The authors investigated the functional status at ICU admission and at hospital discharge, and the impact of dysfunctions on survivors' lifespan.
MethodSingle-center retrospective cohort. The FSS (Functional Status Scale) was calculated at ICU admission and at hospital discharge. A new morbidity was defined as an increase in FSS ≥ 3.
ResultsAmong 1002 patients, there were 855 survivors. Of these, 194 (22.6%) had died by the end of the study; 45 (5.3%) had a new morbidity. Means in the motor domain at admission and discharge were 1.37 (SD: 0.82) and 1.53 (SD 0.95, p = 0.002). In the feeding domain, the means were 1.19 (SD 0.63) and 1.30 (SD 0.76), p = 0.002; global means were 6.93 (SD 2.45) and 7.2 (SD 2.94), p = 0.007. Acute respiratory failure requiring mechanical ventilation, the score PRISM IV, age < 5 years, and central nervous system tumors were independent predictors of new morbidity. New morbidity correlated with lower odds of survival after hospital discharge, considering all causes of death (p = 0.014), and was independently predictive of death (Cox hazard ratio = 1.98). In Weibull models, shortening in the life span of 14.2% (p = 0.014) was estimated as a new morbidity.
ConclusionsNew morbidities are related to age, disease severity at admission, and SNC tumors. New morbidities, in turn, correlate with lower probabilities of survival and shortening of the remaining life span. Physical rehabilitation interventions in this population of children may have the potential to provide an increase in lifespan.
As in adults, in pediatric intensive care, an increase in morbidity has accompanied a decrease in mortality over the last few decades. This has led to a shift in the focus of the international intensive care community from simply reducing mortality to improving survivors’ prognoses.1 Survivors of critical illness can experience substantial and prolonged negative impacts on various aspects of their subsequent quality of life, with functional, psychological, and cognitive deficits.2 Different sequelae in patients interfere with the quality of life. The studies in this field are sparse, with methodological limitations and qualitative heterogeneities, making it difficult to interpret data on new morbidities after intensive care in children.3
Children with cancer who require intensive care constitute a highly complex and challenging population, with significantly worse outcomes when compared to the general population.4 Mortality rates are much higher and have remained relatively unchanged in recent years.5 As for the survivors of these hospitalizations, the authors have no data on functional deficits or newly acquired morbidities. The objectives of this study were to investigate the functional status of children and adolescents with cancer admitted to the ICU, compare the situation at admission to the ICU with the situation at hospital discharge, and describe the general characteristics of patients who developed new morbidity. Additionally, the authors aimed to investigate whether the acquisition of new morbidity would have any impact on the survivors' lifespan.
MethodsThe study consisted of a retrospective cohort including cancer patients under 18 years of age, admitted to the ICU of the Pediatric Institute of Oncology, a referral hospital for childhood cancer, in São Paulo, Brazil, from April 1, 2014, to April 30, 2019. General criteria for admission to the ICU include acute organ dysfunction (cardiac, respiratory, endocrinological, metabolic, neurological, and hematological). Most admissions are surgical, following tumor resection (neurosurgery, thoracic and abdominal surgery, orthopedics). The study was authorized by the Research Ethics Committee from the Federal University of Sao Paulo, under number 0963/2020. The consent form was waived for cases in which it was not possible to contact those responsible for the patient, to authorize access to the medical records. The study was conducted in accordance with the Declaration of Helsinki and the Brazilian regulation for human research.
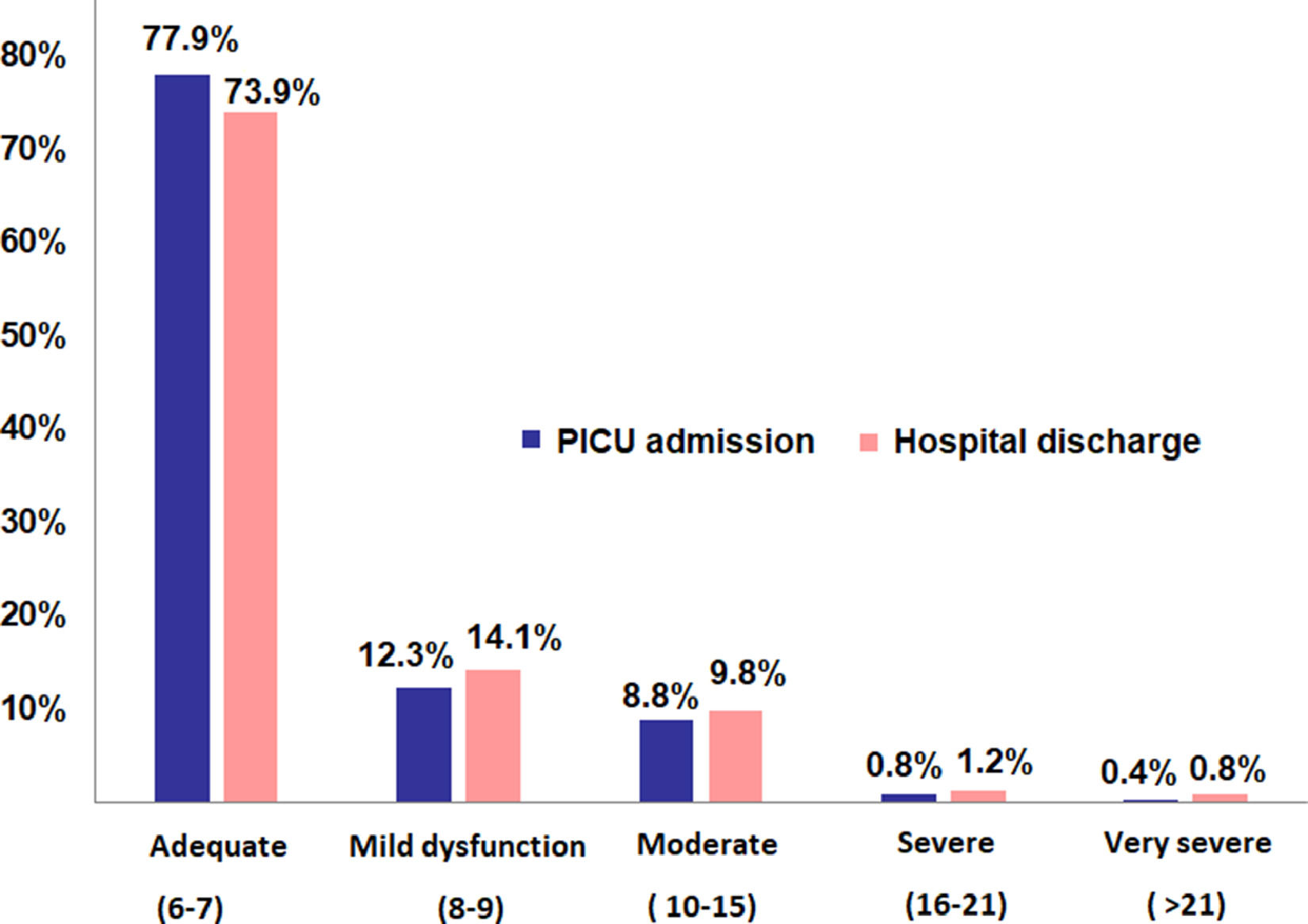
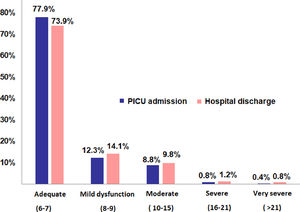
To assess the functional outcomes, the authors used the FSS (Functional Status Scale), applied at admission to the ICU and at hospital discharge. The FSS is composed of six domains (mental status, sensory functioning, communication, motor functioning, feeding, and respiratory status).6 Each domain is scored from 1 point (normal) to 5 points (very severe dysfunction). The total score ranges from 6 to 30 points, and lower scores indicate better functionality. The total score is categorized as follows: 6 - 7, adequate; 8 - 9, mild dysfunction; 10 - 15, moderate dysfunction; 16 - 21, severe dysfunction; and more than 21 points, very severe dysfunction.7 New morbidity, or a significant new change in functional status, was defined as an increase in FSS ≥ 3 points between hospital admission and discharge.1 In the present study's institution, patients undergo rehabilitation and complete follow-up in various outpatient clinics, with a centralized medical record. The follow-up for the study was done through the analysis of the consultations until the end of the stipulated period.
Logistic regression (bivariate and multivariate) was used to evaluate the variables: “sepsis,” “diagnosis of leukemia or lymphoma,” “recurrence of the oncological disease,” “PRISM IV raw scores,” “renal replacement therapy (initiated in this admission, not previous or dependent on dialysis),” “acute respiratory failure with need for ventilation on admission” (intubated immediately before admission or within 4 h of admission, non-invasive ventilation not included),” “hematopoietic stem cell transplantation (HSCT),” “malnutrition with a body mass index (BMI) z-score < −2,” “central nervous system tumors,” “need for vasoactive drugs,” and “age” as risk factors for the outcome “new morbidity.” As the focus was on changes at admission and discharge, the authors chose not to include variables such as ventilation time. For statistical modeling of the risks represented by the above variables on the outcome of “all-cause death after hospital discharge,” the authors used Cox regression. The authors also used the Weibull distribution for Accelerated Failure Time (AFT) models, for the same outcome. An AFT model assumes that the effect of a covariate is to accelerate or decelerate the life course as a result of a condition.8 The percentage of shortening in the lifespan of survivors is calculated as (1-AFT × 100). The authors analyzed the same variables described in the Cox model as conditions for the determination of AFTs. The Kaplan-Meier curve was also used for this outcome, with comparisons using the log-rank test (Mantel-Cox). Differences in distribution were assessed with the Mann-Whitney test. Statistical tests were performed using the software R, version 4.1.1 (The R Foundation for Statistical Computing, 2021, Vienna, Austria). In order to reduce the possibility of bias, each data entry was reviewed by a second investigator. Sample calculations were not performed, as the objective was to analyze all possible hospitalizations in the period. All analyses were based on the complete case data only.
Data availability statementData associated with the paper are publicly available from the corresponding author on request.
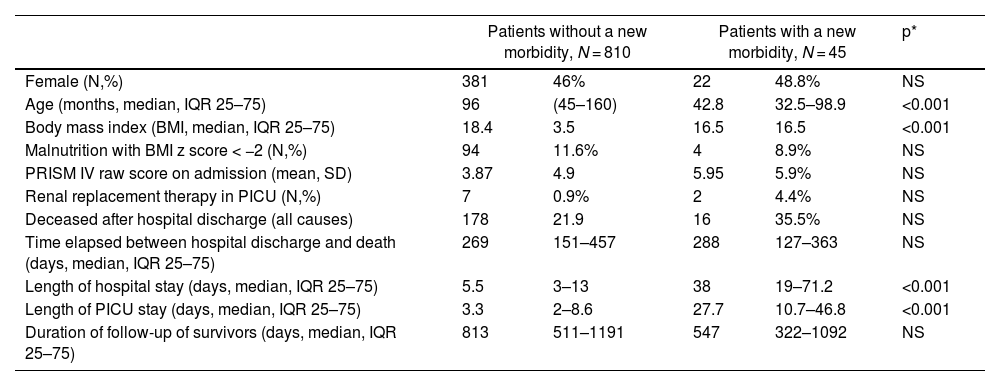
ResultsThe authors assessed data from 1002 patients admitted to the ICU from April 2014 to April 2019; there were 128 deaths during hospitalization (12.7%), leaving 874 patients for survival analysis. After excluding patients with missing data and loss of follow-up, data from 855 surviving patients were included in the analyses. By June 2020, defined as the end of data collection, 194 (22.6%) of these patients had died due to the progression of cancer and other complications, in a median time of 269 days. Forty-five of the 855 survivors had a new morbidity, that is, an increase of at least three points in the FSS score between admission and discharge (5.3%). The characteristics of the patients with and without new morbidities are shown and compared in Table 1. Central nervous system tumors were the most frequent cancer diagnoses (41.7%). Acute lymphocytic leukemia and acute myeloid leukemia were 11% of the diagnoses. More details about the oncological diagnoses and the immediate reason for PICU admission are in Supplementary Table 1.
Characteristics of the patients, according to the presence of a new morbidity at hospital discharge. P* = p-value by chi-square test or Mann-Whitney test, as appropriate. NS, non-significant; IQR, Interquartile range.
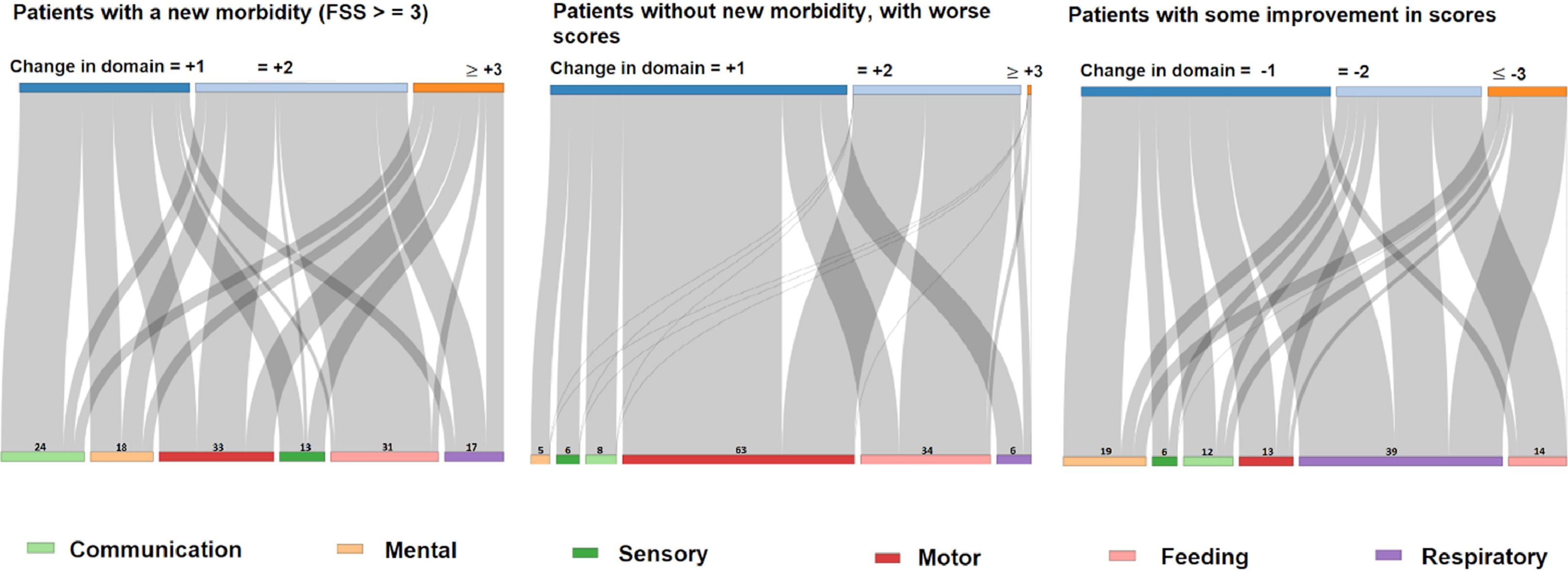
There was a worse FSS score without new morbidity in 104 patients (12.1%), and 63 patients had improvement in the scores (7.3%), particularly in the respiratory domain. The changes observed in each domain are illustrated in Figure 1.
When comparing the scores at admission and at hospital discharge, the authors observed worsening in the motor and feeding domains, reflected in the total score. Means in the motor domain at admission and discharge were 1.37 (Standard Deviation: 0.82) and 1.53 (SD 0.95), with p = 0.002 at the Mann-Whitney test. In the feeding domain, the means were 1.19 (SD 0.63) and 1.30 (SD 0.76), p = 0.002; global means were 6.93 (SD 2.45) and 7.2 (SD 2.94), p = 0.007. The frequencies of the score categories at admission and at discharge are illustrated in Figure 2.
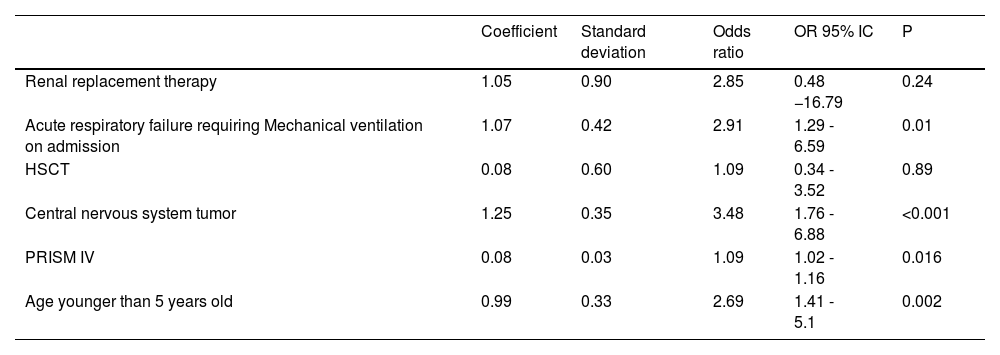
In the risk analysis for developing new morbidity, the variables “renal replacement therapy,” “acute respiratory failure requiring mechanical ventilation on admission,” “central nervous system tumor,” “PRISM IV,” and “age” was predictive of the outcome in bivariate logistic regression models. The results of the bivariate analysis are shown in Supplementary Table 2. The variables with a p < 0.1 in the bivariate analysis were included in multivariate models for the outcome “new morbidity.” The best model is shown in Table 2, where it is noted that the variables “Acute respiratory failure requiring mechanical ventilation, “PRISM IV,” “age younger than 5 years old,” and “central nervous system tumor,” were independent predictors of new morbidity.
Multivariate model for the outcome “new morbidity”.
As for the 45 patients with new morbidity, 16 (35.5%) died during the study assessment period. The mortality of patients without new morbidity was 21.9% (178/810). In the survival analysis, the development of new morbidity was correlated with lower probabilities of survival after hospital discharge in the log-rank test (p = 0.014). The variables included in the bivariate Cox regression models for the outcome “death from all causes after hospital discharge” are shown in Supplementary Table 3. In the multivariate model, the authors included no variables that showed a dependent relationship with the outcome “new morbidity” in the logistic regression (PRISM IV, age, renal and respiratory failure, and central nervous system tumor). The objective was to define whether the variable “new morbidity” would be predictive of death from all causes in survivors. In this model, the new morbidity was shown to be an independent predictor for this outcome with a hazard ratio = 1.98 (95% CI: 1.18–3.32, p = 0.009), in relation to diagnosis of lymphoma or leukemia, cancer recurrence, HSCT and malnutrition (BMI z score < −2). The variables “malnutrition” (HR 2.21, 95% CI: 1.53–3.18, p < 0.001), and “cancer recurrence” (HR 2.47, 95% CI: 1.67–3.64, p < 0.001) were also independent predictors of this outcome.
The same variables analyzed in the Cox multivariate model were analyzed with the Weibull regression to determine the accelerated failure times, and the authors observed that the acquisition of new morbidity was related to a percentage of shortening in the remaining lifespan of 14.2% (p = 0.014). Other independent factors were cancer recurrence (shortening of 19.1%, p < 0.001) and malnutrition (shortening of 17%, p < 0.001). The complete model is in Supplementary Table 4.
DiscussionThe development of new morbidities during hospitalization in pediatric oncology ICUs is still an unexplored field, and the data presented in this work are epidemiologically relevant. The fact that 5.3% of surviving patients had new morbidity shows that this outcome should be monitored, alongside mortality, as a negative outcome to be improved. Survivors of childhood cancer are at risk of lower life expectancy throughout adult life, with considerable variation among diagnoses.9 The authors have demonstrated in the present work that survivors of an oncology ICU admission are also at risk of a lower life expectancy in the years to come if they experience new morbidity during that hospitalization. In addition to more obvious factors such as malnutrition and recurrence of the oncological disease, a newly acquired morbidity was related to a greater probability of death after hospital discharge and a shortening of the remaining lifespan by about 14%. It is obvious that the design of this study, a retrospective cohort, does not allow causal inference, nor does it allow to differentiate a new morbidity acquired by a natural complication of the disease from one acquired by failures in the quality of care. For example, surgery for a posterior fossa tumor may naturally result in severe dysphagia, with a risk of broncho-aspiration and pneumonia. However, potentially preventable causes, such as respiratory morbidities caused by pneumonia associated with prolonged mechanical ventilation, or motor limitations caused by muscle weakness due to excessive sedation and lack of early mobilization,10 are together in the same outcome. This difficulty in distinguishing between underlying disease and intensive care complications is a common deficiency in follow-up studies.11 There is a paucity of longitudinal epidemiological studies with control groups that consider patients' pre-hospitalization functional status in the PICU, with the ability to describe the duration and nature of recovery.12 Nevertheless, a focus on preventable causes of new morbidities acquired during PICU stay can improve these children's survival.
The multivariate model that best explained the occurrence of new morbidity showed that respiratory failure requiring mechanical ventilation, central nervous system tumors, the PRISM IV score, and age younger than 5 years old are independent predictive variables. Younger children have a lower capacity for the healing process that follows intensive care, as well as for acquiring new age-appropriate skills.13 In a 2009 study, Knoester et al. reported that in children aged 1 to 6 years old, respiratory problems, mood, and activity disturbances were more frequent 3 and 9 months after an ICU admission.14 The PRISM IV score correlation confirms the findings of previous studies, that acute illness severity at ICU admission is associated with greater morbidity in survivors.15 Central nervous system tumors in children often have a devastating effect on survivors' quality of life because of the disease and treatments, including surgery, radiation, and chemotherapy. Long-term effects include sensory and neuroendocrine abnormalities and motor and cognitive deficits. Some treatments, such as radiotherapy and intrathecal methotrexate, have been associated with neurocognitive deficits. Younger patients tend to have a worse prognosis, showing the greater vulnerability of immature brains to disease and treatments.16,17 The duration of mechanical ventilation has been related to a greater probability of dysfunction or death in children.18 The authors did not assess the duration of ventilation, but the need for it at admission, which characterizes a greater severity in an acute form.
Motor and feeding were the most frequently observed disorders in patients with a change in FSS of at least +2 points. This was also observed in the studies by Pollack et al.1 and Pereira et al.19 in children of general ICUs and reinforces the need for early intervention for mobilization and swallowing therapy.
In addition to the already discussed limitations regarding the study design, other weaknesses may include a selection bias, as the present study's hospital mainly treats referred and critically ill patients. Because it was performed in a single center, the findings of this study may not be generalizable to other pediatric oncology ICUs. The authors did not search for the baseline FSS status (before PICU admission), because the purpose was to assess the new dysfunctions acquired during the PICU stay, and most of the admissions were surgical, particularly neurosurgeries for tumor resection, which can drastically change the child's functional status in the immediate postoperative period. So, for that purpose, the baseline status could not be useful.
ConclusionsNew morbidities can be observed in about 5% of cases at hospital discharge of children with cancer who survive ICU hospitalization and are correlated with a shortening of the remaining lifespan that can reach 14%, regardless of other factors such as disease recurrence and malnutrition. Patients most predisposed to having new morbidity are those with greater acute severity at admission, requiring mechanical ventilation, younger patients, and patients with central nervous system tumors. This study reinforces the need for rehabilitation interventions still in the intensive care unit, particularly in the motor and feeding domains.
Only institutional (IOP/GRAAC).
Institution: Grupo de Apoio ao Adolescente e à Criança com Câncer (GRAACC)/ Institute of Pediatric Oncology (IOP)/ São Paulo Federal University (UNIFESP).