children with ventricular septal defects (VSD) can have chronic volume overload, which can result in changes of left heart echocardiographic parameters. To evaluate the changes before and after surgical closure, the children were divided into three groups according to the degree of mitral regurgitation (MR), and their echocardiographic characteristics were reviewed at serial follow-up after surgical closure.
Methodsthe preoperative, and one-, three-, and 12-month postoperative echocardiographic data of 40 children who underwent surgical closure of VSD were retrospectively reviewed. Left ventricular end-diastolic volume (LVEDV), left ventricular end-diastolic dimension (LVEDD), left ventricular end-systolic dimension (LVESD), mitral valvular characteristics, including degree of MR and mitral valve annulus, and left atrial (LA) characteristics, including volume and dimensions, were observed.
Resultspreoperative LVEDV, LVEDD, LVESD, mitral valvular annulus, LA volume, and LA dimensions were significantly larger in children with MR. Additionally, there were significant decreases in LVEDV, LVEDD, LA volume, and LA dimensions at one, three, and 12 months postoperatively. The degree of MR also improved to a lower grade after surgical closure of the VSD without additional mitral valve repair.
Conclusionthe echocardiographic parameters of left heart dilation and MR in children with VSD improved within the first year after surgical closure without additional mitral valve repair. Furthermore, in all of the patients with VSD, regardless of MR, LA dilation was reduced within three months after surgical closure of the VSD; however, LV and mitral valve annular dilatation decreased within 12 months.
crianças com defeito do septo ventricular (DSV) podem apresentar sobrecarga de volume crônica, que pode resultar em mudanças nos parâmetros ecocardiográficos do coração esquerdo. Para avaliar as mudanças antes e depois do fechamento cirúrgico, as crianças foram divididas em 3 grupos segundo o grau de regurgitação mitral (RM) e suas características ecocardiográficas foram analisadas com acompanhamento em série após o fechamento cirúrgico.
Métodorevisamos retrospectivamente os dados ecocardiográficos de 40 crianças submetidas a fechamento cirúrgico de DSV antes da cirurgia e nos meses 1, 3 e 12 após a cirurgia. Observamos o volume diastólico final do ventrículo esquerdo (VDFVE), dimensão diastólica final do ventrículo esquerdo (DDFVE) e dimensão sistólica final do ventrículo esquerdo (DSFVE), características da válvula mitral, incluindo grau de RM e o anel da válvula mitral, e características do átrio esquerdo (AE), incluindo volume e dimensões.
Resultadosos resultados para VDFVE, DDFVE, DSFVE, anel da válvula mitral, volume do AE e dimensões do AE foram significativamente maiores em crianças com RM. Além disso, não houve redução significativa no VDFVE, DDFVE, volume do AE e nas dimensões do AE nos meses 1, 3 e 12 após a cirurgia. O grau de RM também apresentou melhoria para um grau menor após o fechamento cirúrgico do DSV sem reparo adicional da válvula mitral.
Conclusãoos parâmetros ecocardiográficos de dilatação do coração esquerdo e a RM em crianças com DSV haviam apresentado melhora no primeiro ano após o fechamento cirúrgico sem reparo adicional da válvula mitral. Além disso, em todos os pacientes com DSV, independentemente de RM, a dilatação do AE reduziu em três meses após o fechamento cirúrgico do DSV; contudo, a dilatação do VE e do anel da válvula mitral reduziu em 12 meses.
It is known that left-to-right shunting in ventricular septal defects (VSD) generally increases pulmonary arterial blood flow and pulmonary venous return to the left heart. This pathophysiologic sequela may result in volume overload of the left atrium (LA) and left ventricle (LV), and subsequent LV enlargement, mitral annular dilation, mitral regurgitation (MR), and consequent LA enlargement to allow for the homeostatic balance of LA pressure.1–3 In the natural course of these changes after surgical closure, it has been demonstrated that the left ventricular end-diastolic volume (LVEDV) returns to normal within the first 2 years of life. However, the left atrial volume (LAV) remains elevated.4 The natural course of MR in children with VSD has also been studied, and it is believed that MR in children with a normal mitral valve (MV) apparatus and hemodynamically large VSD resolves spontaneously after the surgical closure of VSD.5 However, limited information is available on the relationship between MR and left heart volume overload.
The hypothesis of the present study was that a higher degree of MR is associated with more severe left heart dilation, and that the reversibility of the myocardium damage might take a longer period with a more severe degree of left heart dilation. Thus, this study aimed to investigate the timing in resolution of left heart dilation according to the degree of MR in children who underwent surgical closure of VSD.
Materials and methodsSubject characteristicsThe institutional review board approval for a retrospective data review was obtained (CNUH-12-192). The echocardiographic data of 40 patients under 15 years of age who had undergone surgical closure of isolated VSD by a single cardiac surgeon between January of 2009 and November of 2011 were retrospectively reviewed. Patients with small atrial septal defects (ASD) or patent foramen ovale (PFO) were included. However, patients with other associated congenital heart defects, MV abnormalities, ventricular dysfunction, and systemic diseases, including chromosomal anomalies, were excluded. The patients with VSD were divided into three groups according to the degree of preoperative MR, which is the degree of left heart dilation: no MR (no MR group), trivial to mild MR (mild MR group), and moderate to severe MR (moderate to severe MR group). Left heart echocardiographic characteristics of the patients in three groups at serial follow-up after surgical closure of VSD were retrospectively reviewed.
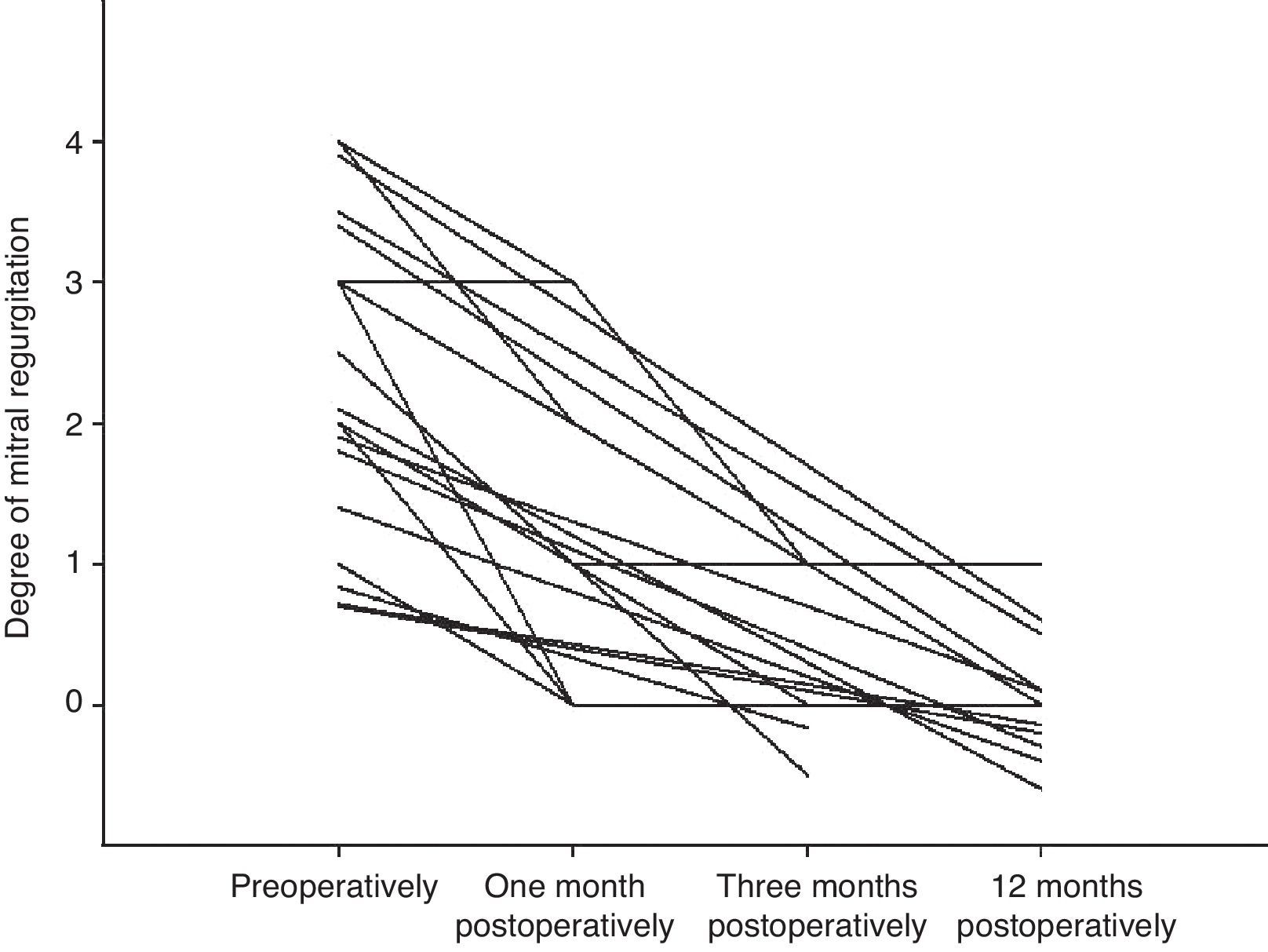
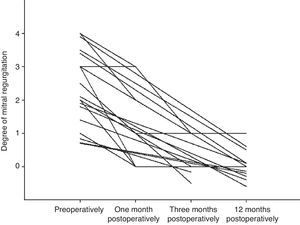
Assessment of MR and left heart echocardiographic changesMR was classified as none, trivial, mild, moderate, or severe based on qualitative color flow mapping. The changes in the degree of MR preoperatively and at one, three, and 12 months postoperatively in those who had MR before the surgical closure of VSD were also reviewed.
The following parameters through echocardiography at approximately one month preoperatively were reviewed: type of VSD, sizes and peak Doppler gradients of the VSD, and degree of MR. Body weight, height, body surface area (BSA), and postoperative survival were also examined. At all times, including approximately one month preoperatively and at one, three, and 12 months postoperatively, the following parameters were evaluated in echocardiography: LV characteristics, including the LV end-diastolic dimension (LVEDD), LV end-systolic dimension (LVESD), and LV end-diastolic volume (LVEDV), MV annulus, LA end-systolic dimensions, and LA end-systolic volume (LA volume). The changes in echocardiographic parameters over serial follow-up times were then evaluated and compared among the three groups. LVEDD and LVESD were obtained by M-mode echocardiography, and they were converted to Z-scores. The LVEDD Z-score (LVEDD-Z) and LVESD Z-score (LVESD-Z) were calculated as the number of standard deviations from the mean value of the normal population relative to the BSA. The LVEDV was indexed to the BSA and defined as the LVEDV index. The mitral valve annulus was measured from the apical four-chamber view at mid-diastole, and the data were converted to Z-scores for inter-individual comparisons. The dimensions of three planes of linear LA were also measured: the parasternal long axis (PLAX), lateral (LAT), and superoinferior (SI).6 The LA volume was measured following recommendations for chamber quantification7 by the following equation: LA volume=4π/3×(PLAX/2)×(LAT/2)×(SI/2). All linear LA dimensions and LA volume to the BSA were indexed and defined as the PLAX index, LAT index, SI index, and LAV index.
Statistical analysesThe chi-squared test and one-way analysis of variance (ANOVA) with Tukey's post-hoc analysis were used to test for differences in subject characteristics among the three groups of MR. Two-way repeated measures ANOVA with Tukey's post-hoc analysis was used to compare the left heart echocardiographic parameters among three groups of MR according to the time. The Statistical Package for Social Sciences (SPSS) version 20.0 (SPSS Inc. - Chicago, IL, USA) was used for all data analyses.
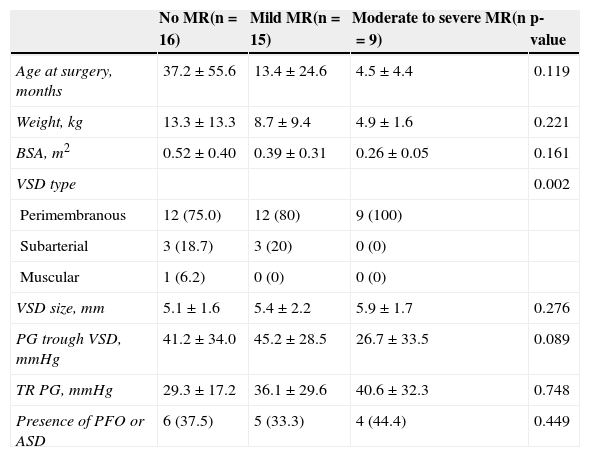
ResultsSubject characteristicsA total of 40 patients with VSD met the inclusion criteria: 16 patients had VSD with no preoperative MR, 15 patients had trivial to mild MR, and nine patients had moderate to severe MR. In the group with no MR, 12 patients (75.0%) had perimembranous VSD, three (18.7%) had subarterial VSD, and one (6.2%) had outlet muscular VSD. In the group with trivial to mild MR, 12 patients (80.0%) had perimembranous VSD and three (20.0%) had subarterial VSD. In the group with moderate to severe MR, all nine patients (100.0%) had perimembranous VSD (p=0.002). There were no statistically significant differences in age, body weight, BSA, pressure gradient through VSD, pressure gradient of tricuspid regurgitation, or the presence of ASD or PFO among the three groups (Table 1). There was no postoperative mortality.
Subject characteristics according to the grade of mitral regurgitation.
| No MR(n=16) | Mild MR(n=15) | Moderate to severe MR(n=9) | p-value | |
|---|---|---|---|---|
| Age at surgery, months | 37.2±55.6 | 13.4±24.6 | 4.5±4.4 | 0.119 |
| Weight, kg | 13.3±13.3 | 8.7±9.4 | 4.9±1.6 | 0.221 |
| BSA, m2 | 0.52±0.40 | 0.39±0.31 | 0.26±0.05 | 0.161 |
| VSD type | 0.002 | |||
| Perimembranous | 12 (75.0) | 12 (80) | 9 (100) | |
| Subarterial | 3 (18.7) | 3 (20) | 0 (0) | |
| Muscular | 1 (6.2) | 0 (0) | 0 (0) | |
| VSD size, mm | 5.1±1.6 | 5.4±2.2 | 5.9±1.7 | 0.276 |
| PG trough VSD, mmHg | 41.2±34.0 | 45.2±28.5 | 26.7±33.5 | 0.089 |
| TR PG, mmHg | 29.3±17.2 | 36.1±29.6 | 40.6±32.3 | 0.748 |
| Presence of PFO or ASD | 6 (37.5) | 5 (33.3) | 4 (44.4) | 0.449 |
ASD, atrial septal defects; BSA, body surface area; MR, mitral regurgitation; PG, pressure gradient; PFO, patent foramen ovale; TR, tricuspid regurgitation; VSD, ventricular septal defect.
All data are presented as mean±standard deviation or n (%).
Patients who did not have MR preoperatively did not progress to new-onset MR after surgical closure of the VSD. All patients improved regarding the degree of MR. In the mild MR group (n=15), 11 patients had trivial MR and four had mild MR preoperatively; at one month postoperatively (n=15), 12 patients were resolved and three patients improved to a trivial degree of MR; at three months postoperatively (n=12), 11 patients were resolved and one patient remained with trivial MR until 12 months after surgery. In the moderate to severe MR group (n=9), six patients had moderate MR and three had severe MR preoperatively; at one month postoperatively (n=9), MR had resolved in three patients, improved to trivial in three patients, decreased to moderate in two patients, and one patient remained with moderate MR. At three months (n = 7), four patients improved to trivial and three patients remained without MR. At 12 months, follow-up data were available for six patients; among them, MR remained trivial in two patients (Fig. 1).
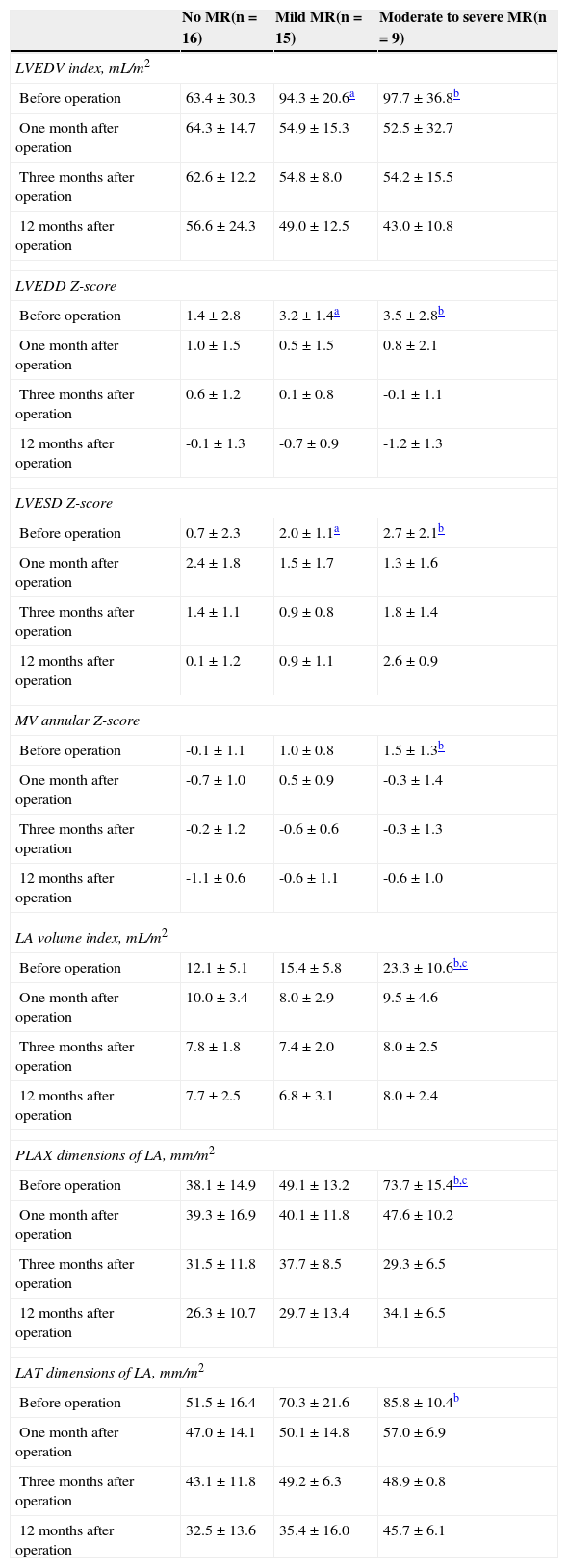
Left heart echocardiographic characteristicsThe echocardiographic values of LV, MV annulus, and LA enlargement are shown in Table 2. The preoperative LVEDV index, LVEDD-Z, and LVESD-Z were significantly greater in the mild MR group (p=0.034, p=0.034, and p=0.039, respectively) and moderate to severe MR group (p=0.036, p=0.035, and p=0.020, respectively) than in the no MR group.
Left heart echocardiographic parameters before and at one, three, and 12 months after surgical closure of ventricular septal defect, according to the degree of mitral regurgitation.
| No MR(n=16) | Mild MR(n=15) | Moderate to severe MR(n=9) | |
|---|---|---|---|
| LVEDV index, mL/m2 | |||
| Before operation | 63.4±30.3 | 94.3±20.6a | 97.7±36.8b |
| One month after operation | 64.3±14.7 | 54.9±15.3 | 52.5±32.7 |
| Three months after operation | 62.6±12.2 | 54.8±8.0 | 54.2±15.5 |
| 12 months after operation | 56.6±24.3 | 49.0±12.5 | 43.0±10.8 |
| LVEDD Z-score | |||
| Before operation | 1.4±2.8 | 3.2±1.4a | 3.5±2.8b |
| One month after operation | 1.0±1.5 | 0.5±1.5 | 0.8±2.1 |
| Three months after operation | 0.6±1.2 | 0.1±0.8 | -0.1±1.1 |
| 12 months after operation | -0.1±1.3 | -0.7±0.9 | -1.2±1.3 |
| LVESD Z-score | |||
| Before operation | 0.7±2.3 | 2.0±1.1a | 2.7±2.1b |
| One month after operation | 2.4±1.8 | 1.5±1.7 | 1.3±1.6 |
| Three months after operation | 1.4±1.1 | 0.9±0.8 | 1.8±1.4 |
| 12 months after operation | 0.1±1.2 | 0.9±1.1 | 2.6±0.9 |
| MV annular Z-score | |||
| Before operation | -0.1±1.1 | 1.0±0.8 | 1.5±1.3b |
| One month after operation | -0.7±1.0 | 0.5±0.9 | -0.3±1.4 |
| Three months after operation | -0.2±1.2 | -0.6±0.6 | -0.3±1.3 |
| 12 months after operation | -1.1±0.6 | -0.6±1.1 | -0.6±1.0 |
| LA volume index, mL/m2 | |||
| Before operation | 12.1±5.1 | 15.4±5.8 | 23.3±10.6b,c |
| One month after operation | 10.0±3.4 | 8.0±2.9 | 9.5±4.6 |
| Three months after operation | 7.8±1.8 | 7.4±2.0 | 8.0±2.5 |
| 12 months after operation | 7.7±2.5 | 6.8±3.1 | 8.0±2.4 |
| PLAX dimensions of LA, mm/m2 | |||
| Before operation | 38.1±14.9 | 49.1±13.2 | 73.7±15.4b,c |
| One month after operation | 39.3±16.9 | 40.1±11.8 | 47.6±10.2 |
| Three months after operation | 31.5±11.8 | 37.7±8.5 | 29.3±6.5 |
| 12 months after operation | 26.3±10.7 | 29.7±13.4 | 34.1±6.5 |
| LAT dimensions of LA, mm/m2 | |||
| Before operation | 51.5±16.4 | 70.3±21.6 | 85.8±10.4b |
| One month after operation | 47.0±14.1 | 50.1±14.8 | 57.0±6.9 |
| Three months after operation | 43.1±11.8 | 49.2±6.3 | 48.9±0.8 |
| 12 months after operation | 32.5±13.6 | 35.4±16.0 | 45.7±6.1 |
LA, left atrium; LAT, lateral; LVEDD, left ventricular end-diastolic dimension; LVEDV, left ventricular end-diastolic volume; LVESD, left ventricular end-systolic dimension; MR, mitral regurgitation; MV, mitral valve; PLAX, parasternal long axis; SI, superior-inferior.
All data are presented as mean±standard deviation.
The preoperative MV annular Z-score in the moderate to severe MR group was significantly larger than that in the no MR group (p=0.038).
There was a significant difference in the LA volume index and PLAX index of the moderate to severe MR group compared with that of the no MR group (p=0.008, p=0.001, respectively) and mild MR group (p=0.047, p=0.006, respectively) preoperatively.
The preoperative LAT index in the moderate to severe MR group was significantly higher than that in the no MR group (p=0.001). There was no significant difference in the echocardiographic values of LV, MV annulus, and LA parameters among the groups at any subsequent time.
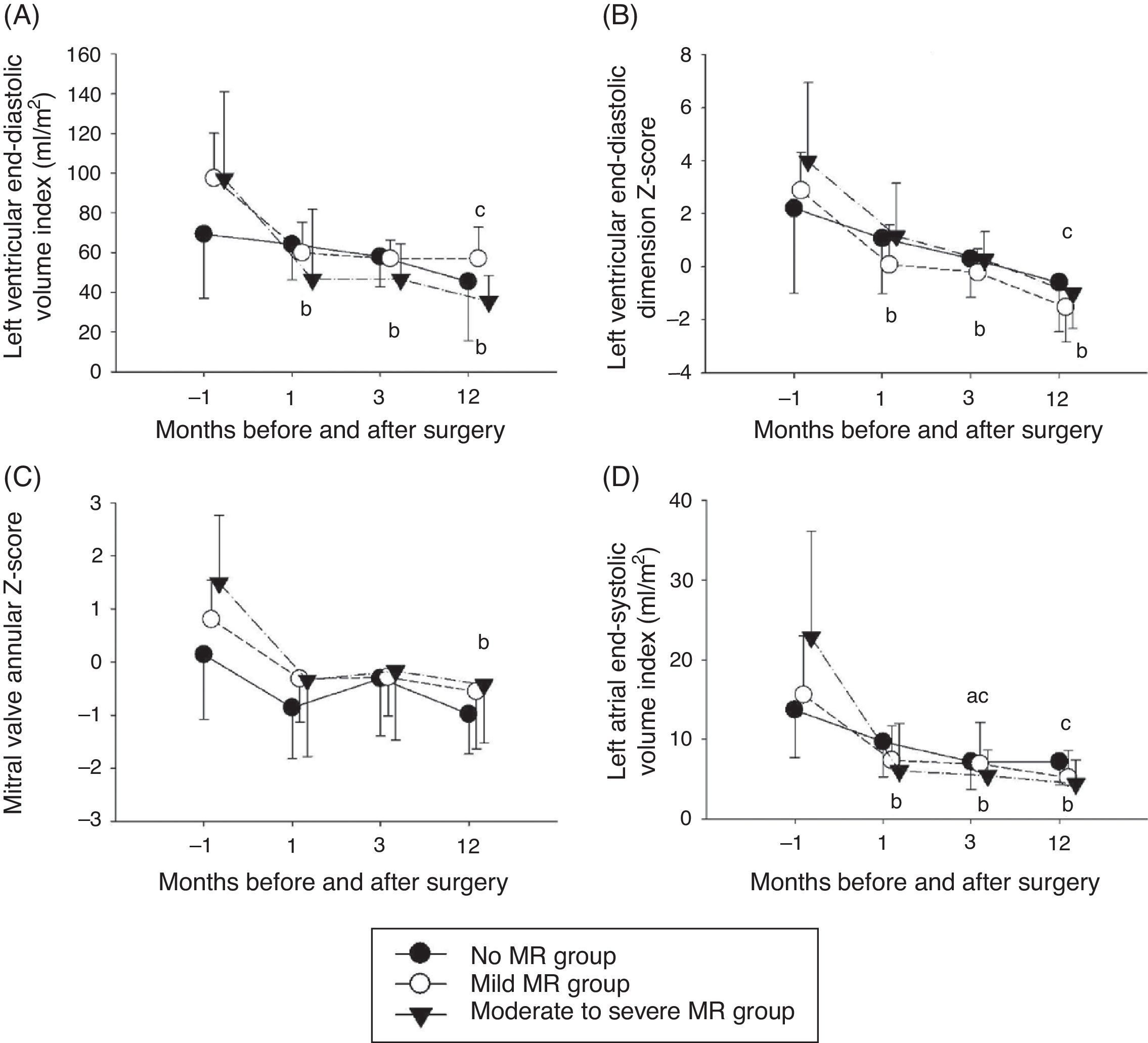
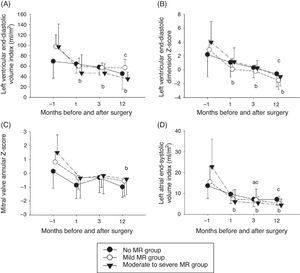
Serial changes in postoperative left heart echocardiographic parametersNo groups showed any significant decrease in the LVEDV index, LVEDD-Z, LVESD-Z, and MV annulus Z-score at any time following closure of the VSD. The mild MR group demonstrated a significant reduction in the LVEDV index and LVEDD-Z at one month (p<0.001, p<0.001, respectively), three months (p=0.004, p<0.001, respectively), and 12 months postoperatively (p=0.002, p<0.001, respectively) when compared with one month preoperatively. The moderate to severe MR group demonstrated a significant reduction in the LVEDV index and LVESD-Z only at 12 months postoperatively (p=0.035, p=0.003, respectively) compared with one month preoperatively. There were significant reductions in LVEDD-Z at three months and 12 months postoperatively (p=0.043, p=0.027, respectively). There were no significant intergroup differences (Fig. 2A, B).
Changes in echocardiographic data in the three groups according to time: before the operation, and at one, three, and 12 months after ventricular septal defect operation (expressed as -1, 1, 3, and 12, respectively). A, left ventricular end-diastolic volume index (mL/m2). B, left ventricular end-diastolic dimension Z-score. C, mitral valve annular Z-score. D, left atrial volume index (mL/m2). a p<0.05 vs. one month preoperatively in the group with no mitral regurgitation (MR). b p<0.05 vs. one month preoperatively in the group with trivial to mild MR. c p<0.05 vs. one month preoperatively in the group with moderate to severe MR.
The mild MR group demonstrated a significant reduction in the MV annular Z-score 12 months postoperatively (p=0.028) when compared with one month preoperatively. There were no significant intergroup differences (Fig. 2C).
The no MR group showed a significant decrease in the LA volume index only at three months (p=0.023) following closure of the VSD. The mild MR group demonstrated a significant reduction in the LA volume index at one month (p=0.011), three months (p=0.020), and 12 months (p=0.006) postoperatively when compared with one month preoperatively. The moderate to severe MR group demonstrated a significant decrease at three months (p=0.021) and 12 months (p=0.015). There was also a significant intergroup difference between the no MR group and the moderate to severe MR group (p=0.011), and between the mild MR group and the moderate to severe MR group (p=0.027) (Fig. 2D).
The no MR group showed a significant decrease in the PLAX index at one month (p=0.023) and three months (p=0.014) postoperatively. The mild MR group demonstrated a significant reduction in the PLAX index at three months (p=0.030), six months (p<0.001), and 12 months (p<0.001) postoperatively when compared with one month preoperatively. The moderate to severe MR group also showed a significant decrease at one month (p=0.034), three months (p=0.006), and 12 months (p=0.002). There was also a significant intergroup difference between the no MR and moderate to severe MR groups (p=0.019)
The no MR group showed a significant decrease in the LAT index at three months (p=0.041) and 12 months (p=0.005) following closure of the VSD. The mild MR and the moderate to severe MR groups demonstrated a significant reduction in the LAT index at one month (p<0.001, p=0.002, respectively), three months (p=0.003, p<0.001, respectively), and 12 months (p<0.001, p<0.001, respectively) postoperatively when compared with one month preoperatively. There was also a significant intergroup difference between the groups with no MR and with moderate to severe MR (p=0.028).
All groups demonstrated a significant reduction in the SI index at one month (p=0.05, p=0.028, and p=0.014), three months (p=0.029, p=0.049, and p≤0.001), and 12 months (p=0.014, p=0.004, and p≤0.001) postoperatively when compared with one month preoperatively. There were no significant intergroup differences.
DiscussionIn the present study, the LV, MV annulus, and LA dilation were evaluated by measuring the LVEDV, LVEDD, MV annulus, LA dimensions, and LA volume. It was observed that all of the echocardiographic parameters associated with left heart dilation decreased regardless of MR within one year.
LV dilationPapadimitriou et al.8 reported on structural reversibility by creating aortocaval shunts in dogs. They examined the LV volume, LV mass, and histological changes at the time in which congestive heart failure developed, and they also evaluated two other groups at two and six months after the created shunt had been closed. According to their results, the volume overload in the left chamber led to structural changes at the myocyte level that were reversible after the shunt burden was removed. Another clinical study concerning the reversibility of left ventricular dilation demonstrated that children with moderately large VSD and LV volume overloads without pulmonary hypertension or congestive heart failure experienced a spontaneous decrease of LV dilation.8 In the present study, with a chronic left to right shunt, LVEDV, LVEDD, and LVESD were significantly greater in patients with MR compared to those without MR. After removal of the shunt burden, there were no statistical differences among the three groups at any of the serial follow-up times. In addition, the LVEDV and LVEDD decreased significantly after surgical closure at all of the follow-up times in children with VSD and trivial to mild MR.
MV annular dilation and MRMV annular dilation is considered to be a physiologic sequela to volume overload to the left heart, and MR develops secondary to annular dilation.9 Hisatomi et al.10 reported cases of children with VSD who underwent MV repair, and concluded that if MR develops secondary to annular dilation, there is no need for MV repair. In contrast, Honjo et al.11 have also reported on 17 children who underwent MV repair, among whom were five patients with VSD, two with ASD, two with left ventricular diverticulum, one with partial anomalous pulmonary venous return, and one with coarctation of the aorta and VSD. They concluded that MV repair is feasible and presents a low reoperation rate. However, Mahadin et al.5 stated that a more aggressive approach to MV repair would do harm to growing children if the natural course of MR was not fully recognized. They suggested that MR with a normal mitral valve apparatus improves after surgical closure of VSD, and that MV repair should be taken under careful consideration. In this study, the MV annular Z-scores were measured and compared according to the degree of MR. The MV annulus was significantly larger in children with moderate to severe MR compared to those without MR. In addition, the MV annulus was found to decrease significantly after surgical closure in those with trivial to mild MR within one year. The present findings support the fact that children with VSD experience restoration to their normal valvular competency and the coaptation zone after surgical closure of VSD without MV repair.5 It was also observed that MR was reversible after surgical closure of VSD, and this happened mostly within the first year after surgery. In particular, the degree of MR decreased within one month of surgical closure. Based on these findings, an aggressive approach to MV repair in children with VSD is not necessary, considering the natural course of MR.
LA dilationThere were limited data regarding the significance of LA volume. The LA volume is also important because it can contribute to LV diastolic filling.12 Sakata et al.13 have recently developed an LA volume-tracking method, and highlighted the importance of measuring LA volume in patients with chronic LV volume overload. Cordell et al.4 have measured LVEDV and maximal LA volume by catheterization, and demonstrated that LVEDV returned to normal after surgical closure of VSD; however, the maximal LA volume remained elevated. They indicated this as a permanent change in the elasticity of LA. In contrast to that study, in the present study echocardiography was used. The dimensions of LA at the parasternal long axis view and at the apical four-chamber view were measured, the LA volume was calculated using the recommended formula and then indexed to the BSA. The preoperative LA volume indexed to the BSA was significantly larger in children with VSD and moderate to severe MR than in those with a lesser degree of MR. In contrast to other parameters of LV and MV annular dilatation, which did not show a significant decrease in children without MR at any subsequent time postoperatively, the LA volume and dimensions decreased significantly within three months after surgical closure in all degrees of MR, including VSD with no MR. There was no difference in the chamber size at any time after surgery relative to the degree of MR.
The present study had a relatively small number of reviewed patients, especially among those with moderate to severe MR. This is due to the practice adopted in this institution to not wait for surgery if the degree of MR is higher than mild to moderate. In addition, follow-up data were missing for nine of the 40 subjects at three months after surgery, and for seven of 40 subjects at 12 months after surgery. Qualitative methods were used to determine the degree of MR, and misrepresentation of the severity is thus possible.
This study is the first to assess the serial changes in left heart echocardiographic parameters before surgery and at one, three, and 12 months after surgical closure in predicting the natural course in children with surgical closure of VSD. The echocardiographic parameters, including the LVEDD, LVEDV, MV annulus, LA dimensions, and LA volume showed significant differences according to the degree of MR. Also, in all patients with VSD, regardless of MR, LA dilation was reduced within three months after surgical closure of the VSD; however, LV and MV annular dilatation decreased within 12 months, which tended to take more time only in those with MR. Further studies are needed to determine the reason for different times required for the resolution of LV, MV, and LA dilation.
FundingThis study was supported by a grant (CRI 13024-1) from the Chonnam National University Hospital Research Institute of Clinical Medicine.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Cho HJ, Ma JS, Cho YK, Ahn BH, Na KJ, Jeong IS. Timing in resolution of left heart dilation according to the degree of mitral regurgitation in children with ventricular septal defect after surgical closure. J Pediatr (Rio J). 2014;90:71–77.