To validate the Subjective Global Nutritional Assessment (SGNA) questionnaire for Brazilian children and adolescents.
MethodsA cross-sectional study with 242 patients, aged 30 days to 13 years, treated in pediatric units of a tertiary hospital with acute illness and minimum hospitalization of 24h. After permission from the authors of the original study, the following criteria were observed to obtain the validation of SGNA instruments: translation and backtranslation, concurrent validity, predictive validity, and inter-observer reliability. The variables studied were age, sex, weight and length at birth, prematurity, and anthropometry (weight, height, body mass index, upper arm circumference, triceps skinfold, and subscapular skinfold). The primary outcome was considered as the need for admission/readmission within 30 days after hospital discharge. Statistical tests used included ANOVA, Kruskal–Wallis, Mann–Whitney, chi-square, and Kappa coefficient.
ResultsAccording to SGNA score, 80% of patients were considered as well nourished, 14.5% moderately malnourished, and 5.4% severely malnourished. Concurrent validity showed a weak correlation between the SGNA and anthropometric measurements (p<0.001). Regarding predictive power, the main outcome associated with SGNA was length of admission/readmission. Secondary outcomes associated included the following: length of stay at the unit after SGNA, weight and length at birth, and prematurity (p<0.05). The interobserver reliability showed good agreement among examiners (Kappa=0.74).
ConclusionThis study validated the SGNA in this group of hospitalized pediatric patients, ensuring its use in the clinical setting and for research purposes in the Brazilian population.
Validar o questionário de Avaliação Nutricional Subjetiva Global (ANSG) para a população de crianças e adolescentes brasileiros.
MétodosEstudo transversal, realizado com 242 pacientes, de 30 dias a 13 anos, atendidos em unidades pediátricas de um hospital terciário, com doenças agudas e tempo de permanência mínima de 24 horas hospitalizados. Após autorização dos autores do estudo original foram realizadas as seguintes etapas para obtenção da validação dos instrumentos de ANSG: tradução (backtranslation), validade de critério concorrente e preditiva e confiabilidade interobservador. As variáveis em estudo foram: idade, sexo, peso e comprimento ao nascer, prematuridade e antropometria (peso, estatura, índice de massa corporal, circunferência braquial, dobra cutânea tricipital e dobra cutânea subescapular). O desfecho principal considerado foi necessidade de internação/reinternação até 30 dias após a alta hospitalar. Os testes estatísticos utilizados foram: ANOVA, Kruskal–Wallis, Mann–Whitney, Qui-quadrado e coeficiente Kappa.
ResultadosDe acordo com a classificação do ANSG 80% dos pacientes foram classificados como bem nutridos, 14.5% moderadamente desnutridos e 5.4% gravemente desnutridos. A validade concorrente mostrou fraca a regular correlação do ANSG com as medidas antropométricas utilizadas (p<0.001). Quanto ao poder preditivo, desfecho principal associado ao ANSG foi tempo de internação/reinternação. Os desfechos secundários associados foram: tempo de permanência na unidade após ANSG, peso e comprimento ao nascer e prematuridade (p<0.05). A confiabilidade interobservador mostrou boa concordância entre os avaliadores (Kappa=0.74).
ConclusãoEste estudo validou o método de ANSG nessa amostra de pacientes pediátricos hospitalizados, possibilitando seu uso para fins de aplicação clínica e de pesquisa na população brasileira.
In recent decades, there has been a significant reduction in the prevalence of worldwide malnutrition in children.1 Nevertheless, death rates due to severe malnutrition in children undergoing hospital treatment remain high.2–4 Several studies have reported a prevalence of malnutrition related to an underlying disease of 6–51% in hospitalized children.5–7
However, the lack of consensus regarding the definition, heterogeneous nutritional screening methods, and the fact that nutrition is not prioritized as part of patient care are some of the factors responsible for the under-recognition of malnutrition prevalence and its impact on clinical results. Recently, a new definition of hospital malnutrition in children has been used. This definition incorporates the concepts of chronicity, etiology and pathogenesis of malnutrition, its association with inflammation, and its impact on body functional alterations.8
Thus, it is crucial to know and monitor the nutritional status of hospitalized children, to better understand factors contributing to the occurrence of complications, increased length of hospital stay, and consequent increase in health system costs.5,9–11
Subjective nutritional assessment is an evaluation method based on clinical judgment and has been widely used to assess the nutritional status of adults for clinical research purposes,7 considered a predictor of morbidity and mortality.12 It differs from other nutritional assessment methods by encompassing not only body composition alterations but also patient functional impairment,13 assessing the possible presence of nutritional risks, based on clinical history and physical examination. It is a simple, fast, inexpensive, and non-invasive method that can be performed at the bedside.12
The questionnaire adapted by Secker and Jeejeebhoy7 for the pediatric population has been termed the Subjective Global Nutritional Assessment (SGNA), and evaluates the following parameters: the child's current height and weight history, parental height, food consumption, frequency and duration of gastrointestinal symptoms, and current functional capacity and recent alterations. It also associates nutrition with physical examination.
The presence of functional alterations appears to be the determining factor in the occurrence of complications associated with malnutrition. Thus, it is of utmost importance to attain early detection of nutritional risk through a method that is adequate, sensitive to identify early alterations, specific enough to be changed only by nutritional imbalances, and corrected based on a nutrition intervention.14
Considering the need to validate a reliable method of nutritional assessment for children and adolescents in Brazil, the aim of this study was to validate the SGNA in a population of Brazilian children and adolescents.
MethodsPopulationThis was a cross-sectional study carried out with 242 patients aged 30 days to 13 years, in the city of Porto Alegre, RS, Southern Brazil. Patients were enrolled in the Pediatric Emergency and Inpatient Units of Hospital de Clinicas de Porto Alegre, RS, considering as a study factor the nutritional status assessment based on objective and subjective data. The analyzed outcomes were need for hospital admission (patients from the emergency observation room) or readmission (patients from the pediatric ward). Data collection occurred from May 2012 to June 2013.
The study inclusion criteria were the following: children and adolescents, aged 30 days to 19 years, of both genders, with clinical diagnosis of acute diseases15 and minimum length of stay of 24h in the Pediatric Emergency and Inpatient Units.
Exclusion criteria were as follows: neuropsychomotor development delay (according to parental information); underlying chronic diseases (congenital malformations, inborn errors of metabolism, heart disease, neuropathy, liver disease, immunocompromised patients, children of HIV+ mothers); chronic use of medication except for ferrous sulfate and multivitamins at prophylactic doses; hospital admission in the 30-day period prior to the study assessment; patients younger than one month; infectious process in the past seven days; incapacity to perform anthropometric measurements; and patients and caregivers who did not speak Portuguese. The clinical information related to the underlying diseases were collected from medical records and confirmed by the assistant medical team.
The research project designed for the development of this study was approved by the Research Ethics Committee of Hospital de Clínicas de Porto Alegre (Project No. 11-0339). Parents and/or guardians signed an informed consent prior to study enrollment.
Tool validation processInitially permission was obtained from the authors to reproduce and use the SGNA questionnaires originating from the PhD thesis entitled “Nutritional Assessment in Children: A Comparison of Clinical Judgment and Objective Measures.”16 Next, the questionnaires were translated through the back-translation method,17 according to the following steps: first, translation from English into Portuguese; subsequently, the new questionnaires were translated from Portuguese back into English.
At the third step, a comparison of the tools was performed by a bilingual translator whose native language is English, who verified whether the new questionnaires were accurate according to the original content and structure. The steps of this translation process were performed by three independent translators. Subsequently, translation validation was performed, consisting of the reliability and validity assessment.
Study designAfter researcher training to standardize collection of anthropometric measurements18 and SGNA questionnaire use,7,19 each child was assessed by two independent researchers blinded to each other; one researcher collected anthropometric data, whereas the other applied the SGNA questionnaire. To test SGNA interobserver reproducibility, 61 randomly selected patients (25% of the study population) were evaluated by a third collaborator, who also applied the SGNA questionnaire.
The objective and subjective data were collected within 48h after patient hospital admission. Thirty days after patient hospital discharge, a search was carried out in the medical files to observe the outcome of need for hospital admission/readmission. Data were entered into a database using Microsoft Excel software (Microsoft®, 2007, USA) and exported to SPSS (version 18.0, Chicago, USA). Anthro and AnthroPlus software (version 3.2.2, World Health Organization, Geneva, Switzerland) were used to assess anthropometric data.
Subjective global nutritional assessmentThe evaluators used the SGNA questionnaire (Appendixes A and B) to guide the interview and obtain information from the patient's medical history, such as the patient's current height and weight history, parental heights, food consumption (volume, type, and frequency of feedings, liquid and solid foods for infants, feeding frequency, and brief description of food ingestion on a typical day; appetite assessment and recent changes; food ingestion or dietary problems and restrictions), frequency and duration of gastrointestinal symptoms (loss of appetite, vomiting, diarrhea, constipation, abdominal pain, and nausea) and current functional capacity and recent changes (alertness, amount of energy or activity and school attendance, capacity to run and play games or sports, and time of sleep). The questionnaire also correlates nutrition with the physical examination, focusing on specific body sites to detect signs of fat (cheeks, biceps and triceps, ribs, and buttocks) and muscle loss (clavicle, shoulder, scapula, quadriceps, knee, and calf), as well as edema (ankles and sacrum). It considers the presence or absence of specific history characteristics, the metabolic demands of the underlying condition, and physical signs associated with malnutrition, attaining an overall assessment of patient nutritional status and an overall classification: well-nourished, moderately malnourished, or severely malnourished (Appendix C). The SGNA does not use a rigid scoring system based on specific criteria.7
Objective nutritional assessmentThe following anthropometric measurements were analyzed: weight and height; body mass index (BMI); upper arm circumference (AC); triceps skinfold (TSF), and subscapular skinfold (SSF). For children younger than 24 months, weight was measured with the children wearing no clothes or diapers. Children older than 24 months and adolescents were weighed with a gown and without shoes. A Filizola® electronic scale (Filizola®, SP, Brazil) was used to measure weight.
Height measurements were performed using a wood board with a fixed blade on one side and moveable on the other, the top of the head on the fixed part (WCS®, Brazil), with the moveable part arranged to be in parallel with the child's legs. In children younger than 24 months, the length was measured in the supine position by measuring with a ruler attached to the board. Children older than 24 months and adolescents were measured in the standing position with an anthropometric ruler (WISO®, Brazil) fixed on the wall and mobile cursor graduated in centimeters.
AC measurements were measured using a flexible and retractable fiberglass measuring tape, surrounding the middle portion of the non-dominant arm, with the arm relaxed. TSF measurements were performed in the posterior region of the non-dominant arm, parallel to the longitudinal axis, at midpoint between the acromion and olecranon. SSF measurements were performed with the non-dominant arm relaxed at the side of the body, obliquely to the longitudinal axis, following the orientation of the ribs, located two centimeters below the lower angle of the scapula.
The skinfolds were measured in triplicate using a scientific adipometer (Cescorf®, Brazil). All equipment was calibrated and the techniques used to obtain measurements were standardized.18 The anthropometric assessment and nutritional status classification were carried out based on the following criteria and tools of the WHO20,21:
Children aged zero to five years: the WHO's Anthro Plus software (version 3.2.2, 2011, World Health Organization, Geneva, Switzerland) was used, which determines z-scores for the weight/height (W/H), weight/age (W/A), height/age (H/A), body mass index/age (BMI/A), upper arm circumference/age (AC/A), tricipital skinfold/age (TSF/A), and subscapular skinfold/Age (SSF/A) ratios.
Children older than five years: the WHO's Anthro Plus software (version 3.2.2, 2009, World Health Organization, Geneva, Switzerland) was used, which determines z-scores for W/A, H/A, and BMI/A ratios. z-score data for AC/A, TSF/A and SSF/A ratios were evaluated according to the reference values of Frisancho.22 The premature infants (n=18) were evaluated using the corrected age up to 2 years.23
Statistical analysisSample size was calculated considering the means and standard deviation of hospital length of stay found in the study by Secker and Jeejeebhoy,7 of 5.3±5.0 days for the group of well-nourished children and 8.2±10 days for the group of malnourished children, with a power of 80% and a significance level of 0.05, resulting in a total of 236 patients. The required sample size to test interobserver reliability was calculated based on the Kappa value of 0.6, considering a power of 80% and significance level of 0.05, resulting in a subgroup of 61 patients.
Quantitative variables were expressed as mean and standard deviation or median and interquartile range. Categorical variables were described as absolute and relative frequencies. One-way ANOVA with post hoc Tukey test was applied to compare means between groups. In case of asymmetry, Kruskal–Wallis test was used. When comparing proportions between groups, Pearson's chi-squared test and prevalence ratio with a 95% confidence interval were applied. The association between nutritional assessment methods was assessed by Kendall coefficient. The agreement between the methods was evaluated by Kappa coefficient. The significance level was set at 5% (p<0.05).
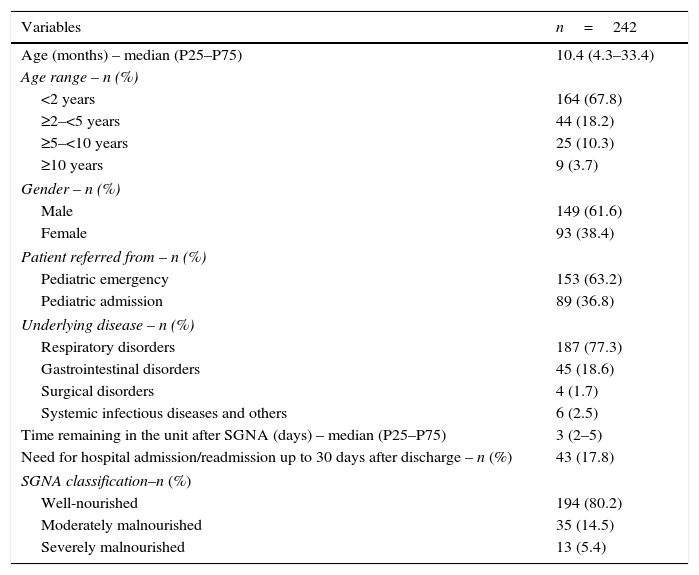
ResultsThe sample comprised 242 patients, with a median age of approximately 10 months (25th–75th percentiles: 4.3–33.4), with minimum of one month and a maximum of 162 months. The age range younger than 2 years predominated (67.8%), as well as the male gender (61.6%). Sample characterization is shown in Table 1.
Characterization of the study sample.
| Variables | n=242 |
|---|---|
| Age (months) – median (P25–P75) | 10.4 (4.3–33.4) |
| Age range – n (%) | |
| <2 years | 164 (67.8) |
| ≥2–<5 years | 44 (18.2) |
| ≥5–<10 years | 25 (10.3) |
| ≥10 years | 9 (3.7) |
| Gender – n (%) | |
| Male | 149 (61.6) |
| Female | 93 (38.4) |
| Patient referred from – n (%) | |
| Pediatric emergency | 153 (63.2) |
| Pediatric admission | 89 (36.8) |
| Underlying disease – n (%) | |
| Respiratory disorders | 187 (77.3) |
| Gastrointestinal disorders | 45 (18.6) |
| Surgical disorders | 4 (1.7) |
| Systemic infectious diseases and others | 6 (2.5) |
| Time remaining in the unit after SGNA (days) – median (P25–P75) | 3 (2–5) |
| Need for hospital admission/readmission up to 30 days after discharge – n (%) | 43 (17.8) |
| SGNA classification–n (%) | |
| Well-nourished | 194 (80.2) |
| Moderately malnourished | 35 (14.5) |
| Severely malnourished | 13 (5.4) |
SGNA, Subjective Global Nutritional Assessment.
Data were expressed as mean±standard deviation, median (P25–P75), or absolute number (%) as indicated.
Of the total sample, 153 patients were treated at the Emergency Pediatric Unit (63.2%) and 89 at the Inpatient Pediatric Unit (36.8%). The most frequent diagnosis was respiratory disease (77.3%), followed by gastrointestinal disease (18.6%).
Psychometric propertiesConcurrent validityNutritional status, as determined by the SGNA, was compared with anthropometric measurements. According to the SGNA, 194 patients (80.2%) were classified as well-nourished, 35 patients (14.5%) as moderately malnourished, and 13 patients (5.4%) as severely malnourished.
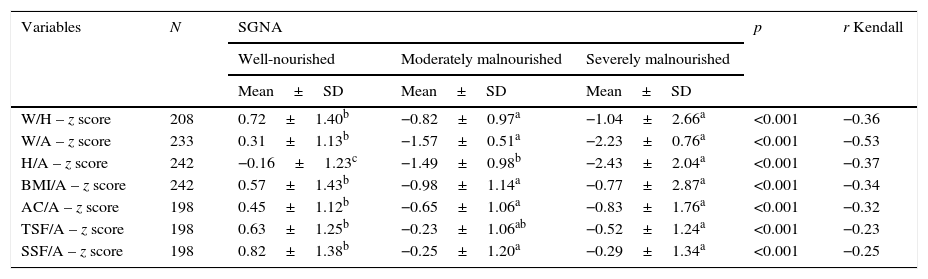
Overall, there was a significant difference between the groups; the group classified as well-nourished showed significantly higher values than the other two (moderately and severely malnourished) in all nutritional assessment methods (objective and subjective). However, among the moderately and severely malnourished, the difference was only significant in relation to height/age ratio (Table 2). Kendall coefficients disclosed the weak-to-regular associations between the nutritional assessment methods. The ratio that showed the greatest association with SGNA was weight/age.
Association between Subjective Global Nutritional Assessment (SGNA) data and objective anthropometric measurements (z-score).
| Variables | N | SGNA | p | r Kendall | ||
|---|---|---|---|---|---|---|
| Well-nourished | Moderately malnourished | Severely malnourished | ||||
| Mean±SD | Mean±SD | Mean±SD | ||||
| W/H – z score | 208 | 0.72±1.40b | −0.82±0.97a | −1.04±2.66a | <0.001 | −0.36 |
| W/A – z score | 233 | 0.31±1.13b | −1.57±0.51a | −2.23±0.76a | <0.001 | −0.53 |
| H/A – z score | 242 | −0.16±1.23c | −1.49±0.98b | −2.43±2.04a | <0.001 | −0.37 |
| BMI/A – z score | 242 | 0.57±1.43b | −0.98±1.14a | −0.77±2.87a | <0.001 | −0.34 |
| AC/A – z score | 198 | 0.45±1.12b | −0.65±1.06a | −0.83±1.76a | <0.001 | −0.32 |
| TSF/A – z score | 198 | 0.63±1.25b | −0.23±1.06ab | −0.52±1.24a | <0.001 | −0.23 |
| SSF/A – z score | 198 | 0.82±1.38b | −0.25±1.20a | −0.29±1.34a | <0.001 | −0.25 |
SGNA, subjective global nutritional assessment; W/H, weight for height; W/A, weight for age; H/A, height for age; BMI/A, body mass index for age; AC/A, upper arm circumference for age; TSF/A, triceps skinfold thickness for age; SSF/A, subscapular skinfold thickness for age.
Data were expressed as mean±standard deviation.
a,b Equal letters do not differ by Tukey test at the 5% significance level.
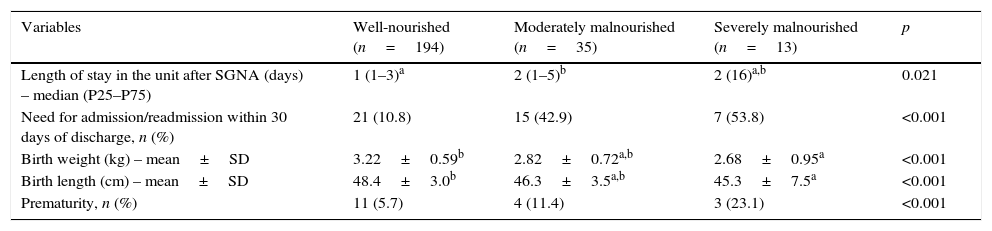
The need for hospital admission/readmission occurred in 43 cases (17.8%). The median (25th–75th percentiles) of time of admission/readmission was two days. The probability of admission/readmission was approximately four times higher in moderately malnourished patients when compared to normal weight ones (PR=3.96; 95% CI: 2.27–6.91). In severely malnourished patients, the probability of hospital admission/readmission was approximately five times greater when compared to normal weight ones (PR=4.97; 95% CI: 2.61–9.48).
Nutritional status classified by SGNA was associated with all assessed outcomes (Table 3). Patients considered by SGNA as severely malnourished had lower weight and length at birth than the group of patients considered well nourished (p<0.05). Moreover, the need for hospital admission/readmission and prematurity increased with an increasing degree of malnutrition (p<0.001).
Association between Subjective Global Nutritional Assessment (SGNA) data and outcomes.
| Variables | Well-nourished (n=194) | Moderately malnourished (n=35) | Severely malnourished (n=13) | p |
|---|---|---|---|---|
| Length of stay in the unit after SGNA (days) – median (P25–P75) | 1 (1–3)a | 2 (1–5)b | 2 (16)a,b | 0.021 |
| Need for admission/readmission within 30 days of discharge, n (%) | 21 (10.8) | 15 (42.9) | 7 (53.8) | <0.001 |
| Birth weight (kg) – mean±SD | 3.22±0.59b | 2.82±0.72a,b | 2.68±0.95a | <0.001 |
| Birth length (cm) – mean±SD | 48.4±3.0b | 46.3±3.5a,b | 45.3±7.5a | <0.001 |
| Prematurity, n (%) | 11 (5.7) | 4 (11.4) | 3 (23.1) | <0.001 |
SGNA, Subjective Global Nutritional Assessment.
Data were expressed as mean±standard deviation, median (P25–P75), or absolute number (%) as indicated.
a,b Equal letters do not differ by Tukey test at 5% significance level.
There was good interobserver agreement (kappa=0.74; p<0.001), and the percentage of well-nourished, moderately malnourished, and severely malnourished individuals were similar for the two observers. The correlation occurred in 56 of 61 cases (92%).
DiscussionSubjective global assessment has been widely used, as it is an easy-to-perform method that does not require expensive resources and can be performed by professionals that comprise the multidisciplinary team.14
This study translated and validated the SGNA for the Brazilian pediatric population, through the following psychometric properties: concurrent and predictive validity and interobserver reliability.
Concurrent validity assesses the correlation of the tool with another measure (the gold standard) used to measure what is being assessed, both applied simultaneously.24 This study found a significant association between SGNA and commonly used anthropometric measures, as reported by Brazilian studies involving adults with different pathologies.3,25–27 The results were also similar to those found in the original study by Seeker and Jeejeebhoy7 involving children undergoing small surgical procedures. However, it is noteworthy that the agreement observed between the methods, SGNA and anthropometric measures, was weak-to-regular in this study (p<0.001).
The predictive validity includes future predictions, regarding the quality with which a tool can predict a future criterion.24 The nutritional status evaluated by SGNA was associated with all assessed outcomes (need for hospital admission/readmission within 30 days after hospital discharge, length of hospital stay after SGNA, weight and length at birth, and prematurity) (p<0.05). An increasing degree of malnutrition according to the SGNA classification was associated with increased complications. Studies using subjective assessment as an evaluation method of the nutritional status of hospitalized patients have also shown this power.7,26,28
The interobserver reliability evaluates the reproducibility of a tool through its application by two or more observers.24 In this study, there was good reliability (Kappa=0.74; p<0.001), higher than the one found in the original study by Secker and Jeejeebhoy.7
Because this is a subjective method, the SGNA diagnostic accuracy depends on observer's experience and training, which is its main disadvantage. However, studies carried out with adults also attained a level of agreement similar to that obtained in this study. In an early study on nutritional status assessment, Baker et al.15 showed good agreement between their evaluators (Kappa=0.72), as well as Detsky et al.29 when they standardized the clinical method, creating a subjective nutritional assessment questionnaire (Kappa=0.78). In more recent studies, a weak-to-moderate concordance was observed between the evaluators. Secker and Jeejeebhoy,7 studying surgical pediatric patients in a hospital in Canada, obtained Kappa=0.28. Beguetto et al.,30 studying adult patients admitted to a university general hospital in Porto Alegre, RS, found Kappa=0.46.
The evaluation of the psychometric properties of the SGNA in this study showed the tool has good interobserver reliability, in addition to having confirmed the concurrent and predictive validity of the questionnaires. Its application in Brazilian children and adolescents and in different clinical situations from that of the original study showed good results. After the translation and study of the psychometric properties of the SGNA, the tool showed to be reliable and valid for assessing the nutritional status of children and adolescents.
In this study, hospital stay showed no association with the SGNA, unlike what other studies reported.7,9,25 A possible explanation may be due to the fact that the selected patients had acute diseases and were admitted through the Pediatric Emergency Unit. In the study by Secker and Jeejeebhoy,7 patients were from the Surgical Inpatient Pediatric Unit.
A limitation of this study was the difficulty of performing biochemical tests to confirm the diagnosis of the patient's nutritional status. However, the positive aspect of the study was the demonstration of the high sensitivity of the SGNA questionnaire for nutritional risk and malnutrition diagnosis. The fact that it considers the clinical and functional alterations, which can lead the patient to a situation of protein, energy, and immune competence loss, favored the immediate diagnosis of nutritional risk and malnutrition.
SGNA validation for the Brazilian pediatric population can be a stimulus for the utilization of this method as systematic assessment in pediatric services, in different clinical situations. This can be performed as soon as the patient arrives at the hospital, facilitating the identification of those who may be at nutritional risk, so that the most appropriate nutritional intervention can be performed.
The methodology used and the careful translation process allow for the conclusion that SGNA is a valid and reliable instrument for the assessment of the nutritional status of Brazilian pediatric patients.
SGNA is a useful diagnostic tool for assessing nutritional status, with similar efficacy to anthropometric parameters, regardless of the clinical status of patients. This study validated the SGNA questionnaire in this sample of hospitalized pediatric patients, allowing its use for clinical applications and for research purposes in the Brazilian population.
FundingThe study received support from FIPE, Research and Graduate Study Group, Hospital de Clinicas de Porto Alegre and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Conflicts of interestThe authors declare no conflicts of interest.
The study received financial support from FIPE and CAPES.
Please cite this article as: Carniel MP, Santetti D, Andrade JS, Favero BP, Moschen T, Campos PA, et al. Validation of a subjective global assessment questionnaire. J Pediatr (Rio J). 2015;91:596–602.
The study was conducted at Postgraduate Program in Child and Adolescent Health, Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.