Compare the occurrence of choking and gagging in infants subjected to three complementary feeding (CF) methods.
MethodsRandomized clinical trial with mother-infant pairs, allocated according to the following methods of CF: a) Parent-Led Weaning (PLW) — group control, b) Baby-Led Introduction to SolidS (BLISS), and c) mixed (initially BLISS and if the infant presents a lack of interest or dissatisfaction, PLW), with the last two methods guided by the infant. Mothers received nutritional intervention on CF and prevention of choking and gagging according to the method at 5.5 months of age and remained in follow-up until 12 months. Frequencies of choking and gagging were collected by questionnaire at nine and 12 months. The comparison between groups was performed using the analysis of variance test (p < 0.05).
Results130 infants were followed, and 34 (26.2%) children presented choking between six and 12 months of age, 13 (30.2%) in PLW, 10 (22.2%) BLISS, and 11 (26.2%) mixed method, no significative difference between methods (p > 0.05). The choking was caused mainly by the semi-solid/solid consistency. Moreover, 100 (80%) infants aged from six to 12 months presented gagging and their characteristics were not statistically different among groups (p > 0.05).
ConclusionInfants following a baby-led feeding method that includes advice on minimizing choking risk do not seem more likely to choke than infants following traditional feeding practice that includes advice on minimizing choking risk.
The introduction of complementary feeding (CF) is recommended from the age of six months, in addition to breast milk or infant formula. Usually, from six months onward, healthy infants show signs of readiness and skills that indicate the possibility of safely starting CF.1
Traditionally, CF should start with porridge or puree food offered by an adult by spoon, and then progress to the same consistency of the family's food by the end of the first year. This approach is called Parent-Led Weaning (PLW), in which the parents take the lead at mealtime.2 Other methods have become popular in recent years, such as Baby-Led Weaning (BLW)3 that encourages, since the beginning of CF, the exclusive offer of solid foods, cut or sliced, thus the child feeds food to their mouth; and Baby Led Introduction to SolidS (BLISS),4 which is an adaptation of the BLW, whose foods are also presented in solid consistency with child-safe cuts, and additionally, and only foods with lower risks for choking are chosen, as well as iron-rich and energy-rich foods. Both methods promote the child's autonomy and allow for infant self-regulation.5
All CF methods present benefits and risks, such as the child's autonomy and the child's ability to self-regulate—the use or not of utensils—differences in the absorption and intake of iron-rich foods, the reduction of the difference between the child's diet and family nutrition, and the fear of choking episodes.4-11
The risk of choking is often a concern among parents, caregivers, and healthcare professionals.4,6,7,10-14 Unlike gagging (or nausea or gag reflex), which helps to protect the airways during the swallowing process,15 choking is a serious event in which the airway is partially or completely obstructed by a foreign body, making it impossible for the children to resolve it on their own, requiring choking maneuvers or medical assistance.
In the literature, there are few studies assessing the choking outcome related to CF methods,9,10,16 and none in Brazil at the time of this study. Moreover, studies published to date use different approaches to classify CF methods.9-10 Given the gap in knowledge about cases of choking and gagging among children undergoing different CF methods, this paper aimed to compare the occurrence of choking and gagging in infants subjected to three CF methods—PLW, BLISS, and mixed, in the first year of life.
MethodsThis study protocol was published,17,18 registered in the Brazilian Clinical Trials Registry (ReBEC), and approved by the Hospital's Research Ethics Committee. This is a parallel randomized clinical trial with three intervention arms according to the CF method: (A) PLW, the control arm; (B) strict BLISS; and (C) mixed, a combination of PLW and BLISS, created especially for this study. The three methods are explained below:
- •
PLW: Initially, the consistency of the food should be pasty, kneaded with a fork (six to eight months in the form of porridge and puree), and gradually progress to the consistency of family food at 12 months of age, with a variety of colors and food groups at every meal, without mixing or sifting food.19 The main characteristic of this goal is the greater influence of parents in the feeding process.19
- •
BLISS: parents were instructed to encourage the infant to feed by themselves, always accompanied by an adult. The consistency of the food offered from six months must be firm, to allow the infant to feed with their own hands and that they can chew; cut into elongated shapes, such as strips or sticks, to facilitate the pinching of the fingers and prevent choking. Parents were advised to avoid rushing the child during the meal, respecting their time to explore flavors and textures, and offering three types of food at each meal: iron-rich food, energy-rich food, and fiber-rich sources.5
- •
Mixed: parents were instructed to initially apply the BLISS approach. If the child was not satisfied or showed disinterest, they were instructed to offer the food using the PLW technique during the same meal.17,18
Regardless of the CF method, it was oriented to start with two meals (breakfast and lunch) and after one month include dinner; without rigid schedules (no time-imposed) and respecting the child's appetite; and always with the presence of an adult.19
Mothers living in the Porto Alegre, Brazil, and the metropolitan area were considered for inclusion purposes, with their healthy, term, non-twin infants, with birth weight ≥ 2,500g, whose age group was below six months of age and had not started the CF process yet. The pairs of mothers-children were recruited via the local newspaper and an online invitation with social networking pages aimed at mothers’ groups. In the first contact, after checking the inclusion criteria, those considered eligible received a standardized message explaining the study's details, risks, and benefits, and any additional questions were answered by the researchers. After confirming interest, a consent form was sent by email. Once the signed consent form was received back, along with an initially completed questionnaire, the participant was randomly allocated a group. The participants were sequentially numbered and entered a randomization list of three blocks and equal numbers, generated by a computer (http://www.randomization.com) via a researcher not involved (blinded) in the intervention or data collection. Mothers were only aware of which group they were allocated to at the first intervention.
After randomization, groups of three to eight pairs were submitted to a specific intervention according to the CF methods (BLISS, PLW, or mixed). The intervention took place when the infant was 5.5 months old, in a private nutrition clinic equipped with an experimental kitchen, and was conducted by two nutritionists who provided detailed guidance on the proposed CF method for the group allocated and taught cuts and food preparations according to the method. A speech therapist guided signs of readiness necessary for the onset of CF, the definition and differentiation of gagging and choking, and instructions on the Heimlich maneuver, via printed educational materials (Figure 1) and videos illustrating the gagging, choking, and maneuvers. Due to the COVID-19 pandemic, some interventions took place remotely, by videoconferencing in virtual communication applications with the same guidelines and team involved in the face-to-face intervention.
Mother and child data were collected using an online questionnaire, the questioned data were: maternal schooling level (years), maternal skin color (White or non-White—Mixed-race, Black, and Yellow), marital status (living with a partner or not), number of children, monthly family income (Brazilian reais), prenatal care (yes or no), breastfeeding guidance (yes or no), type of childbirth (cesarean section or vaginal childbirth), child's birth weight (g), length of the child at birth (cm), breastfeeding in the first hour of life (yes or no), age of introduction of solids (days), who usually accompanies the child's meals? (mother or others), breastfeeding at nine months (yes or no), breastfeeding at 12 months (yes or no), use of a baby bottle at 12 months (yes or no), use of a pacifier at 12 months (yes or no), finger-sucking at 12 months (yes or no). Breastfeeding practice was defined as receiving any amount of human milk by bottle, cup, or breast, regardless of any other food offering.20
The participants received a reinforcement of infant feeding counseling at nine months by home visits, and at 12 months by attending the hospital. At nine months and 12 months of age, the questionnaire built for this study based on the literature was applied,9,10,16 in a face-to-face or remote meeting during the COVID-19 pandemic. The variables considered for this study were as follows: occurrence of choking; consistency of the food that caused the event; type of food involved, need or not to gag, presence of the gagging, gagging frequency, and the food that triggered the reflex. Choking was considered partial or total obstruction of airflow, caused by the entry of a foreign body that can cause cyanosis and/or asphyxia and gagging. The first episode of choking or gagging was considered for analysis.
The sample size of the primary outcome of the randomized clinical trial was calculated using WinPepi® software version 11.65. Considering a unit standard deviation of 1, the statistical power of 80%, and a significance level of 5% to detect a difference in body mass index of 0.8 kg/m2,16 the sample calculation for a half standard deviation difference consisted of 48 mother-infant pairs for each of the three intervention groups. For the secondary outcomes explored in this article, the sampling power was calculated a posteriori considering a significance level of 5%, the sample size of 130 subjects, chocking proportions of 35% (PLW) and 70% (BLISS and mixed),16 and applying continuity correction, a power of 94.1% was reached with the recruited sample. This calculation was performed using the online version of PSS Health online.
The database was created using the program Statistical Package for the Social Sciences (SPSS 21.0) with double entry and further validation. The CF method was considered the independent variable and the episodes of choking and gagging were the variable dependent. A descriptive analysis of the categorical variables of the data was performed, presented as relative and absolute percentages. For quantitative variables, median, interquartile range, mean, and standard deviation were used. The Chi-Square test or analysis of variance (ANOVA) was used and a p < 0.05 significance level was adopted to compare variables. Data were analyzed by intention to treat.
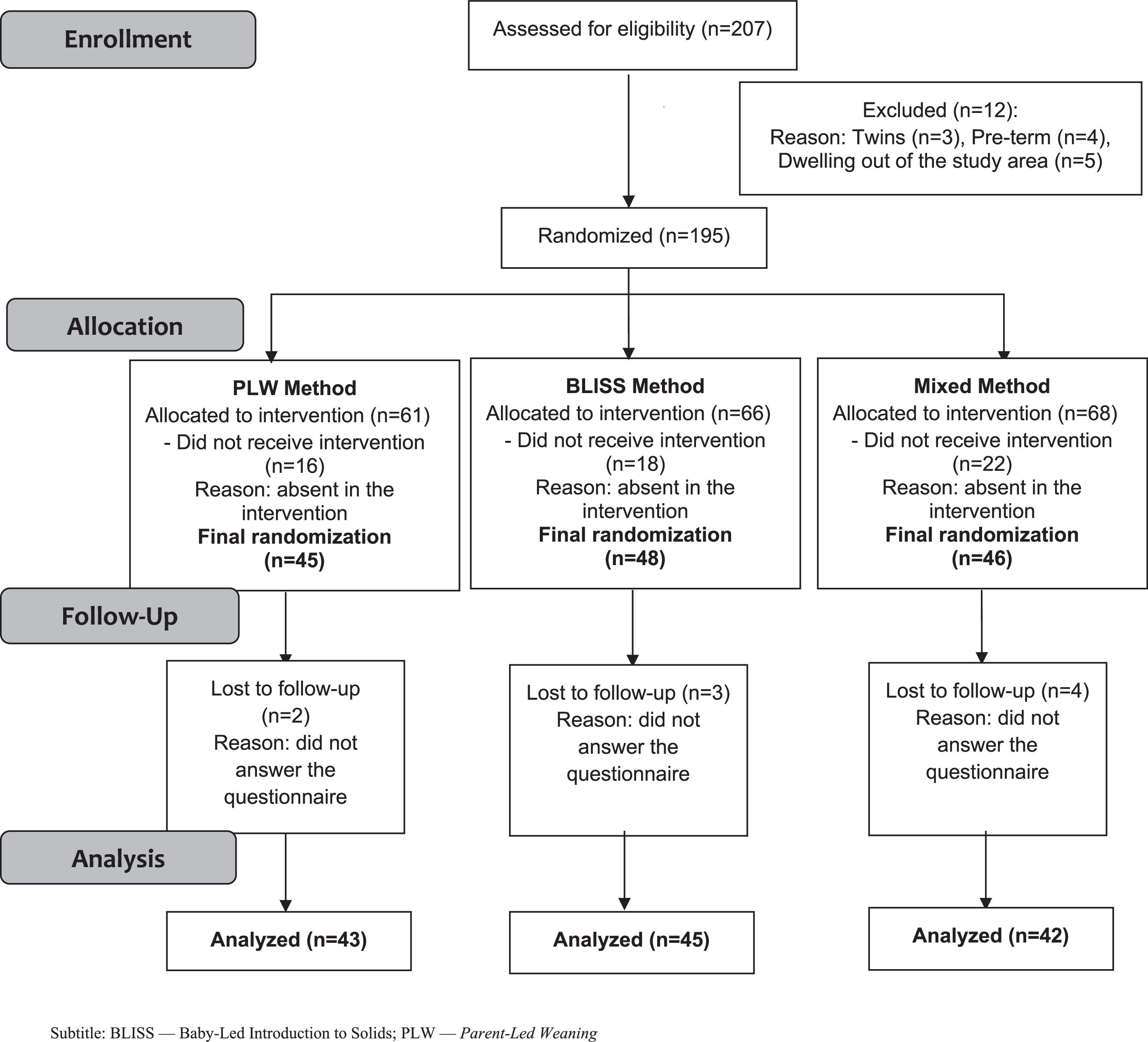
ResultsA total of 207 mother-infant pairs contacted the research team, out of which 12 (5.8%) did not meet the inclusion criteria, leaving 195 mother-infant pairs eligible that were randomized. There were 56 (27.0%) mother-infant pairs who chose not to proceed with the interventions. Mothers who did not attend the intervention did not differ in race/ethnicity (p = 0.607) and maternal age (p = 0.112), however, had lower education (p = 0.003) and lower family income (p = 0.028) compared to the families included. A total of 139 mother-infant pairs were included in the study, 45 (32.4%) in the PLW, 48 (34.5%) in the BLISS, and 46 (33.1%) in the mixed method. During the follow-up, nine mother-infant pairs failed to answer the questionnaires. Data from 130 mother-infant pairs were analyzed in the study. The clinical trial profile is shown in Figure 2, from the recruitment of the mother-infant pairs until the evaluation of the 12 months of children's age.
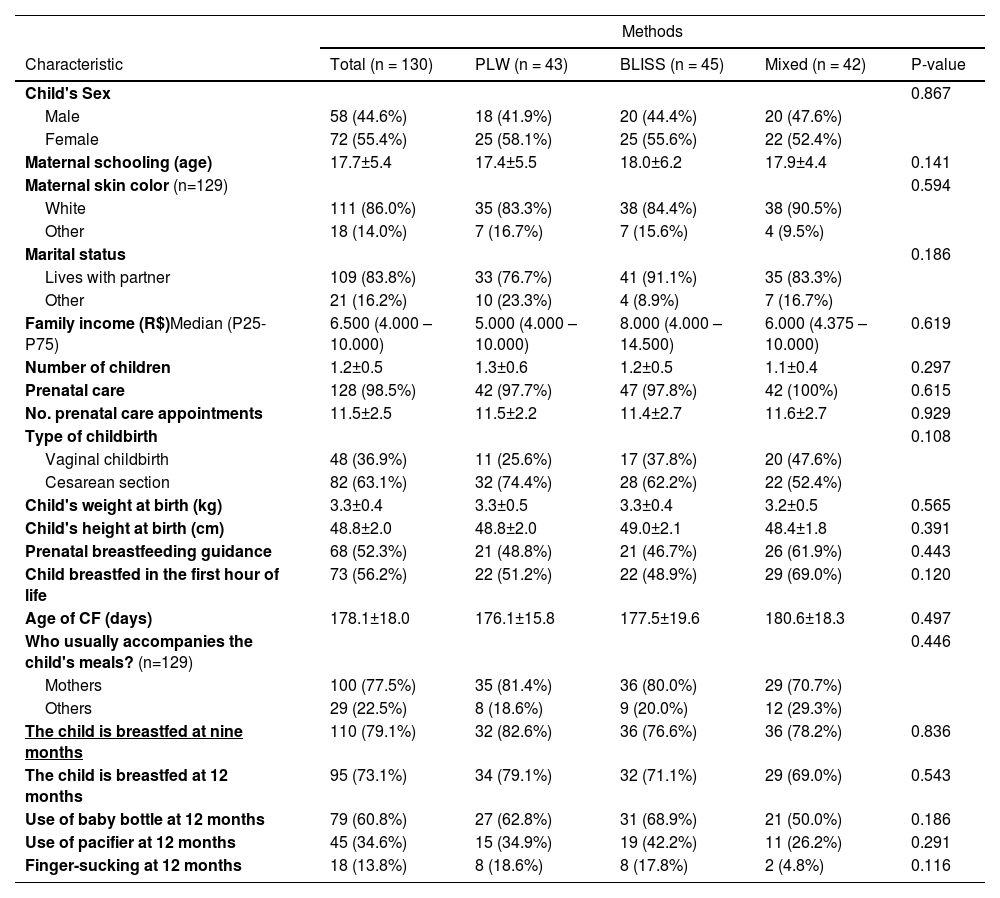
Table 1 describes the sample. In most cases, mothers were responsible for feeding the child (n = 100; 77.5%). Mothers with mean schooling of 17.7 ± 5.4 years and a family income of around five minimum wages composed the sample. The CF methods presented no statistical difference (p > 0.05).
Characterization of the total sample by the method of food introduction.
BLISS, Baby-Led Introduction to Solids; CF, Complementary Food; PLW, Parent-Led Weaning; CI, confidence interval; Chi-square test (p < 0,05); ANOVA test (p < 0,05).
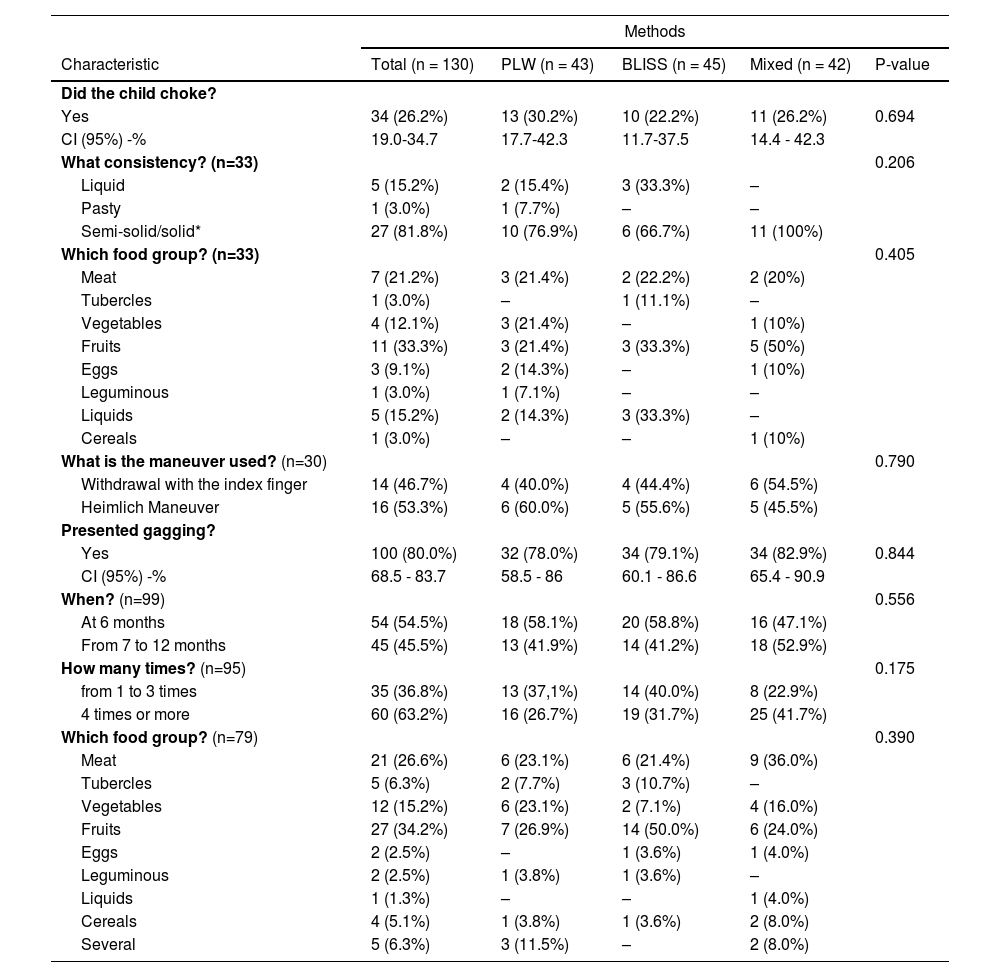
Table 2 shows data on choking and gagging. During CF, 26.2% (n = 34) of infants presented choking, in which 81.8% (27/33) of the episodes occurred with semi-solid or solid foods and 33.3% (11/33) with fruits. The methods of CF- PLW 30.2% (13/43), BLISS 22.2% (10/45), and mixed 26.2% (11/42) - had no statistically significant difference in choking episodes (p = 0.694). The gagging appeared in 80% (n=100) of infants in the first year, 54.5% (54/99) at six months, 45.5% (45/99) from seven to 12 months, and 34.2% (27/99) with fruits.
Characterization of choking and gagging episodes in the total sample and by food introduction method (n = 130).
BLISS, Baby-Led Introduction to Solids; PLW, Parent-Led Weaning; CI, confidence interval*. The consistency depended on the method applied and the age of the child.; ANOVA test; p < 0,05.
Episodes of gagging with the CF methods - PLW 78.0% (32/43), BLISS 79.1% (34/45), and mixed 82.9% (34/42) - presented no statistically significant difference (p = 0.844). Medical care was not required for the identified choking episodes, as the degassing maneuver and removal with the index finger managed the event.
DiscussionIn this study, the occurrence of choking and choking episodes was similar to the CF methods. The occurrence of at least one choking episode was 30.2% in the PLW, 22.2% in the BLISS, and 26.2% in the mixed. Regarding the occurrence of gagging, 78.0% of the mothers using the PLW reported at least one episode, 79.1% using the BLISS, and 82.9% using the mixed-in infants in the first year of life. Regarding the occurrence in all infants, 26.2% had at least one episode of choking, and 80.0% had gagging. Previous studies in the literature evaluated choking episodes considering the CF methods with a frequency of 1% and 35%.7,9,10,21,22,16 The frequency found in this sample was like the populations, and none of the studies found significant differences between the methods regarding the occurrence of choking.
A systematic review published in 2021 that evaluated 29 articles on the benefits and risks of BLW/BLISS-type methods, showed that choking is a frequent concern for parents who do not follow the BLW/BLISS.11 Another meta-analysis, published in 2022, concluded that there is no cause-effect relationship between choking and BLISS/BLW.23 Non-systematic reviews also indicated the lack of evidence of a relationship between the BLISS/BLW-type methods and the occurrence of choking.24,25 Although there are original articles on gagging and systematic reviews on the risks and benefits of the BLW/BLISS, the occurrence of gagging is not addressed.
A study comparing the PWL, BLW, and BLW adapted9 retrospectively evaluated the occurrence of choking after defining the event, differentiating it from gagging, as the present study did. The overall percentage of choking among the PLW (11.6%), BLW (11.9%), and BLW adapted (15.5%) was not significant and did not relate to comparisons with sample description data. However, when comparing the groups with the type of food offered to the child, those who followed the traditional method had a greater number of choking episodes when fed with “finger foods and lumpy purees”, suggesting that exposure to different textures, especially the more complex ones, may contribute to protection against choking.
The longitudinal study that compared the PWL and BLISS10 was the only one that -in addition to differentiating and verifying the occurrence of choking and gagging - guided minimizing risk and management in the event of choking, which was the protocol used in this paper. Questionnaires and daily calendars collected choking and gagging frequencies, in addition to measuring exposure to foods with a risk of asphyxia. The groups (PWL and BLISS) had no significant difference in the number of choking events, both by the questionnaire and by the calendar. Gagging was more frequent at six months in the BLISS (94.7%) compared with the PLW (80.7%). The methods and data presented10 are similar to this study, except that the authors tested the third method in the study, the mixed, which combines the techniques allowing the child to have greater autonomy over meals.
The PLW transfers the feeding control from the child to the parents, unlike the BLISS or BLW, whose autonomy of child feeding is the basis of both methods. The role of parents in controlling the choice of what is offered, and the amount of food ingested, affects the child's autonomy and ability to self-regulate if they do not respect the signs of hunger and satiety shown by the child.16 In this study, besides testing the PLW and BLISS methods, the authors also evaluated a third group that initially received whole foods and, if they showed disinterest, received the foods by spoon - the mixed method. Preliminary data demonstrate that this approach has greater adherence compared to PLW and BLISS.26 Therefore, this can be a safe approach to be guided, especially regarding the risk of suffocation.
No evidence that softened consistencies should be prioritized, since offering food in this way would limit the energy density necessary for the child's development, in addition to impairing orofacial development and increasing the risk of food selectivity.11,27 Offering solid foods at the beginning of food introduction allows for the exploration of different textures, favors sensory perception, and stimulates the control and handling of food in the oral cavity, promoting safe chewing and swallowing function.11,25 The occurrence of choking and gagging in all consistencies highlights the need to pay attention both to consistency and to the characteristics and form of food presentation, as well as for the development of the child's oral motor skills.9,11,19,28-30
Besides preparations in the form of food presentation with a potential risk for choking, and regardless of the CF methods used, this study carried out basic care guidance during feeding to avoid choking. Care measures, including how to deal with choking episodes and choking maneuvers, and information about food, ensure that CF can be conducted safely, regardless of the method used.10,29 Moreover, the presence of an adult constantly supervising the child at feeding provides safety to avoid choking and handling them correctly, as well as promoting a pleasant food environment for the child and the family.9,29
This study showed that the presence of the mother during the child's feeding may have provided a better identification of choking episodes and an agile solution to the event, making feeding safer regardless of the method used. All episodes of choking were resolved at home with the indicated maneuvers, without the need for specialized support. In a recent study, mothers report the benefit that knowledge about choking events can make a difference in CF, when these events are correctly identified and understood as common situations in the routine of learning to eat, thus making the process for parents and children more pleasant, healthy, and safe.14
The present study has limitations. Despite the possibility of memory bias, as the authors applied the questionnaires retrospectively, we believe that choking episodes are memories that mark mothers. Most of the sample was socioeconomically favored, which may limit the applicability to other socioeconomic realities. Furthermore, parental behavioral issues and child behavioral issues were not investigated and may be involved in the occurrence of choking. The strength of this study is the single-blind, randomized clinical trial design. Since inception, the authors designed the study to investigate infant safety in different CF methods, after intervention with a speech therapist on gagging, and prevention and management of choking.
Finally, infants whose mothers received intervention for the introduction of CF via infant-guided methods did not present more choking episodes than infants whose mothers received intervention for the PLW. Thus, it is suggested that infant-guided methods can be safe if caregivers receive guidance on the prevention and management of possible episodes of choking. The authors emphasize the need for more studies to investigate this relationship in other locations.
Trial registrationBrazilian Clinical Trials Registry (ReBEC): RBR- 229scm number U1111-1226-9516. Registered on September 24, 2019.
Fundação de Apoio à Universidade do Rio Grande do Sul (FAURGS), Brazil, No. 36908; Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Brazil, No. 2019-0230; Fundo de Incentivo à Pesquisa e Eventos (FIPE), Hospital de Clínicas de Porto Alegre (HCPA), Brazil, No. 2019-0230.
Institution or service with which the work is associated for indexing in Index Medicus/MEDLINE: Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Brazil; Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, Brazil.