to validate the Portuguese version of the Children's Sleep Habits Questionnaire (CSHQ-PT) and compare it to the versions from other countries.
Methodsthe questionnaire was previously adapted to the Portuguese language according to international guidelines. 500 questionnaires were delivered to the parents of a Portuguese community sample of children aged 2 to 10 years old. 370 (74%) valid questionnaires were obtained, 55 children met exclusion criteria and 315 entered in the validation study.
Resultsthe CSHQ-PT internal consistency (Cronbach's α) was 0.78 for the total scale and ranged from 0.44 to 0.74 for subscales. The test-retest reliability for subscales (Pearson's correlations, n=58) ranged from 0.59 to 0.85. Our data did not adjust to the original 8 domains structure in Confirmatory Factor Analysis but the Exploratory Factor Analysis extracted 5 factors that have correspondence to CSHQ subscales.
Conclusionthe CSHQ-PT evidenced psychometric properties that are comparable to the versions from other countries and adequate for the screening of sleep disturbances in children from 2 to 10 years old.
validar a versão em português do Questionário de Hábitos de Sono das Crianças (CSHQ-PT) e compará-la às versões de outros países.
Métodoso questionário foi anteriormente adaptado para o português de acordo com as diretrizes internacionais. 500 questionários foram entregues aos pais de uma amostra populacional portuguesa de crianças com idade entre 2 e 10 anos. 370 (74%) questionários válidos foram obtidos, 55 crianças apresentaram critérios de exclusão e 315 foram aceitas no estudo de validação.
Resultadosa consistência interna do CSHQ-PT (α de Cronbach) foi de 0,78 para a escala completa e variou de 0,44 a 0,74 nas subescalas. A confiabilidade teste-reteste das subescalas (correlações de Pearson, n = 58) variou de 0,59 a 0,85. Nossos dados não foram compatíveis com a estrutura original de 8 domínios na Análise Fatorial Confirmatória, porém a Análise Fatorial Exploratória extraiu 5 fatores que correspondem às subescalas do CSHQ.
Conclusãoo CSHQ-PT apresentou propriedades psicométricas comparáveis às versões de outros países e adequadas para triagem de problemas do sono em crianças de 2 a 10 anos de idade.
Adequate sleep is increasingly recognized as an important determinant of child and adolescent health, for inadequate sleep may impact daytime cognitive functions, academic performance, behavior, emotional regulation, weight and the risk of accidental falls.1–5 Its consequences may extend also to the parents sleep quality and daytime functioning. 6
Parents report sleep difficulties in 10-75% of children worldwide, ranging from transient benign behavioral problems to more persistent and severe conditions such as the sleep apnea syndromes.3,7,8 Sleep problems also seem to be common in Portugal and in Brazil, but there is a lack of recent data about the sleep habits of children aged 2 to 6 years old obtained with validated questionnaires.9,10
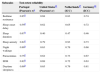
The Children's Sleep Habits Questionnaire (CSHQ) is a retrospective parent-report questionnaire that was developed in the United States to evaluate the sleep behavior in school-aged children.11 The questions were selected in order to include the symptom presentations of the most common pediatric sleep disorders, according to the International Classification of Sleep Disorders. 12 Thirty-three out of its 45 initial items (Fig. 1) were further conceptually grouped into eight subscales, reflecting the following sleep domains: Bedtime Resistance, Sleep Onset Delay, Sleep Duration, Sleep Anxiety, Night Wakings, Parasomnias, Sleep-Disordered Breathing and Daytime Sleepiness. This 33-items structure was validated for the screening sleep disturbances in school-aged children (4 to 10 years old) showing a full scale internal consistency of 0.68 in a community sample, ranging from 0.36 to 0.70 for the subscales. Comparing the results from community and clinic samples, this study suggested a total score cut off of 41 to identify children with potential sleep disorders.12
The CSHQ was subsequently used in several studies, reflecting its usefulness and adequate psychometric properties, and it was also successfully used with children aged 2 to 3 years old.13,14 There are adaptations of the questionnaire to other languages such as Chinese, Hebrew, Dutch, German, Italian and Spanish and, for most of them, there are published validation studies.15–20
The CSHQ was previously adapted to the Portuguese language and culture.21 In this study we aimed to perform its validation and to compare it to the versions from other countries.
MethodsThe CSHQ evaluates the parents’ perception of their child's sleep during the last week or, if it was not representative for some reason, during a recent more typical week. The frequency of sleep related behaviors is rated on a 3-point scale as “usually” (5 to 7 times per week, scored as 3 points), “sometimes” (2 to 4 times per week, scored as 2 points) or “rarely” (0 to 1 time per week, scored as 1 point). The scoring of some items was reversed (items 1, 2, 3, 10, 11 and 26) so that an higher score corresponds to a more disturbed sleep. Full scale (33 items) and subscales scores can be calculated.12 The subscales are Bedtime Resistance (items 1, 3, 4, 5, 6 and 8), Sleep Onset Delay (item 2), Sleep Duration (items 9, 10 and 11), Sleep Anxiety (items 5, 7, 8 and 21), Night Wakings (items 16, 24 and 25), Parasomnias (items 12, 13, 14, 15, 17, 22 and 23), Sleep-Disordered Breathing (items 18, 19 and 20) and Daytime Sleepiness (items 26, 27, 28, 29, 30, 31, 32 and 33).
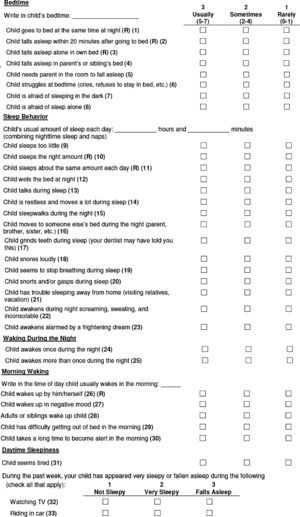
The cultural adaptation of the CSHQ to the Portuguese language (CSHQ-PT) was authorized by the author of the original version in 2009, who also approved the final back translation. This process was developed by a translation team from Portugal, according to recommended guidelines.21,22,23 The questionnaire was translated to the Portuguese language by two independent translators and a single consensus version was obtained; the English back translation was performed by another two translators who had English as their first language, and synthesized in a single version. The translation team, that also included a respiratory medicine pediatrician and a professional translator, reviewed the documents in order to solve the small discrepancies and to get a Portuguese version that was conceptually equivalent to the original and understandable for parents with low literacy level. The final Portuguese version (Fig. 2) was tested in cognitive interviews (n=10 parents, including 3 with Brazilian Portuguese as their first language) showing that it was clear for all of them.
For children under 4 years, the item “Wets bed” did not apply and it was scored as “sometimes” as in a previous study with this age band. 13
The participants were enrolled in schools (N=252) and also in surveillance appointments (n=248), so that younger children would be included. In order to have a more representative sample, both medium-high and low population density regions of Portugal were selected. Parents who volunteered received a second questionnaire for retest analysis after 1-2 weeks (n=138).
The minimum sample size was set as N=231 for an estimated full scale α=0.70 to be determined with a 95% confidence interval of ±0.05.24 This sample size would also be reasonable for factor analysis.25 Allowing for non-responders and children with exclusion criteria, 500 questionnaires were delivered to a convenience sample of parents of children from 2 to 10 years old.
The inclusion criteria were eligible age of the children and the willingness of the parents to participate after informed consent. As in the original validation study, the exclusion criteria were the parent report of a developmental or psychiatric disorder (such as Attention Deficit Hyperactivity Disorder - ADHD, Autism Spectrum Disorder) or medication (psychostimulants, anticonvulsants or antihistamines) that might impact sleep.12
In the absence of a well established socioeconomic status classification in Portugal, the parent educational level was used for this characterization.
The study protocol and the questionnaire were approved by the Ministry of Education and the Ethics Committee. The questionnaires were delivered between October 2010 (pilot study) and February 2011.
The data analysis was made with SPSS 11.0 program, except for Confirmatory Factor Analysis that was performed using LISREL 8.7 software. P values were considered significant if under 0.05. Unpaired t test, Kruskal-Wallis tests and chi-square tests were used to compare means, distributions and proportions between groups as appropriate.
The internal consistency of the 33 scoring items and its subscales was assessed with Cronbach's α coefficients. Test-retest reliability for subscales was evaluated with Pearson's r. The correlations were regarded as weak (0.20-0.39), moderate (0.40-0.59), strong (0.60-0.79) or very strong (0.80-1.00).26
Confirmatory Factor Analysis was performed to test the adjustment of our data to the 8-factor model of the original CSHQ. A Comparative Fit Index (CFI) > 0.95 and a Root Mean Square Error of Approximation (RMSEA) < 0.06 were considered as a good fit.27 As these conditions were not satisfied, we performed also an Exploratory Factor Analysis.
ResultsThree hundred and seventy seven questionnaires were returned and seven were excluded for having more than 20% missing or invalid answers. From 370 (74%) valid questionnaires, fifty five children (15%) met exclusion, 29 for disease (mainly ADHD) and 30 for medication (mainly antihistamines). Likewise, 315 questionnaires entered in the validation study.
The questionnaires were answered by the mothers (81.9%), fathers (12.3%), both (4.8%) or other person (1.0%). The children's mean age was 5.8 ± 2.4 years. Other Socio-demographic characteristics are presented in Table 1.
Socio-demographic characterization of the validation sample (n = 315).
| Variable | n | % |
|---|---|---|
| Child gender | ||
| Male | 149 | 47.3% |
| Female | 166 | 52.7% |
| Child age | ||
| 2 years old | 37 | 11.7% |
| 3 y.o. | 31 | 9.8% |
| 4 y.o. | 43 | 13.7% |
| 5 y.o. | 33 | 10.5% |
| 6 y.o. | 34 | 10.8% |
| 7 y.o. | 45 | 14.3% |
| 8 y.o. | 49 | 15.6% |
| 9 y.o. | 34 | 10.8% |
| 10 y.o. | 9 | 2.9% |
| Parent education | ||
| I. Less than 9 years | 24 | 7.6% |
| II. 9 years | 65 | 20.6% |
| III. 12 years | 96 | 30.5% |
| IV. Bachelor's degree or higher | 118 | 37.5% |
| Missing | 12 | 3.8% |
| Population density zone | ||
| Medium-High (urban ≥100/Km2) | 225 | 72.6% |
| Low (rural, <100/Km2) | 85 | 27.4% |
| Country of residence | ||
| Portugal | 315 | 100% |
The CSHQ-PT total score mean was 47.0 ± 7.2 (95% CI: 46.10-47.81). Comparing the mean total scores from three age subgroups (2 to 4, 5 to 7, and 8 to 10 years), we found a trend for a gradual decrease: 49.4 ± 7.8, 46.2 ± 6.1, 45.11 ± 7.1, respectively (p < 0.001). There were no differences between boys and girls. Children identified by the parents as “Problem sleepers” had a higher mean score then “Non-problem sleepers”: 54.5 versus 45.9, respectively (p < 0.001).
The internal consistency of the CSHQ-PT was 0.78 for the full 33-item scale (95% CI 0.746 - 0.809) and ranged from 0.44 to 0.74 for the subscales (Table 2). Eliminating items 21, 26, 28, 32 and 33 would increase the total scale α to 0.81 but would decrease the subscales α, except for item 21. Eliminating items 7 and 21 would increase Sleep Anxiety α from 0.44 to 0.57.
CSHQ internal consistencies (Cronbach's α) in community samples from different countries.
| Portugal | US12 | China15 | Israel16 | Netherlands17 | Germany18 | |
|---|---|---|---|---|---|---|
| Full scale | 0.78a | 0.68 | 0.80 | 0.81 | NP | 0.68 |
| Subscales: | 0.49-0.72 | |||||
| Bedtime resistance | 0.74a | 0.70 | 0.78 | 0.68 | 0.70 | |
| Sleep duration | 0.68a | 0.69 | 0.68 | 0.63 | 0.70 | |
| Sleep anxiety | 0.44a | 0.63 | 0.65 | 0.54 | 0.55 | |
| Night wakings | 0.58a | 0.54 | 0.49 | 0.62 | 0.49 | |
| Parasomnias | 0.57a | 0.36 | 0.28 | 0.54 | 0.36 | |
| Sleep-disordered breathing | 0.67a | 0.51 | 0.46 | 0.47 | 0.23 | |
| Daytime sleepiness | 0.71a | 0.65 | 0.67 | 0.67 | 0.63 | |
| Study sample size | 315 | 469 | 517 | 98 | 1145 | 298 |
CSHQ, Children's Sleep Habits Questionnaire; NP, not published.
The answers for children aged 2 to 3 years old (n = 68) showed internal consistencies that were similar to the older ones: total scale 0.78, Bedtime Resistance 0.74, Sleep Duration 0.72, Sleep Anxiety 0.53, Night Wakings 0.58, Parasomnias 0.57, Sleep-Disordered Breathing 0.74 and Daytime Sleepiness 0.64.
Retest questionnaires were sent to 138 parents with a 57.2% response rate. Twenty one questionnaires presented exclusion criteria and 58 were used in test-retest reliability analysis. The total CSHQ score showed a strong correlation in retests (0.79, p < 0.001). Subscale score correlations ranged from 0.59 to 0.85 (Table 3). The sleep schedules (bedtime and wake time in weekdays and weekends) showed very strong correlations (from 0.86 to 0.96) except for the bedtime in the weekend (0.64, p < 0.001). The child's usual amount of sleep each day also showed a strong correlation in retests (r=0.79, p < 0.001).
CSHQ test-retest reliability in community samples from different countries.
| Subscales | Test-retest reliability | |||
|---|---|---|---|---|
| Portugal (Pearson's r)a | United States12 (Pearson's r) | Netherlands17 (ICC) | Germany18 (ICC) | |
| Bedtime resistance | 0.85b | 0.68 | 0.83 | 0.74 |
| Sleep onset delay | 0.59b | 0.62 | 0.65 | 0.72 |
| Sleep duration | 0.67b | 0.40 | 0.47 | 0.46 |
| Sleep anxiety | 0.82b | 0.79 | 0.93 | 0.73 |
| Night wakings | 0.80b | 0.63 | 0.79 | 0.68 |
| Parasomnias | 0.79b | 0.62 | 0.73 | 0.67 |
| SDB | 0.82b | 0.69 | 0.72 | 0.63 |
| Daytime sleepiness | 0.69b | 0.65 | 0.79 | 0.81 |
CSHQ, Children's Sleep Habits Questionnaire; ICC, Intraclass correlation coefficients; SDB, Sleep-disordered breathing.
Our data did not fit the original CSHQ eight domain structure in Confirmatory Factor Analysis as CFI was 0.863 and RMSEA was 0.063. The Exploratory Factor Analysis extracted five factors: daytime somnolence (items 26, 27, 28, 29, 30 and 31), difficulty in settle to sleep alone/sleep anxiety (items 3, 4, 5, 8 and 16), night wakings and parasomnias (items 12, 13, 14, 22, 23, 24 and 25), sleep duration (items 1, 2, 6, 9, 10, 11 and 25) and Sleep-disordered breathing (items 18, 19 and 20).
DiscussionThe CSHQ has already been used for children aged 2 to 3 years but the validation data for this age band is scarce.28 In this study, we found total scale and subscale internal consistencies that were similar to older children.12,17,18
Considering the full sample, the total scale α (0.78) is above the recommended value of 0.70.24 It is also higher than the values described in community samples from the United Sates and Germany (Table 2) and identical to an US clinical sample.12,18 The CSHQ-PT also evidenced convergent validity with the overall parent evaluation of sleep difficulties as children identified as “Problem sleepers” got higher total scores.24
Subscale internal consistencies were similar to the original validation values (see Table 2), except for the lower α for the Sleep Anxiety subscale (0.44). This has already been described in the Dutch and German questionnaires and the same was found for other scales in other languages.12,16–18 In Portugal, it seems that items 7 and 21 are not well adapted to our reality because eliminating them would increase the subscale α to 0.57. Besides that, Factorial Analysis showed that items 3 and 4 were also related to this construct.
Factor analysis (FA) is not described in the original CSHQ validation study.12 We found that our data did not show a good fit to the original subscales in Confirmatory FA but the Exploratory FA extracted 5 factors with an interesting correspondence to the subscale domains. The Dutch community sample did not fit either and 4 factors were determined as in a smaller study with English-speaking children.17,28 These differences may be related to the translation process as well as distinct patterns of sleep behaviors in the studied populations. This is the reason why, despite all the effort involved in the cross-cultural adaptation of questionnaires, the validation of the new versions is mandatory.22,23 Nevertheless, it is appropriate to keep the original CSHQ itens and subscales for Portuguese children for they showed acceptable psychometric properties and they are important for both clinical purposes and cross-cultural comparisons.
The test-retest reliability analysis for subscales showed strong and very strong correlations that were similar or higher than the original ones and comparable to the intraclass correlation coefficients from other studies (Table 3). We also present for the first time test-retest correlations for the sleep schedules and the quantitative sleep duration evaluation of the CSHQ, finding that most of them are above the recommended value of 0.70.24
The mean total CSHQ score in Portuguese children was higher than described before in North American, Chinese, Dutch, German and Hebrew community samples, even when considering only 4-10 years old (mean total score 46.45±7.14).14–18 This finding suggested an higher prevalence of problematic sleep behaviors in our population that needs further investigation.
We present the validation of an international instrument that may be useful for both clinical practice and research. Since the beginning of this project, other children sleep questionnaires were adapted to the Portuguese language in Brazil, having less emphasis in the behavioral dimension of sleep and different age limits.29,30 The adaptation of the CSHQ to the Portuguese language included cognitive interviews with Brazilian parents living in Portugal and showed that the questionnaire was clear to all of them. Therefore, although it was not yet validated in Brazil, the CSHQ-PT also seems adequate for Brazilian populations.21
We do recognize some limitations in our work. We used convenience samples that, although heterogeneous in geographic and socioeconomic characteristics, may not be fully representative of the Portuguese population. Also, we were not able to characterize non responders due to privacy constraints, though we got a fair response rate (74%) comparing to other countries (46.9% in the USA, 63% in Holland and 92% in China).12,15,17 The comparison of the CSHQ-PT results with sleep logs and more objective actigraphy data would also be useful.
In conclusion, our study shows that the CSHQ-PT is comparable to the versions from other countries and has adequate psychometric properties for the screening of sleep problems in children aged from 2 to 10 years old.
FundingThis study was supported by Cuf-Descobertas Hospital.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Silva FG, Silva CR, Braga LB, Neto AS. Portuguese Children's Sleep Habits Questionnaire - validation and cross-cultural comparison. J Pediatr (Rio J). 2014;90:78–84.