The aim of this study was to translate and validate the Pediatric Daytime Sleepiness Scale (PDSS) into Brazilian Portuguese.
MethodsThe translation/validation process was carried out through translation, back translation, technical review, assessment of verbal comprehension/clarity of the scale by experts and a focus group, test–retest, and application of the tool. The reproducibility analysis was performed by applying the PDSS in test–retest; internal consistency was verified by applying the scale in 90 children and adolescents.
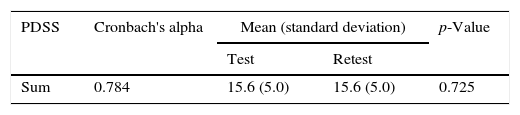
ResultsThe mean score of the sum of PDSS questions was 15.6 (SD=5.0) points. The PDSS showed appropriate indicators of content validation and clarity for the Brazilian Portuguese version. The internal consistency analysis showed a Cronbach's alpha of 0.784. The PDSS showed adequate reproducibility. The PDSS scores showed a significant and negative correlation with time spent in bed (r=−0.214; p=0.023).
ConclusionThe Brazilian Portuguese version of the PDSS shows satisfactory indicators of validity and can be applied in clinical practice and scientific research.
Este estudo teve como objetivo traduzir e validar Pediatric Daytime Sleepiness Scale (PDSS) para o português (Brasil).
MétodoO processo da tradução/validação deu-se por meio da tradução, retro tradução, revisão técnica, avaliação da compreensão verbal/clareza do questionário por especialistas e por grupo focal, teste-reteste e aplicação do instrumento. A análise de reprodutibilidade realizou-se por meio da aplicação da PDSS em teste-reteste e a consistência interna pela aplicação da escala em 90 crianças e adolescentes.
ResultadosA pontuação média verificada no somatório das questões da PDSS foi 15,6(5,0) pontos. A PDSS apresentou adequados indicadores de validade de conteúdo e clareza de linguagem em português do Brasil. A análise da consistência interna identificou alfa de Cronbach de 0,784. A PDSS apresentou adequada reprodutibilidade. Os escores da PDSS apresentaram correlação negativa e significativa com o tempo na cama (r=-0,214; p=0,023).
ConclusõesA versão em português da PDSS apresenta satisfatórios indicadores de validade podendo ser aplicada na prática clínica e em pesquisas científicas.
Excessive daytime sleepiness (EDS) is characterized by an increased sensation of sleepiness and decreased alertness.1,2 It is one of the main effects of low-duration and/or poor-quality sleep, and is associated with learning and behavioral problems, low cognitive performance, and attention and concentration deficits.3–7 EDS can be observed at all stages of life. However, studies point to its increase in prevalence in adolescence, a life stage in which a delayed sleep phase characterized by later times to sleep and wake8,9 and reduced sleeping hours10 can be observed. Gibson et al.9 identified 68% of adolescents with EDS in the early hours of the morning in a study performed in Canada. Similarly, Souza et al.,11 in a sample of Brazilian adolescents, identified a prevalence of 55.8% of EDS. Nevertheless, as discussed by Pereira et al.,2 Brazilian literature is scarce with regard to the procedures and tools to evaluate EDS in children and adolescents.
The gold standard for EDS assessment is the Multiple Sleep Latency Test, which is performed in the laboratory, making this assessment unfeasible in many circumstances.12 Regarding the most widely used questionnaire to assess EDS, the Epworth scale,13 it has important limitations related to the content of its questions to be used in pediatric populations.
The Pediatric Daytime Sleepiness Scale (PDSS), by Drake et al.,3 has been used in studies with foreign samples3,7,14–17 and constitutes an important tool for the assessment of excessive daytime sleepiness in children and adolescents. However, translation and validation studies of this scale for use in Brazil were not found in the literature. The aim of this study was to translate and validate the PDSS into Brazilian Portuguese.
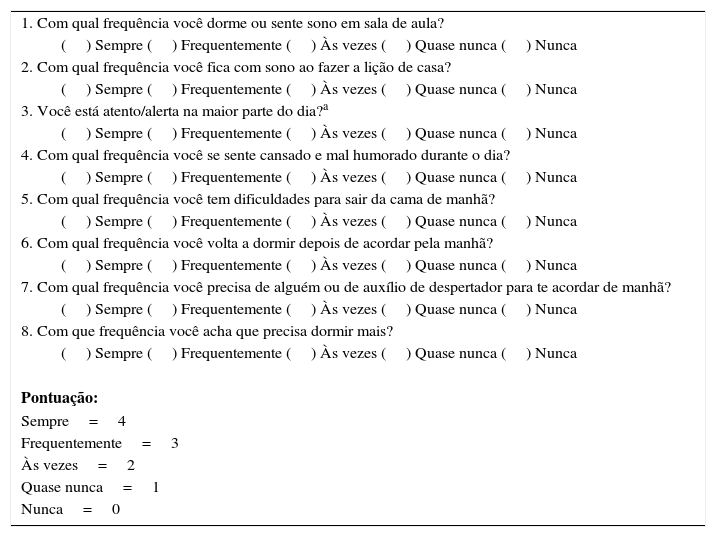
MethodThe PDSS aims to assess the occurrence of EDS, and was validated for children and adolescents aged 11–15 years.3 It consists of eight multiple choice questions. Each question has five response options, using a Likert scale: 0=never; 1=almost never; 2=sometimes; 3=frequently, and 4=always. The questions, with the exception of the third, which has a reverse score, have a direct effect, with higher scores indicating more sleepiness. In the end, the sum of questions scores is obtained, with the score scale ranging from zero to 32 points.
The process of translation and cultural adaptation preserved the assessment of equivalences suggested by Herdman et al.18 and Reichenheim et al.19 The process was carried out according to the following steps: translation, back translation, technical review, assessment of verbal comprehension and clarity of the questionnaire by field experts, assessment of the tool clarity with a focus group, test–retest, and finally, the application of the completed tool.
Initially, three experienced researchers who are fluent in English translated the original tool from English into Brazilian Portuguese. The researchers discussed the discrepancies in the translations and defined a Brazilian Portuguese version, which was then back translated by a native English-speaking expert.
Subsequently, the technical review was performed by the same researchers who carried out the tool translation, in which the English version was compared to the original questionnaire. After the translation accuracy was verified, the questionnaire was sent to five specialists, researchers specialized in the areas of sleep and pediatrics, who assessed the tool items regarding verbal comprehension, clarity of questions, and adequacy to the population aged 11–15 years.
Next, a focus group consisting of ten children and adolescents of both genders, aged 10–17 years, was used to assess the clarity and understanding of the questions, thus defining the final Portuguese version of the PDSS.
For the internal consistency analysis conducted through Cronbach's Alpha, the tool was applied in 90 children and adolescents of both genders (51 girls) enrolled in the final years of elementary school (59.3%) and high school (40.7%), aged 10–17 years, with a mean of 15.7 years. Alpha values ≥0.7 were considered acceptable.20,21 This same group was asked, through a questionnaire, about their sleeping and waking schedule. Based on the information about the sleeping and waking time, the time in bed was calculated. The scale reproducibility was analyzed based on the tool's application in a subgroup of 30 children and adolescents who answered the scale again one week after the first application.
The participating children and adolescents were selected from two private schools, one in Florianópolis, state of Santa Catarina, and another in Curitiba, state of Paraná. After requesting permission to conduct the study in the abovementioned schools, the educational coordinators indicated the classes that were available to answer the questionnaire. Thus, invitations were sent to the students of the selected classes to obtain authorization from their parents or guardians to participate in the study. The project was approved by the Ethics Committee on Human Research of the institution; parents or guardians signed the informed consent and the students signed the term of consent.
The mean and standard deviation of the sum of the scale questions were calculated. The Wilcoxon test was used for the analysis of the test–retest difference. Spearman's correlation test was used for the analysis of correlation between the PDSS scores and time in bed. A 5% level of significance was considered for the inferential tests. Analyses were performed using SPSS version 20.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, version 20.0; NY, USA).
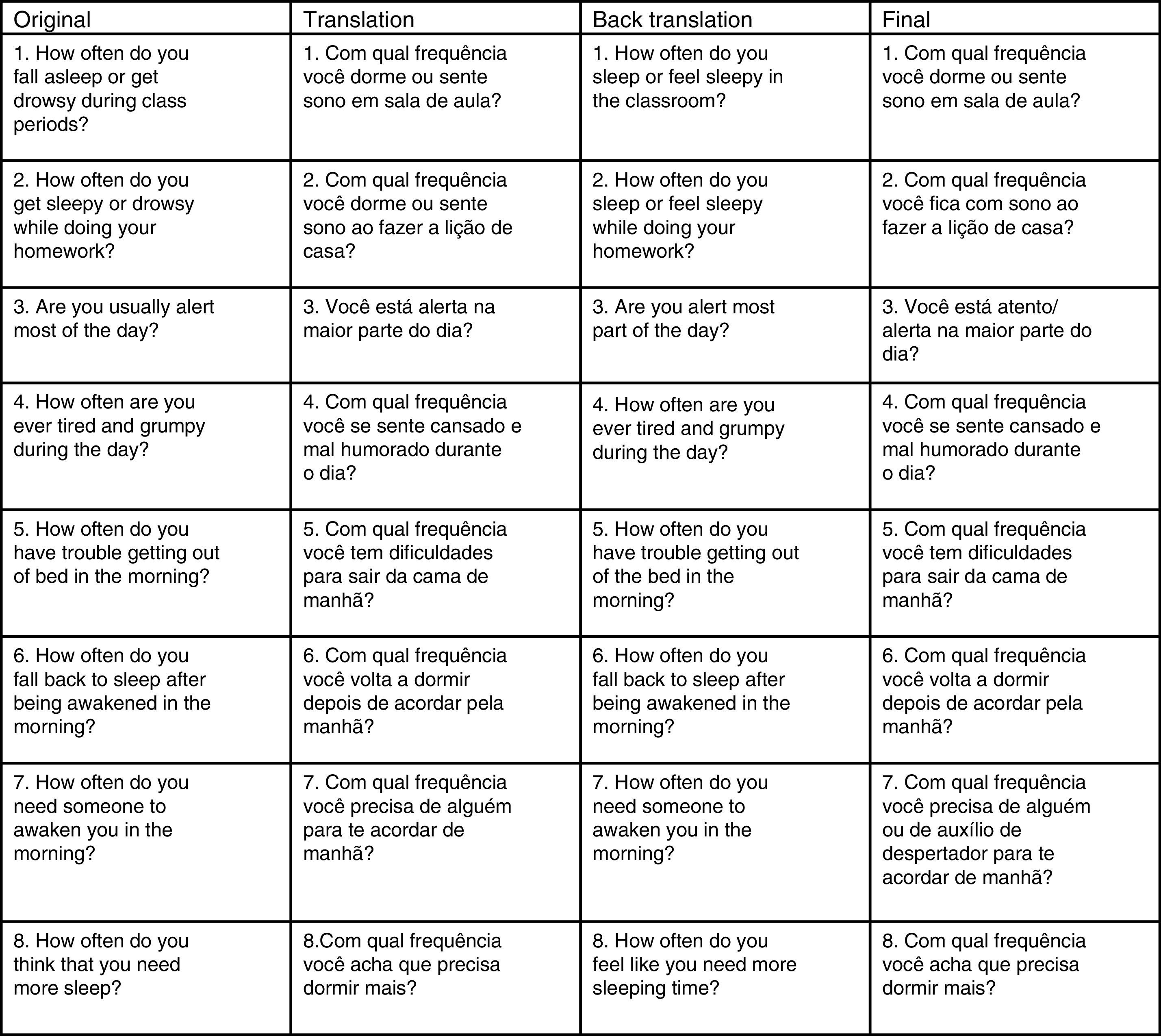
ResultsTranslation and cultural adaptationFig. 1 shows the translation and back-translation analysis of the PDSS questions (Appendix A). The questions showed clarity in the comparison between translation and back translation; the proposed final version of the questions was contextually similar to the original one regarding the language expressions. However, an adaptation was carried out in question seven for better understanding, based on the advice of the area specialist and the focus group.
Expert evaluationThe experts were asked about the clarity and linguistic appropriateness considering the understanding of children and adolescents in the age range of the original tool. Based on this assessment, the word “atento” (aware) was added to the word “alerta” (alert) in question three, due to a better understanding by children and adolescents. In addition, in this assessment, an expert suggested adapting question seven: “How often do you need someone to wake you up in the morning?” The expert suggested considering other ways of awakening, such as an alarm clock. The suggestion was considered valid and adapted in the final version of the scale.
Furthermore, in the final version of the scale, question two was adjusted considering the terms “sleepy” and “drowsy.” These terms were considered synonyms in the Portuguese language, and it is believed that the redundancy used in the English language is not necessary for the appropriate understanding of the question in Portuguese. Thus, the final question was “How often do you feel sleepy while doing your homework?”
Finally, the experts were asked: “According to your perception, does the translated tool constitute a valid indicator in Portuguese and Brazilian culture for the investigation of excessive daytime sleepiness in children and adolescents?” In this evaluation, only one expert said “in part,” as he questioned the lack of work-related questions, considering that, in adolescence, some people are already working. Because of the original scale, it was decided not to make changes considering work activities. Finally, all experts answered “yes” to the following question: “According to your point of view, is the scoring scale in Brazilian Portuguese appropriate?”
Focus groupThe focus group was carried out with ten children and adolescents to verify the understanding of the questions. This group was selected considering the indication of the educational coordination of one of the schools participating in the study, accounting for the availability of students to participate in this activity. The questions were read one by one to the group, and the children/adolescents were asked to explain their understanding. In this stage, the clarity of the questions was verified; no participants had doubts about the content of the questions.
Questionnaire applicationA group of children and adolescents answered all the scale questions with the objective to analyze the internal consistency. A subgroup answered the scale again one week after the first application. The internal consistency and reproducibility results are shown in Table 1. Furthermore, the correlation between the PDSS scores with the time in bed was calculated, and a significant negative correlation was found (r=−0.214; p=0.023).
DiscussionClinical manifestations of EDS in children and adolescents are variable, more evident in sedentary activities such as reading, watching television, and riding a car, and may differ from those observed in adults. While the adult is more likely to have generalized fatigue complaints, younger individuals, especially pre-adolescents, may show inattention, hyperactivity, and behavioral problems.1
The consequences of EDS go beyond clinical symptoms and emerge in several dimensions of life, such as school performance, as shown by the study of Perez-Chada et al.7 in 2884 Argentinean students with a mean age of 13.3 years. The Argentinean study found that EDS measured by PDSS was an independent predictor for poor academic performance in the disciplines of languages and mathematics.
Sleep disorders are increasing in modern society and constitute the main cause of EDS.1,22,23 Thus, there was a significant correlation between the time in bed and EDS in children and adolescents investigated in the validation of PDSS in Brazilian Portuguese. This result confirms that reported by Drake et al.,3 who found that shorter sleep duration was correlated with increased EDS.
In order to analyze the EDS in pediatric populations, the literature indicates some direct tools, such as Multiple Latency Test, and indirect ones, such as the PDSS. Considering that the use of laboratory tests is restricted to a few laboratories, the PDSS is indicated in the clinical practice for the diagnosis and identification of treatment effects, as well as in scientific studies, particularly those with large populations.
The scale content includes questions such as the sensation of feeling sleepy in class and during school tasks, questions about the daily irritability, difficulty getting out of bed, the need to sleep longer, and using an alarm clock or help to wake up. Therefore, although the scale has a summed score, it is possible to analyze the answers to specific questions. Also, it is important to emphasize that the clinical research and EDS research must take into account other factors, such as the sleep/wake cycle pattern, time of use of electronic media,6 and the dietary pattern.24
The PDSS showed satisfactory reliability results (Cronbach's alpha=0.784). Generally, it is affirmed that a value of 0.7–0.8 is acceptable for the analysis, and it is considered that the number of questions influences the statistical calculation, because the numerator of the equation for α depends on the number of scale items.21 Internal consistency values were similar to that observed by Drake et al.3 (Cronbach's alpha=0.81) when validating the American scale. Also, in a similar study carried out with the Epworth Sleepiness Scale, the internal consistency analysis showed a Cronbach's alpha of 0.76 for the validation of Brazilian scale and 0.79 for the validation of the original scale.25
The mean of the sum of the PDSS questions (15.6 points) was similar to that found by Drake et al.3 (15.3 points) and Perez-Chada et al.7 (15.7 points). However, Perez-lloret et al.17 found, in a study of 1194 13–17 year-olds of low socioeconomic level, a slightly lower mean PDSS score (13.8 points). Additionally, Perez-lloret et al.17 identified an association of EDS with low sleep duration, reduced attention, and poor cognitive performance. Thus, considering the mean scores observed in the aforementioned studies, as well as the amplitude of the score scale (0–32 points), it is believed that it is sensitive to assess EDS, as it does not have a “ceiling effect” and/or “floor effect” in the sum of questions.
It is also observed that in the aforementioned studies that used the PDSS, including its validation study, cutoff points for the classification of different levels of EDS were not proposed as in Epworth scale, considering that the greater the score, the higher the indication of daytime sleepiness. In this sense, the authors suggest carrying out further studies for the proposed cutoff points for the sum of the scale.
Another key point refers to the recommended age range for the application of PDSS. The age range of children and adolescents in the original validation study by Drake et al.,3 11–15 years old, was expanded in this study to meet the assessment needs and due to the scarcity of tools to assess EDS in Brazilian children and adolescents. Moreover, literature reports that EDS increases during adolescence due to biological and environmental factors.8,9 Thus, it is considered that the application of PDSS in children younger than the age of the original scale validation (11 years) must ensure the proper understanding of the questions, while for older ages (14 years), it is necessary to consider the appropriateness of the scale regarding the sample profile or patient to be investigated.
A possible limitation of this study is the fact that the sample was obtained exclusively from private schools. However, considering that the PDSS questions are easy to understand and directly related to the daily lives of children and adolescents, such a tool will be well understood by young individuals from other school networks. Additionally, the correlation between PDSS scores with time in bed verified through the questionnaire may limit the analysis sensitivity.
In view of the present analysis, PDSS can be considered as valid for application in samples of Brazilian children and adolescents, by showing appropriate indicators of validity, reproducibility, and internal consistency.
Conflicts of interestThe authors declare no conflicts of interest.
| 1. Com qual frequência você dorme ou sente sono em sala de aula? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 2. Com qual frequência você fica com sono ao fazer a lição de casa? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 3. Você está atento/alerta na maior parte do dia?a |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 4. Com qual frequência você se sente cansado e mal humorado durante o dia? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 5. Com qual frequência você tem dificuldades para sair da cama de manhã? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 6. Com qual frequência você volta a dormir depois de acordar pela manhã? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 7. Com qual frequência você precisa de alguém ou de auxílio de despertador para te acordar de manhã? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| 8. Com que frequência você acha que precisa dormir mais? |
| () Sempre () Frequentemente () Às vezes () Quase nunca () Nunca |
| Pontuação: |
| Sempre=4 |
| Frequentemente=3 |
| Às vezes=2 |
| Quase nunca=1 |
| Nunca=0 |
Please cite this article as: Felden ÉP, Carniel JD, Andrade RD, Pelegrini A, Anacleto TS, Louzada FM. Translation and validation of the Pediatric Daytime Sleepiness Scale (PDSS) into Brazilian Portuguese. J Pediatr (Rio J). 2016;92:168–73.