To evaluate the influence of socioeconomic and psychological factors on glycemic control in young children with type 1 diabetes mellitus.
MethodsThis was a cross-sectional study assessing prepubertal children with type 1 diabetes mellitus. The authors analyzed the socioeconomic status using the Brazil Economic Classification Criterion (Critério de Classificação Econômica Brasil [CCEB]) and psychological conditions through the Brazilian version of the Problem Areas in Diabetes, associated with glycemic control, measured by glycated hemoglobin (HbA1c). Descriptive analysis was used. The variables were assessed by bivariate and multivariate robust Poisson regression model, as well as Fisher's exact and Pearson's chi-squared tests to obtain the ratios of gross and adjusted prevalence ratio, with confidence interval being estimated at 95%.
ResultsA total of 68 children with type 1 diabetes mellitus were included in the study. A negative association between glycemic control (glycated hemoglobin levels), socioeconomic status (Brazil Economic Classification Criterion), and psychological condition (Brazilian version of the Problem Areas in Diabetes) was observed. Among the study participants, 73.5% (n=50) of the children had an unfavorable socioeconomic status; these participants were 1.4 times more likely to present altered glycated hemoglobin values. In relation to individuals with compromised psychological status, 26 (38.2%) had a score above 70, thus being classified with psychological stress; these children were 1.68 times more likely (95% confidence interval: 1.101, 1.301) to have higher glycated hemoglobin levels.
ConclusionsThe socioeconomic conditions and psychological characteristics of the study participants were negatively associated with glycated hemoglobin results. These data reinforce the importance of the studied variables as predictors of glycemic control.
Avaliar a influência dos fatores socioeconômicos e psicológicos no controle glicêmico de crianças pequenas portadoras de diabetes mellitus tipo 1.
MétodosEstudo de corte transversal, avaliou crianças pré-púberes, com diabetes mellitus tipo 1. Foram analisados os fatores socioeconômicos com o Critério de Classificação Econômica Brasil e as condições psicológicas através da versão brasileira do Problem Areas in Diabetes (B-Paid), associado ao controle glicêmico, mensurado pela hemoglobina glicada. Foi utilizada análise descritiva. As variáveis foram avaliadas bivariada e multivariantemente pelo modelo de regressão de Poisson robusto, os testes Exato de Fisher e Qui-Quadrado de Pearson para as razões de prevalência bruta e ajustada, sendo o intervalo de confiança estimado em 95%.
ResultadosForam incluídas no estudo 68 crianças com diabetes mellitustipo 1. Foi observada uma associação negativa entre controle glicêmico (níveis de hemoglobina glicada), status socioeconômico (Critério de Classificação Econômica Brasil) e condição psicológica (versão brasileira do Problem Areas in Diabetes). Entre os participantes do estudo, 73,5% (n = 50) das crianças apresentaram status socioeconômico desfavorável, esses participantes apresentaram 1,4 vezes mais chances de apresentar valores alterados de hemoglobina glicada. Em relação a indivíduos com estado psicológico comprometido, houve uma prevalência de 26 (38,2%) apresentou uma pontuação acima de 70, sendo assim classificada com estresse psicológico, essas crianças foram 1,68 vezes mais prováveis (intervalo de confiança 95%: 1,101, 1,301) de apresentar níveis mais elevados de hemoglobina glicada.
ConclusãoAs condições socioeconômicas e as características psicológicas dos participantes do estudo foram negativamente associadas aos resultados da hemoglobina glicada. Esses dados reforçam a importância das variáveis estudadas como preditores de controle glicêmico.
Diabetes mellitus type 1 (T1DM) is the most common endocrine-metabolic disorder in children and adolescents worldwide, with a prevalence of 190:100,000 among school children in the United States and an annual incidence ranging from 1.7:100,000 (China).1
Globally, the incidence of childhood T1DM increases worldwide at a rate of approximately 3% per year. In 2007, the incidence rate in Brazil was estimated at 7.7:100,000 children per year.2
The increasing incidence of T1DM in developed and developing countries, such as Brazil, is worrisome because T1DM negatively affects the quality and duration of life, mainly due to morbidity and mortality from its chronic complications.3,4
Improved access to care and better health outcomes for young people with T1DM are desirable; however, there is no clear consensus on how best to achieve these goals.5
Despite the considerable progress that has been made, glycemic control in children with T1DM remains suboptimal, thus placing children at risk for developing long-term complications.5 In addition, family factors, psychological characteristics, and economic issues can influence glycemic control.6
Children from low-income background and adverse socioeconomic status are at higher risk of unfavorable glycemic metabolic control, which may be aggravated by its impact on family structure.
Given the importance of using glycemic control to reduce the risk of chronic complications,7,8 this study aimed to evaluate the influence of the socioeconomic and psychological stress factors in glycemic control in children with T1DM followed-up in a public university service. The present findings will be useful during the development of policies and practices aimed to reduce the morbidity and mortality of diseases related to inadequate control of T1DM.
MethodsParticipants and study designThis study used data from the project “Factors associated with glycemic control in children and adolescents with type 1 diabetes mellitus.”9 This cross-sectional study was performed with children with T1DM who came to clinic appointments during the study period (August/2013–January/2014) and met the following selection criteria: clinical diagnosis of T1DM according to the criteria of the American Diabetes Association10; aged 2–9 years; age at diagnosis ≥1 year; records clearly reporting the dosage of HbA1c by high performance liquid chromatography (HPLC); HbA1c measured within the last year; attendance to ≥three consultations per year; and child's and parent/guardian's consent to participate. Children with cognitive impairments that prevented assessment were excluded.
The children followed-up at these services are mostly from a underprivileged socioeconomic background. T1DM medical supplies (i.e., syringes, NPH and regular human insulin, lancets, glucose meters, and glucose strips) are erratically supplied from their hometown health authorities, leading most often to suboptimal glycemic control. In the present study, no patient used insulin infusion pump.
Setting and study populationThe population was composed of 87 children with T1DM, aged 2–9 years, followed-up at the Pediatric Endocrinology Services of two university hospitals. Of the 87 patients eligible patients, 19 were not included because they did not attend the medical visits during the study period. Therefore, a convenience sample of 68 (78.2%) children met the study selection criteria. Parents or caretakers responsible for the children participated in the survey and answered the questionnaires.
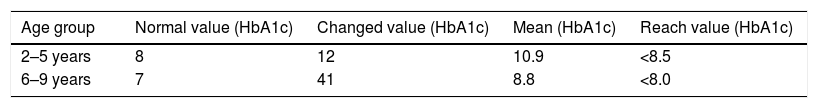
The 68 children were divided into two groups according to their age range: 2–5 years and 6–9 years. To create the groups, during the collection period, the ADA HbA1c desired goals for children were considered: children <6 years, <8.5%; children aged 6–12 years, <8.0%.10
Data collectionThe structured questionnaires were answered in the outpatient clinics on the days of the medical appointments. Due to the young age of the children, the parents or caretakers helped with the responses.
Evaluation of socioeconomic statusData on socioeconomic status were obtained using the Brazil Economic Classification Criterion (Critério De Classificação Econômica Brasil [CCEB]). This is an economic targeting instrument using the household characteristics, presence and quantity of some items, comfort, and level of education of the household head to differentiate the population. The test awards points based on each household characteristic. The sum of these points is then used to divide participants into strata of economic classification, defined as A1, A2, B1, B2, C1, C2, D, and E.
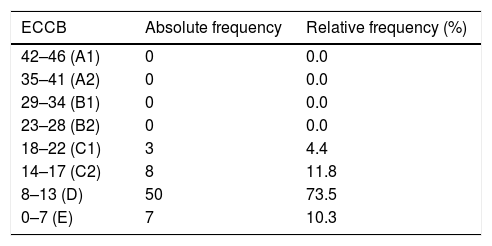
The participants were categorized into the following social classes (A1: 42–46 points, A2: 35–41 points, B1: 29–34 points, B2: 23–28 points, C1: 18–22 points, C2: 14–17 points, D: 8–13 points, and E: 0–7 points). Unfavorable financial situation was diagnosed in participants who scored <10.11
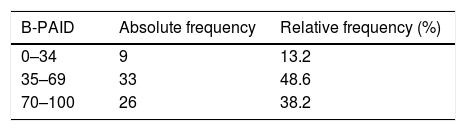
Evaluation of psychological factorsThe influence of psychological factors in the glycemic control was examined using the Problem Areas in Diabetes (PAID) questionnaire, which consists of 20 items focused on the negative emotional aspects of patients with diabetes and can be applied for patients with either T1DM or T2DM. This instrument was translated into Portuguese and validated for Brazil (Brazilian version of the PAID [B-PAID]).12 Each B-PAID item can be scored from 0 (no problem) to 4 (severe problem). The score was transformed into a scale ranging from 0 to 100; the total was reached by adding the answers from 0 to 4 given in the 20 items of the questionnaire, and multiplying the sum by 1.25. A score above 70 indicates greater impairment (psychological stress).12
Evaluation of glycemic controlGlycemic control was assessed by the glycated hemoglobin (HbA1c), which represents the mean glycemia in the last three months (50% of the last month), measured by HPLC. In records with two or more results, the average of HbA1c of the last year was calculated.
As data collection occurred between August/2013 and January/2014, the desired values for HbA1c followed the ADA's recommendations at that time: <8.5% for children <6 years and <8.0% for children aged 6–12 years.10 In 2016, this target value for HbA1c became unique (<7.5%) for all age groups.
Statistical analysisThe assessed variables were sex, age, the participants’ socioeconomic situation, psychological factors, which were presented by the absolute and relative frequencies. Descriptive statistical analysis was performed using the Poisson regression model to directly calculate the gross and adjusted prevalence ratios.13 As the studied children met the criterion of analysis, descriptive statistics were calculated for the level of measurement of the variables of interest.
The participants’ socioeconomic status, psychological condition, and other factors potentially associated with glycemic control were assessed by bivariate and multivariate robust Poisson regression model, Fisher's exact and Pearson's chi-squared tests to obtain the ratios of gross and adjusted prevalence ratio (PR), with confidence interval (CI) being estimated at 95%.
The variables included in the model were those that showed a prevalence difference of >1.3 (30%). Confounding factors were assessed using the percentage difference between PRc and PRad of >10%. Analyses were performed using the statistical package Bioestat (Bioestat, version 5.3, Sociedade Civil de Mamirauá, Belém, Brazil).
Ethical aspectsThe study was approved by the Research Ethics Committee in Human Beings of the Hospital Universitário Prof. Edgard Santos, Universidade Federal da Bahia (UFBA), under No. 42/2013, CAAE: 14859213.0.0000.0049.
As the present study included underage children, the questionnaire was applied after the parents or guardians signed the informed consent form. Patients with unfavorable socioeconomic situation or psychological stress were referred to the clinic staff of Pediatric Endocrinology Outpatients, in order to inform the patients’ conditions and assist them with specialized services.
ResultsA total of 84 children were eligible according to the selection criteria. Of these, 68 children with T1DM were included in the study (mean age 7.1±2.0 years; 28.2% coefficient of variation; range, 2–9 years). A slightly higher prevalence of males was observed: 58.8% (n=40). Of the questionnaires respondents, 76.4% (n=52) were mothers, 10.2% (n=7) were fathers, 8.8% (n=6) were fathers and mothers, and 4.4% (n=3) were grandparents.
Glycemic control was defined by the mean HbA1c level and the patients were divided into two groups according to age: <6 and 6–12 years.10 The 2–5 years group represented 29.4% (n=20) of the sample, while the 6–9 years group accounted for 70.6% (n=48). A total of 80.9% (n=55) of the patients had HbA1c values above the reference values, and only 19.1% (n=13) had values within the expected rate (Table 1).
Classes A1, A2, B1, and B2 were not represented in the study, and the highest proportion of children belonged to class D (73.5%, n=50; Table 2). By B-PAID, 26 children returned a score >70, suggestive of psychological stress (Table 3).
Distribution of socioeconomic condition as a result of the CCEB.
| ECCB | Absolute frequency | Relative frequency (%) |
|---|---|---|
| 42–46 (A1) | 0 | 0.0 |
| 35–41 (A2) | 0 | 0.0 |
| 29–34 (B1) | 0 | 0.0 |
| 23–28 (B2) | 0 | 0.0 |
| 18–22 (C1) | 3 | 4.4 |
| 14–17 (C2) | 8 | 11.8 |
| 8–13 (D) | 50 | 73.5 |
| 0–7 (E) | 7 | 10.3 |
CCEB, Critério de Classificação Econômica Brasil.
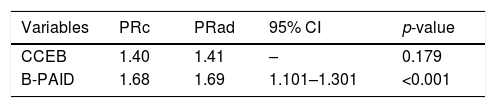
A negative association between glycemic control (HbA1c levels), socioeconomic status (CCEB), and psychological condition (B-PAID) was observed. Among the study participants, 73.5% (n=50) of the children had unfavorable socioeconomic status; 78.0% (n=39) had elevated levels of HbA1c and 55.6% (n=11) were classified with appropriate glycemic control. These participants were 1.4 times more likely to present altered HbA1c values.
In relation to individuals with compromised psychological status, a prevalence of 96.2% (n=25) was observed in patients with elevated HbA1c levels, and 57.1% (n=24) presented adequate glycemic control. These children were 1.68 times more likely (95% CI: 1.101, 1.301) to have higher HbA1c levels (Table 4).
Distribution of gross prevalence ratio (PRg) and adjusted (PRad) values, confidence interval (CI) and p-value of the variables socioeconomic status (CCEB) and psychological conditions (B-PAID) for association with glycemic control (HbA1c).
| Variables | PRc | PRad | 95% CI | p-value |
|---|---|---|---|---|
| CCEB | 1.40 | 1.41 | – | 0.179 |
| B-PAID | 1.68 | 1.69 | 1.101–1.301 | <0.001 |
Note: Values associated with the HbA1c results of the participants using a robust Poisson regression model.
CCEB, Critério de Classificação Econômica Brasil; B-PAID, Brazilian version of the Problem Areas in Diabetes instrument.
T1DM has a peak incidence at 5–7 years of age.14 Data from the literature state that there is no gender predilection, but in the present study there was a slight predominance of T1DM in boys.
The greater participation of mothers in the present study is justified by the young age of the children and by the cultural values, where mothers assume the responsibilities of their children's medical care. Specifically in the case of T1DM, they are responsible for checking the eating habits, stimulating the practice of physical activities, controlling blood glucose levels, accompanying the consultations and hospitalizations, and giving emotional support to the child.15
Glycemic control analysis, measured by the HbA1c outcome, showed that most participants had worse than expected results, with only a small portion returning to proper values, according to the ADA parameters.10 If smaller cutoff points for HbA1c were used, based on the ADA proposal from 2016, the percentage of patients with adequate control would remain low. These data are similar with other studies, and the treatment goals proposed by the ADA were reached by a minority of patients.16,17 Jose et al.18 found similar results to those of the present study, and highlighted difficulties in maintaining lower levels of HbA1c even in reference centers.
In the present study, a negative association was observed between socioeconomic and psychological factors with glycemic control in children. Haller et al.19,20 have stressed how the health team should aim beyond the measurement of blood glucose levels and preventing complications, considering also the social, economic, and psychological conditions, as well as child development.
Interestingly, socioeconomic status was not a significant predictor of HbA1c; nonetheless, the present study identified an association between low economic status and poor glycemic control; the economic problems of developing countries, such as Brazil, should be considered an obstacle to intensive treatment of T1DM.20
Moreover, Walsh et al.20 found that investment and per capita spending on healthcare has an inverse correlation with levels of HbA1c and complications. Hassan et al.21 reported that lower socioeconomic status groups have worse metabolic control, due to the unavailability of care. Thus, for the adequate management of T1DM, some tasks require the acquisition of materials such as insulin, syringes, needles, and strips for the blood glucose test. As most patients belong to a low-income population, free distribution of the material through governmental authorities is necessary. However, not all T1DM patients benefit from the free dispensing of these supplies, having to acquire them with their own resources. According to Castro et al.,22 such expenditures directly affect low-income families, aggravating the economic and psychological situation of families and patients with T1DM. Patients in the public healthcare system have a poor control of diabetes due to their limited financial conditions.
The psychological condition was significantly associated with HbA1c levels in the present sample. The association between psychological aspects of type 1 diabetes with poor glycemic control is in line with other studies.23,24 The International Society for Pediatric and Adolescent Diabetes recommends routine screening for psychosocial concerns in children and adolescents with T1DM, to identify the need for specialized counseling.25 The ADA10 also recommends routine evaluation of psychological problems and family tensions that may impact adherence and diabetes management.
Gross et al.12 also observed a significant association between PAID score and HbA1c levels in patients with T1DM. In Brazilian patients, younger and less educated participants presented greater stress in relation to T1DM; the authors suggest that these should be prioritized in calls.12
Al-Odayani et al.26 found that chronic conditions such T1DM can significantly and permanently interfere with the emotional, physical and social development of children, and can also affect relationships and family lifestyle. In this regard, greater attention should be given to this aspect when designing care and prevention measures.
The present study indicated a significant interaction between psychological and socioeconomic factors with glycemic control of the study participants. Rechenberg et al.27 also studied the relationship between glycemic control, self-care, and psychosocial outcomes based on different income levels and found that children/adolescents from high-income families tended to have significantly lower HbA1c levels than those from families of moderate to low income. Therefore, interventions for children with T1DM and their families should include educational and psychological support, as well as attention to their financial needs.28
Strengths of the present study include the fact that it was performed in a low-income population, contributing to understand the behavior of the disease in this public; this study generated original information about children with T1DM from Bahia and pointed out directions for future research. The primary limitation was the sample size. While the present study garnered a diverse population, its sample size was not large enough to allow a robust analysis. The study should be replicated with a random sample with a wider geographical representativeness. Another important limitation of the study was its design, which does not allow the performance of probabilistic statistics; however, it showed advantages due to analytical simplicity, high descriptive potential, and the fact that it is useful in health planning and in the formulation of hypotheses.
In conclusion, the glycemic control of the children was unsatisfactory (much higher than expected HbA1c values). The results suggest that the socioeconomic conditions and psychological characteristics of the study participants were negatively associated with HbA1c results. These data reinforces the importance of the studied variables as predictors of glycemic control.
FundingThis study was partially funded by a grant of the Fundação de Amparo à Pesquisa do Estado da Bahia (FAPESB).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Andrade CJ, Alves CA. Influence of socioeconomic and psychological factors in glycemic control in young children with type 1 diabetes mellitus. J Pediatr (Rio J). 2019;95:48–53.