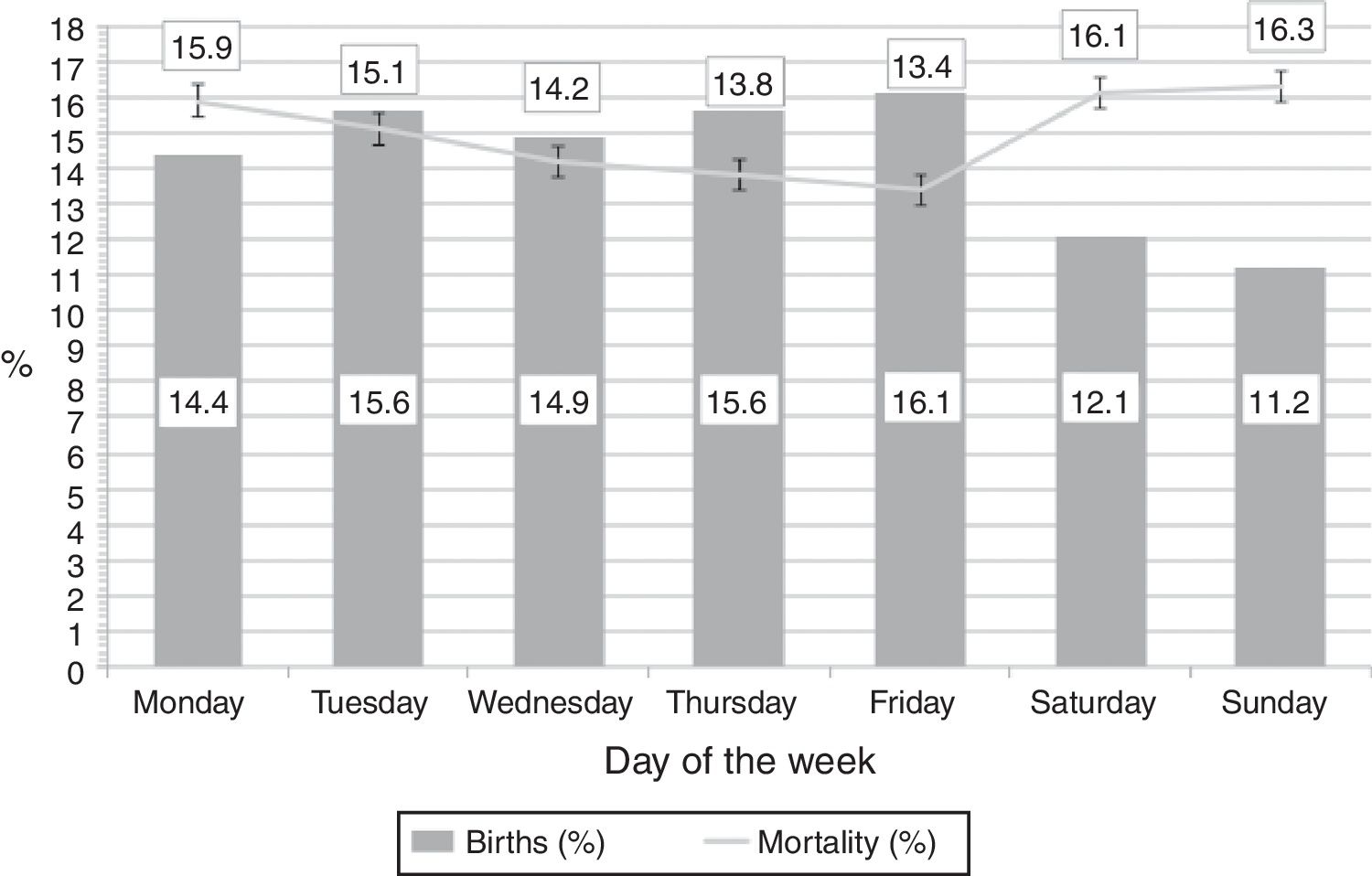
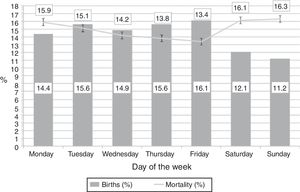
ResultsDuring the study period, a total of 27,205 VLBW infants were admitted to the participating centers. Of these, 25,305 (93%) were inborn. Of these, 1533 (6.1%) with major congenital anomalies and 253 (1%) who died in the DR were excluded. Patients who died in the DR were significantly more immature those who survived (mean [SD] GA was 24.3 [2.3] vs. 29.2 [2.9] weeks; p<0.001). Data regarding limitation of therapy were collected in 142 (56%) of these 253 patients; in 117 cases (82.4%), an elective decision to withhold or withdraw therapy had been taken. Of the patients born on Monday, the hour of birth had not been properly collected in 558 cases, and as a result they could not be classified as being born on the weekend (between 00:00 am and 07:59 am) or on a weekday (from 08:00 am onwards); these cases were also excluded from the study. Finally, 22,961 (84.4%) newborns were included for the analysis. Fig. 1 shows the distribution of births by day of the week. Should the distribution of births across all days of the week be homogeneous, the expected theoretical proportion would be 14.3% of births per day. However, the mean proportion of weekday births was 15.3%, whereas only 11.7% of births occurred on weekend days, indicating a reduction of 24%. These proportions did not vary significantly during the study period.
Distribution of births by day of the week and mortality.
Columns show the proportion of infants born on each day of the week. Mortality indicates the proportion of infants born on that day who eventually died, even though death took place any other day of the week. Error bars indicate the standard error of the mean.
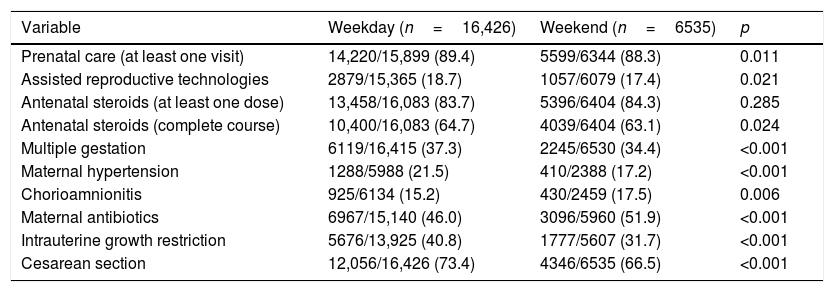
Table 1 presents the obstetric antecedents in both patient groups. Mothers of infants born during weekends had had significantly less prenatal care (defined as at least one medical visit during gestation), assisted reproductive technology (ART), a complete course of antenatal steroids, multiple gestation, maternal hypertension, intrauterine growth restriction, or delivery via C-section. In turn, mothers of infants born on weekends had a higher incidence of chorioamnionitis and maternal antibiotic administration.
Gestational antecedents and type of delivery.
| Variable | Weekday (n=16,426) | Weekend (n=6535) | p |
|---|---|---|---|
| Prenatal care (at least one visit) | 14,220/15,899 (89.4) | 5599/6344 (88.3) | 0.011 |
| Assisted reproductive technologies | 2879/15,365 (18.7) | 1057/6079 (17.4) | 0.021 |
| Antenatal steroids (at least one dose) | 13,458/16,083 (83.7) | 5396/6404 (84.3) | 0.285 |
| Antenatal steroids (complete course) | 10,400/16,083 (64.7) | 4039/6404 (63.1) | 0.024 |
| Multiple gestation | 6119/16,415 (37.3) | 2245/6530 (34.4) | <0.001 |
| Maternal hypertension | 1288/5988 (21.5) | 410/2388 (17.2) | <0.001 |
| Chorioamnionitis | 925/6134 (15.2) | 430/2459 (17.5) | 0.006 |
| Maternal antibiotics | 6967/15,140 (46.0) | 3096/5960 (51.9) | <0.001 |
| Intrauterine growth restriction | 5676/13,925 (40.8) | 1777/5607 (31.7) | <0.001 |
| Cesarean section | 12,056/16,426 (73.4) | 4346/6535 (66.5) | <0.001 |
All values are n/N (%), where N is the total number of patients with valid collected result for the indicated variable. Some variables, such as maternal hypertension and chorioamnionitis started to be collected in 2006, which is the reason for a smaller N in comparison to the other variables.
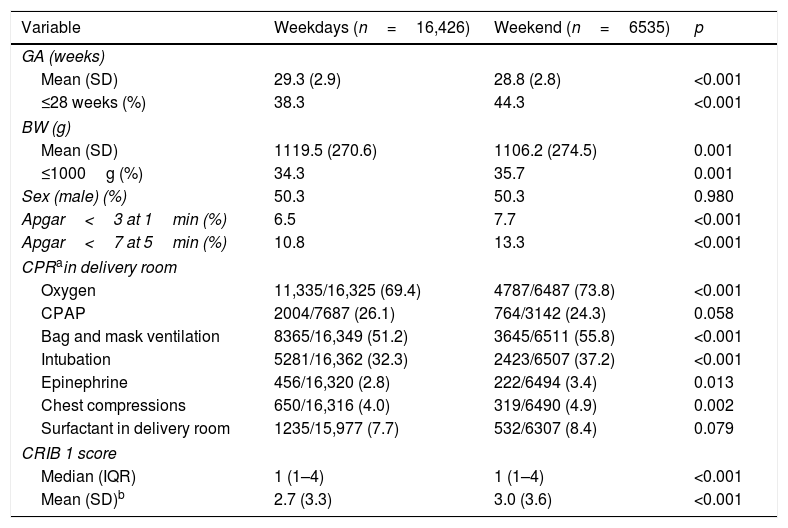
Table 2 shows the somatometric characteristics of patients, their condition at birth, and some relevant aspects of the initial management. Infants born during weekends were more immature, had lower birth weights, and lower Apgar scores at 1 and 5min after birth. Although continuous positive airway pressure (CPAP) use in DR was similar in both groups, patients born during weekends were intubated, received oxygen, epinephrine, or cardiac compressions more frequently than those born on weekdays. Physiological instability in the first 12h after admission, assessed according to the Clinical Risk Index for Babies score,14 was higher in the weekend group.
Sociodemographic characteristics of patients, condition at birth, and interventions.
| Variable | Weekdays (n=16,426) | Weekend (n=6535) | p |
|---|---|---|---|
| GA (weeks) | |||
| Mean (SD) | 29.3 (2.9) | 28.8 (2.8) | <0.001 |
| ≤28 weeks (%) | 38.3 | 44.3 | <0.001 |
| BW (g) | |||
| Mean (SD) | 1119.5 (270.6) | 1106.2 (274.5) | 0.001 |
| ≤1000g (%) | 34.3 | 35.7 | 0.001 |
| Sex (male) (%) | 50.3 | 50.3 | 0.980 |
| Apgar<3 at 1min (%) | 6.5 | 7.7 | <0.001 |
| Apgar<7 at 5min (%) | 10.8 | 13.3 | <0.001 |
| CPRain delivery room | |||
| Oxygen | 11,335/16,325 (69.4) | 4787/6487 (73.8) | <0.001 |
| CPAP | 2004/7687 (26.1) | 764/3142 (24.3) | 0.058 |
| Bag and mask ventilation | 8365/16,349 (51.2) | 3645/6511 (55.8) | <0.001 |
| Intubation | 5281/16,362 (32.3) | 2423/6507 (37.2) | <0.001 |
| Epinephrine | 456/16,320 (2.8) | 222/6494 (3.4) | 0.013 |
| Chest compressions | 650/16,316 (4.0) | 319/6490 (4.9) | 0.002 |
| Surfactant in delivery room | 1235/15,977 (7.7) | 532/6307 (8.4) | 0.079 |
| CRIB 1 score | |||
| Median (IQR) | 1 (1–4) | 1 (1–4) | <0.001 |
| Mean (SD)b | 2.7 (3.3) | 3.0 (3.6) | <0.001 |
GA, gestational age; BW, birth weight; CPR, cardiopulmonary resuscitation; CPAP, continuous positive airway pressure; CRIB, clinical risk index for babies; IQR, interquartile range; SD, standard deviation.
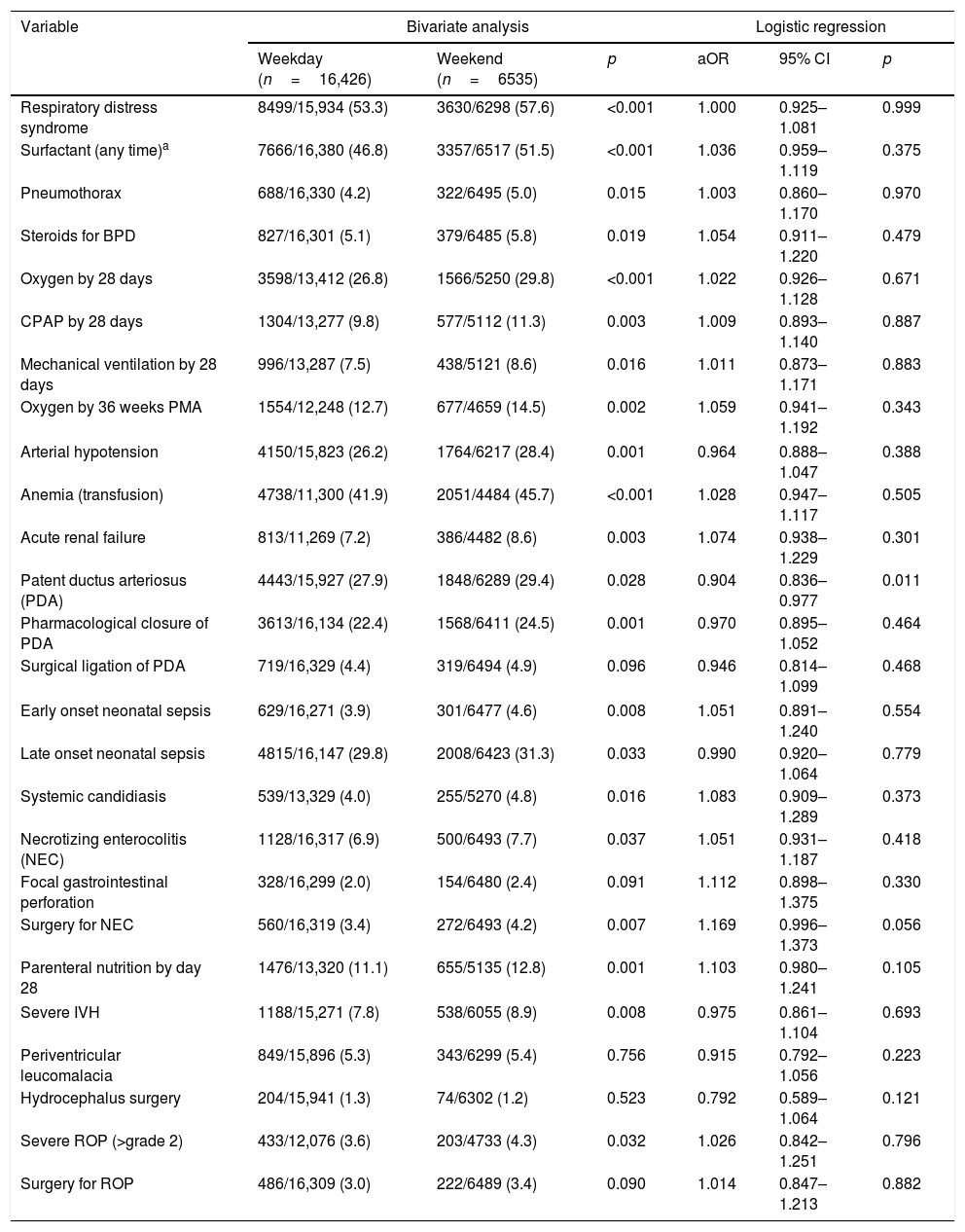
Table 3 presents the most relevant findings of morbidity and mortality in the bivariate and logistic regression analysis. Patients born on weekends had a higher incidence of respiratory disease, hemodynamic instability, anemia requiring transfusion, early and late onset neonatal sepsis, necrotizing enterocolitis (NEC) stage 2 or higher,15 germinal matrix intraventricular hemorrhage (IVH) grades 3 or 4,16 and retinopathy of prematurity grade 2 or higher.17 However, these differences disappeared in the multivariate analysis after correcting for GA, BW, sex, antenatal steroids, multiple gestation, intrauterine growth restriction, and type of delivery. Only the incidence of patent ductus arteriosus (PDA) was significantly higher among patients born during weekends after correction for confounding factors. However, this fact was not associated with a greater need for pharmacological or surgical closure. Finally, mortality was higher among patients born during weekends (14.2% vs. 16.5%; p<0.001), but the probability of survival after adjusting for confounders by the Cox regression analysis was similar (aHR: 1.002 [95% CI: 0.967–1.038]; p=0.915). The distribution of deaths according to the day was similar during weekdays (Mondays, 14.8%; Tuesdays, 15.5%; Wednesdays, 14.6%; Thursdays, 14.7%; and Fridays, 15.5%) while it was significantly lower on the weekend (Saturdays, 13% and Sundays, 12%; p<0.001). Among the 3280 infants who died, data regarding limitation of therapy were collected in 1963 cases (59.8%). A decision to withhold or withdraw therapy was present in 644 cases (32.8%), and the decision to withhold/withdraw therapy was more frequently taken during weekdays (34.4%) than during weekends (28.1%; p=0.035). The age at death was similar in both groups (median [IQR]: 6 (2–18) vs. 7 (2–18) days; p=0.288).
Morbidity and interventions according to day of birth. Bivariate analysis (chi-squared) and multivariate logistic regression for morbidity and interventions (aOR) for patients born on weekends compared to weekdays.
| Variable | Bivariate analysis | Logistic regression | ||||
|---|---|---|---|---|---|---|
| Weekday (n=16,426) | Weekend (n=6535) | p | aOR | 95% CI | p | |
| Respiratory distress syndrome | 8499/15,934 (53.3) | 3630/6298 (57.6) | <0.001 | 1.000 | 0.925–1.081 | 0.999 |
| Surfactant (any time)a | 7666/16,380 (46.8) | 3357/6517 (51.5) | <0.001 | 1.036 | 0.959–1.119 | 0.375 |
| Pneumothorax | 688/16,330 (4.2) | 322/6495 (5.0) | 0.015 | 1.003 | 0.860–1.170 | 0.970 |
| Steroids for BPD | 827/16,301 (5.1) | 379/6485 (5.8) | 0.019 | 1.054 | 0.911–1.220 | 0.479 |
| Oxygen by 28 days | 3598/13,412 (26.8) | 1566/5250 (29.8) | <0.001 | 1.022 | 0.926–1.128 | 0.671 |
| CPAP by 28 days | 1304/13,277 (9.8) | 577/5112 (11.3) | 0.003 | 1.009 | 0.893–1.140 | 0.887 |
| Mechanical ventilation by 28 days | 996/13,287 (7.5) | 438/5121 (8.6) | 0.016 | 1.011 | 0.873–1.171 | 0.883 |
| Oxygen by 36 weeks PMA | 1554/12,248 (12.7) | 677/4659 (14.5) | 0.002 | 1.059 | 0.941–1.192 | 0.343 |
| Arterial hypotension | 4150/15,823 (26.2) | 1764/6217 (28.4) | 0.001 | 0.964 | 0.888–1.047 | 0.388 |
| Anemia (transfusion) | 4738/11,300 (41.9) | 2051/4484 (45.7) | <0.001 | 1.028 | 0.947–1.117 | 0.505 |
| Acute renal failure | 813/11,269 (7.2) | 386/4482 (8.6) | 0.003 | 1.074 | 0.938–1.229 | 0.301 |
| Patent ductus arteriosus (PDA) | 4443/15,927 (27.9) | 1848/6289 (29.4) | 0.028 | 0.904 | 0.836–0.977 | 0.011 |
| Pharmacological closure of PDA | 3613/16,134 (22.4) | 1568/6411 (24.5) | 0.001 | 0.970 | 0.895–1.052 | 0.464 |
| Surgical ligation of PDA | 719/16,329 (4.4) | 319/6494 (4.9) | 0.096 | 0.946 | 0.814–1.099 | 0.468 |
| Early onset neonatal sepsis | 629/16,271 (3.9) | 301/6477 (4.6) | 0.008 | 1.051 | 0.891–1.240 | 0.554 |
| Late onset neonatal sepsis | 4815/16,147 (29.8) | 2008/6423 (31.3) | 0.033 | 0.990 | 0.920–1.064 | 0.779 |
| Systemic candidiasis | 539/13,329 (4.0) | 255/5270 (4.8) | 0.016 | 1.083 | 0.909–1.289 | 0.373 |
| Necrotizing enterocolitis (NEC) | 1128/16,317 (6.9) | 500/6493 (7.7) | 0.037 | 1.051 | 0.931–1.187 | 0.418 |
| Focal gastrointestinal perforation | 328/16,299 (2.0) | 154/6480 (2.4) | 0.091 | 1.112 | 0.898–1.375 | 0.330 |
| Surgery for NEC | 560/16,319 (3.4) | 272/6493 (4.2) | 0.007 | 1.169 | 0.996–1.373 | 0.056 |
| Parenteral nutrition by day 28 | 1476/13,320 (11.1) | 655/5135 (12.8) | 0.001 | 1.103 | 0.980–1.241 | 0.105 |
| Severe IVH | 1188/15,271 (7.8) | 538/6055 (8.9) | 0.008 | 0.975 | 0.861–1.104 | 0.693 |
| Periventricular leucomalacia | 849/15,896 (5.3) | 343/6299 (5.4) | 0.756 | 0.915 | 0.792–1.056 | 0.223 |
| Hydrocephalus surgery | 204/15,941 (1.3) | 74/6302 (1.2) | 0.523 | 0.792 | 0.589–1.064 | 0.121 |
| Severe ROP (>grade 2) | 433/12,076 (3.6) | 203/4733 (4.3) | 0.032 | 1.026 | 0.842–1.251 | 0.796 |
| Surgery for ROP | 486/16,309 (3.0) | 222/6489 (3.4) | 0.090 | 1.014 | 0.847–1.213 | 0.882 |
aOR, adjusted odds ratio; CI, confidence interval; BPD, bronchopulmonary dysplasia; CPAP, continuous positive airway pressure; PMA, postmenstrual age; IVH, intraventricular hemorrhage, ROP, retinopathy of prematurity.
All values are n/N (%), where N is the total number of patients with valid collected result for the indicated variable. In the case of temporal variables (28 days of life or 36 weeks postmenstrual age, PMA) the patients who did not survive to that age were not included in the calculations.
The present study indicated a significant reduction in the number of VLBW infant births during the weekend than on weekdays, as well as an increase in morbidity and mortality, although these differences disappeared after adjusting for confounders. This reduction of births during weekends had already been pointed out by other authors several years ago,1–6 and it is still observed nowadays in different countries.7,12,18,19 It seems unlikely that these differences are due to a biological cycle, and some authors have suggested a relationship with obstetrical interventions such as inductions and elective C-sections.6,18,19 In Spain, the rate of C-sections in this group of patients was 71.4%, and this rate remained stable during the ten-year period of the study, but C-sections were performed more frequently during weekdays. Unfortunately, data concerning induction or indication for C-section were not systematically collected in this database. As shown in Table 1, the present data suggest that in certain high-risk situations (such as multiple gestations, maternal hypertension, and intrauterine growth restriction), a decision to finalize the gestation electively could have been made during weekdays. Despite this, babies born on weekends were smaller, had lower Apgar scores, needed more intervention during resuscitation, and were more unstable in the first 12h of life, exhibiting more morbidity in the bivariate analysis, as well as a 16.2% greater mortality rate when compared with those born on weekdays.
Comparison between studies is difficult, because the definition of weekend itself varies across them. Bell et al.,20 for instance, considered weekend as the period between Friday midnight to Sunday midnight. In other studies, the period was extended until Monday midnight. In the present study, however, it was decided to include until 07:59 am on Monday because care coverage during this time is a prolongation of that on Sunday in the present hospitals. Despite these differences, the results of some studies were similar to the present findings. Gould et al.8 conducted a study in the United States between 1995 and 1997 including patients with all GA and BW. They found a reduction of 17.5% in the number of weekend births, along with a reduction from 22% to 16% in the proportion of C-sections carried out. Neonatal mortality was 2.8‰ among babies born on weekdays vs. 3.1‰ among those born on weekends (OR, 1.12 [95% CI, 1.05–1.19]; p=0.001). Mortality was also higher in babies born by C-section than via vaginal delivery: 6.85‰ vs. 4.94‰, respectively (OR, 1.39 [95% CI, 1.25–1.55]; p<0.001). Nevertheless, in both cases, the statistical differences disappeared after adjusting for BW. Likewise, Luo et al.19 carried out a population-based study in Canada between 1985 and 1998, and reported a 24% reduction in the number of births during the weekends, together with an increase of the relative risk (RR) of stillbirths (RR, 1.06 [95% CI, 1.02–1.09]), and early neonatal mortality (RR, 1.11 [95% CI, 1.07–1.16]), which also disappeared after adjusting for GA in this case. In another population-based study, Salihu et al.21 studied single fetuses with GAs ranging from 20 to 44 weeks, and reported higher mortality among infants born on weekends (3.25‰ vs. 2.87‰). C-section delivery was associated with increased neonatal mortality (HR, 31.47 [95% CI, 15.79–62.74]). In addition, mortality was higher for C-sections carried out during weekends than those carried out on weekdays (HR, 4.00 [95% CI, 1.07–15.03]). Among the sociodemographic factors indicated by the authors as risk factors for neonatal mortality were maternal age <18 years old, black ethnicity, and a lower parental educational level. In that study, mothers older than 35 years had a better prognosis, which is allegedly related to better control of pregnancies and a better compliance of birth plans agreed by parents and professionals. In a recent study in the United Kingdom, after correcting for GA, BW, and maternal age, perinatal mortality was higher among babies born on weekends (aOR, 1.07 [95% CI, 1.02–1.13]), and the incidence of puerperal infections, fetal injuries, and readmissions in the first three days after hospital discharge were also higher among weekend-born babies compared to weekday-born babies.7 That study suggested that during weekends, there would be approximately 770 perinatal deaths and 470 maternal infections more each year than expected if care coverage were uniform throughout the week.
Other studies have shown different results. In a study conducted by Bell et al.22 in a network of university hospitals, residents’ working hours restriction did not influence the risk of neonatal mortality, which in their opinion suggested an appropriate pattern of care coverage by professionals. This fact is relevant in the field of neonatology, because the initial care to the patient in the first few minutes of life significantly contributes to the survival of extremely preterm infants as well as to the short- and long-term clinical results.23 In a recent study by Frank-Wolf et al.,24 although shift time of birth was related to mode of delivery, neonatal morbidity was similar among shifts and between weekends and weekdays.
The present study has some strengths but also limitations. This database collected approximately two-thirds of all VLBW infants in Spain, including most regions, with approximately 60 hospitals, mostly levels 2 and 3, contributing data. This fact reduces the possibility of selection bias, allowing the generalization of results. A potential limitation could be that other holidays were not taken into account, during which the care conditions could be the same as those during Saturdays and Sundays. This is because some holidays vary by communities and/or localities, making it impossible to detect, given the anonymity of cases incorporated into the database. In turn, there may be organizational differences between communities, and the authors do not have specific data regarding the availability of professionals in each center and by days of the week. In addition, if a shortage of professionals or resources during weekends was one of the causes of variations in the number of births or perinatal outcomes, certain periods of the day, such as night shifts, where similar such shortcomings could take place, may have partially masked our results for weekdays. In this sense, it would be interesting to know with certainty the differences in care coverage during night shifts, weekends, and public holidays, and their impact on the results in the different participating centers.25 Another possible limitation is that the study period extended to ten years, during which perinatal care may have varied significantly, which could have affected the morbidity and mortality outcomes. Finally, there are potential biases inherent in this study type, which are derived from unknown confounding factors, which cannot be included and evaluated.
In conclusion, the present results suggest that current care practices tend to cluster high-risk births on weekdays, significantly reducing the number of births on weekends. Paradoxically, this causes urgent and unexpected high-risk deliveries on weekends, increasing the crude morbidity and mortality of patients born during those days. However, after adjusting for risk factors, these differences disappear, suggesting that the coverage of care in these centers is appropriate. However, it is important to emphasize that the analysis carried out in this study is global, including many centers of different categories. The study design does not allow the identification of significant differences between centers. Further studies are required to understand which organizational factors could influence results and, moreover, to compare the systems of different institutions and to generalize those with better results. It is also important to know the possible interrelationships between the maternal, sociodemographic, community, and institutional factors influencing the results of a particular gestation as, undoubtedly, these results have to depend on the healthcare system as a whole.
Conflicts of interestThe authors declare no conflicts of interest.
The authors are greatly indebted to all the participating hospitals and researchers from the Spanish Neonatal Network SEN1500: Complejo Hospitalario Albacete (Andrés Martínez Gutiérrez); Hospital U. de Basurto (Alberto Pérez Legorburu); Hospital Bierzo (María Teresa Prada); Hospital Cabueñes (Rafael García Mozo); Hospital Carlos Haya (Tomás Sánchez Tamayo); Hospital General Castellón (Ramón Aguilera Olmos); Hospital Central Asturias (Belén Fernández Colomer); Hospital Clínic Barcelona (Josep Figuera Aloy); Hospital Clínico San Carlos (Araceli Corredera Sánchez); Hospital Cruces (Amaya Rodríguez Serna); Hospital U. Donostia (M. Ángel Cortajarena Altuna); Hospital Elche (Josep Mut Buigues); Hospital General de Cataluña (Laura Castells Vilella); Hospital G. de Granollers (Israel Anquela Sanz); Hospital Germans Trias i Pujol (W. Coroleu); Hospital Getafe (Lucía Cabanillas Vilaplana); Hospital Infanta Margarita (José María Barcía Ruiz); Hospital Jerez (Dolores Esquivel Mora); Hospital Juan Ramón Jiménez (José Ángel Morilla Sánchez); Hospital Juan XXIII (Mar Albújar); Hospital León (Emilio Álvaro Iglesias); Hospital Miguel Servet (Segundo Rite Gracia); Corporació Parc Taulí (Juan Badia); Hospital San Juan de Deu (Martín Iriondo Sanz); Hospital San Pedro de Logroño (Inés Esteban Díez); Hospital San Pedro de Alcántara (Mª Jesús López Cuesta); Hospital de la Santa Creu i Sant Pau (Gemma Ginovart Galiana); Hospital Severo Ochoa (María José Santos Muñoz); Hospital Txagorritxu (María Mercedes Martínez Ayucar); Hospital Universitario Arnau de Vilanova (Eduard Solé Mir); Hospital Valme (Antonio Gutiérrez Benjumea); Hospital Virgen de la Concha (Víctor Marugán Isabel); Hospital U. Virgen de la Macarena (Mercedes Granero Asencio); Hospital Virgen de la Salud (Alicia de Ureta Huertas); Hospital U. Virgen de las Nieves (Mª Fernanda Moreno Galdó); Hospital Xeral Vigo (María Suárez Albo); Hospital Universitario de Valencia (Javier Estañ Capell); Hospital Universitario de Zaragoza (Purificación Ventura Faci); Hospital Universitario Santiago (Mª Luz Couce Pico); Hospital General de Burgos (Cristina de Frutos Martínez); Hospital General Universitario Alicante (Miriam Salvador Iglesias); Hospital Universitario de Fuenlabrada (Laura Domingo Comeche); Hospital Universitario Gregorio Marañón (Amparo Rodríguez Herreras); Hospital Universitario La Paz (Mª Dolores Elorza); Hospital Materno Infantil de Canarias (Lourdes Urquía Martí);Hospital Universitario Canarias (Pedro A. Fuster Jorge); Hospital Universitario de San Cecilio (Eduardo Narbona); Hospital Universitari i Politecnic La Fe (Isabel Izquierdo Macián); Hospital Universitario Reina Sofía (Juana María Guzmán Cabañas); Hospital Universitario Río Hortera (Mª Mar Montejo Vicente); Hospital Universitario Salamanca (Pilar García González); Hospital Universitario Virgen del Rocío (Carmen Macías Díaz); Hospital Universitario Dexeus (Roser Porta); Scias-Hospital Barcelona (Silvia Martínez-Nadal); Hospital Josep Trueta (Alberto Trujillo); Complejo Hospitalario Universitario de Pontevedra (Javier Vilas González); Hospital Universitario de Ciudad Real (Miguel Ángel Cabezas); Hospital Puerta del Mar (Antonio Segado Arenas); and Hospital Doce de Octubre (Carmen R. Pallás Alonso).
Please cite this article as: García-Muñoz Rodrigo F, García Cruz L, Galán Henríquez G, Urquía Martí L, Rivero Rodríguez S, García-Álix A, et al. Variations in the number of births by day of the week, and morbidity and mortality in very-low-birth-weight infants. J Pediatr (Rio J). 2019;95:41–7.