This pre/post-intervention study aimed to evaluate neonatal outcomes after the implementation of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics.
MethodThis interventional study was conducted across five secondary healthcare regions that supported 62 cities in the southwestern mesoregion of Piauí. It included 431 healthcare professionals responsible for neonatal care in the study region. The participants were trained in neonatal resuscitation through the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics. Delivery room structuring, healthcare professionals’ knowledge, and neonatal care outcomes were analyzed immediately before and after intervention and after 12 months between February 2018 and March 2019, and healthcare professionals were evaluated.
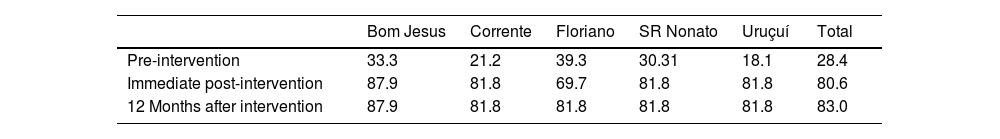
ResultsTraining was conducted for over 106 courses. As a participant could take multiple courses, 700 training sessions were conducted. Regarding delivery room structuring, the acquisition of materials required for resuscitation increased from 28.4 to 80.6% immediately after the intervention and to 83.3% after 12 months. Knowledge retention was significant in the post-training period, with a 95.5% approval rate, and knowledge acquisition was satisfactory after 12 months. The number of newborns transferred during the study period increased significantly. A 72.6% reduction in mortality at birth was recorded, and 479 newborns were resuscitated.
ConclusionFollowing the implementation of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics, structural improvements in delivery rooms, adequate knowledge retention regarding neonatal resuscitation, and a consequent reduction in neonatal mortality were observed.
In Latin America, although approximately 95% of births occur in hospital units, neonatal mortality is four times higher than that in North American and European countries.1–5 In Brazil, infant mortality has declined in recent decades; however, the rate remains at 12 deaths per 1000 live births, which is considerably higher than that in developed countries such as Japan and Finland.3,4,6–9 This situation is related to the difficulty in reducing early neonatal mortality rates and may be associated with the time of birth and perinatal asphyxia.8,10–15 In the northern and northeastern regions of Brazil, neonatal mortality is significantly higher than that in other parts of the country. Additionally, in many Brazilian regions, data regarding early neonatal mortality are uneven owing to high rates of underreporting.16–18 According to DATASUS data from 2011 (Supplementary Fig. S1).14,15,17–19 the state of Piauí, located in the northeastern region of Brazil, has the third highest rate of early neonatal mortality in the country. The southwestern mesoregion of Piauí is a remote territorial division with high socioeconomic vulnerability, high rates of underreporting of neonatal mortality, and a health system weakened by the lack of pediatricians and obstetricians.
Therefore, this study analyzed the impact of training healthcare professionals using the Brazilian Society of Pediatrics’ (Portuguese abbreviation SBP) Neonatal Resuscitation Program (Portuguese abbreviation PRN-SBP) on neonatal outcomes in the southwestern mesoregion of Piauí.15,16–18,20,21
Materials and methodsAn interventional study was performed across five secondary healthcare regions that supported 62 cities in the southwestern mesoregion of Piauí. The five regions included in this study were Floriano, São Raimundo Nonato, Uruçuí, Bom Jesus, and Corrente.17,18
Study phasesPre-interventionThe five study sites were visited between February 24 and 27, 2018, to assess and record delivery room conditions. This assessment involved a consideration of the presence or absence of materials listed in Ordinance SAS/MS 371/2014, which established the guidelines for the organization of comprehensive and humane care for neonates in Brazil's Unified Health System.
The list of supplies needed for delivery room resuscitation (Supplementary Appendix 1) was based on the recommendations published by the International Liaison Committee on Resuscitation (ILCOR)-Neonatal Life Support Task Force. The ILCOR recommendations aid the construction of guidelines adapted to the reality of each region or group of regions, thus serving as a reference to the guidelines of the Neonatal Resuscitation Program of the Brazilian Society of Pediatrics.
From the list of materials required for neonatal resuscitation (Supplementary Appendix 1), 11 items considered fundamental were selected (Supplementary Table S1) as a baseline.
To choose the 11 fundamental items, the following was considered as the criterion: the minimum materials needed to ensure upper airway suctioning, pulmonary ventilation, orotracheal intubation, umbilical catheterization, and infusion of drugs and volume expanders.
Two categories were defined in the analysis of the delivery room structure:
- •
Satisfactory (all fundamental items + 80% of items required for neonatal resuscitation).
- •
Unsatisfactory (absence of at least one fundamental item).
In this course, the authors trained a total of 431 healthcare professionals (doctors, nurses, physical therapists, nursing technicians, and nursing assistants) who worked in delivery rooms in the five cities. The courses were taught exclusively by the researcher, who was both a pediatrician and a PRN-SBP-accredited instructor from March 1, 2018, to June 1, 2018. The following courses were taught: resuscitation of 34-week-old or older newborns, resuscitation of newborns younger than 34 weeks, and transport of high-risk newborns. Each course had a workload of 8 h. Initially, the participants took a pre-test containing 25 multiple-choice questions. The course, designed by the PRN-SBP comprised two theoretical lessons and four practical lessons. Each 8-h course trained approximately 6–8 participants. The SBP certified those who scored ≥80% in a post-test (PT1) with the same multiple-choice questions used in the pre-test (Supplementary Fig. S2).20,22,23
Post-interventionAfter 12 months of intervention, from June 27, 2019, to July 3, 2019, the conditions of delivery rooms were assessed according to the same criteria followed during the pre-intervention period. For this assessment, the researcher followed the previously contacted healthcare professionals fortnightly for 12 months through social networks. In the same period, a sample of healthcare professionals who took a course on resuscitation was randomly selected to take the same post-test (PT2) for the evaluation of PRN-SBP. A score of at least 80% was considered a satisfactory performance and indicated knowledge retention.22 The formula for estimating the proportion for a finite population of 325 students was used to calculate the sample size, with an alpha significance level of 5% and a sampling error of 5%. According to the results, a minimum sample size of 47 students was calculated. Similarly, 12 months after the training sessions, data on neonatal care—the number of external transfers to diverse neonatal reference units, number of delivery room deaths, and number of children who were resuscitated—were collected. The latter was defined as children who underwent positive pressure ventilation under a mask and/or any other advanced procedure (intubation, cardiac massage, umbilical catheterization, use of drugs, and/or expanders). Spreadsheets for data collection and training for the correct completion by healthcare professionals in each location during the intervention period of the study were prepared.
Ethics approval statementThe study was approved by the Ethics and Research Council (CEP) of the State University of Campinas. CAAE: 74978217.5.0000.5404. Proposing institution: School of Medical Sciences- Unicamp. No.: 2.331.312. All the enrolled healthcare professionals signed the informed consent form and were informed regarding the phases of the research.
Patient and public involvementPatients or the public were not involved in the design, conduct, reporting, or dissemination plans of the present research.
ResultsThe intervention involved 431 healthcare professionals (doctors, nurses, and nursing assistants/technicians) from the southwestern mesoregion of Piauí. In this study, 700 training sessions were performed through 106 PRN-SBP courses involving professionals from the five cities in the study: 580 training courses for professionals working in hospitals, and 120 for exclusive professionals of the air and land emergency service.
The training was offered to all 87 doctors working in newborn care in the five study regions, of whom 65 (74.7%) participated. The southwestern mesoregion of Piauí only had 11 pediatricians for the five health regions. In total, 91% (10/11) of the pediatricians and 82.3% (14/17) of obstetricians participated. The other doctors did not present documentation proving any medical specialty. All non-medical professionals who worked in newborn care in the mesoregion participated in the program.
The assessment of delivery rooms, as described in the methodology of the study, showed that none had the essential items for neonatal resuscitation. Some non-conformities were observed during the assessment of inventories in the delivery rooms; for example, auto-inflatable balloons and neonatal masks were absent in the delivery rooms of four of the five cities. Instead, the following were used: adult face masks and laryngoscopes for resuscitation of newborns, auto-inflatable 1000-mL balloons, disposable plastic cups adapted as face masks, and cuffed pediatric tubes. Many newborns were received on marble stones, support tables, and acrylic neonatal cribs without heating. Incubators were often damaged and unusable.
The average percentage of materials found in the study region was 28.4% in the pre-intervention period. At the immediate post-intervention moment, an average outreach of 80.6% was achieved, representing an increase of 52.2%. This further increased to 83.0% 12 months after the intervention (Table 1). Before the intervention, the average was 61.9%. After the immediate intervention, all birth sites reached 100% adequacy and maintained this index up to 12 months after the intervention (Figs. 1 and 2).
Regarding the acquisition of materials necessary for resuscitation and establishment of a strategy related to the practice of immediate care that should be performed within the newborns’ first minute of life, the researchers suggested that the tables used for the organization of materials in the delivery rooms be lined with yellow-gold towels to emphasize the importance of an adequate transition from intrauterine to extrauterine life in the first 60 s of life; that is, the Golden Minute (Supplementary Fig. 3). The assessment for the course on the resuscitation of ≥34-week-old newborns, which was applied during training, consisted of 25 questions and required a minimum of 80% as a passing score. This test was randomly administered to a sample of 167 healthcare professionals 12 months after the intervention and the participation of physicians, physical therapists, and nursing professionals were recorded. The difference in scores between the periods was minimal as the value between the means and medians was less than one point.
Regarding neonatal care variables, there was a significant increase in the number of transfers of newborns to the local reference intensive care unit (ICU) and the capital of the state of Piauí. The municipal ICU in CIAMCA, located in Teresina, registered a 100% increase in admissions as it is the neonatal reference unit in the state capital for newborns in the southwestern mesoregion of Piauí. The city of Corrente, located at the border with the state of Bahia, recorded three admissions in the city of Barreiras in Bahia. The city of Floriano, the closest reference to the other cities in the mesoregion, also registered a significant increase in admissions (78.57%) (Supplementary Table S2).
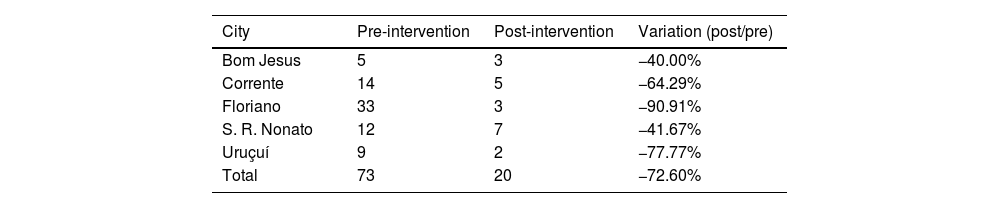
Using the registered delivery room deaths in the five study sites at the pre-intervention assessment and spreadsheets organized by the researcher for the registration of deaths at the post-intervention assessment, a comparison of the absolute and relative frequency of delivery room deaths in the southwestern mesoregion of Piauí was established. A 72.60% reduction in delivery room mortality was registered in the southwestern mesoregion of Piauí. The city of Floriano registered the highest reduction (90.91%), whereas the city of Bom Jesus registered the lowest reduction (40.00%) (Table 2). During this period, 479 newborns were resuscitated, of whom 414 (86.43%) were ≥34 weeks old, and 459 were registered as survivors.
Absolute and relative frequency of delivery room deaths during the 12-month pre- and post-intervention periods of the study.
| City | Pre-intervention | Post-intervention | Variation (post/pre) |
|---|---|---|---|
| Bom Jesus | 5 | 3 | −40.00% |
| Corrente | 14 | 5 | −64.29% |
| Floriano | 33 | 3 | −90.91% |
| S. R. Nonato | 12 | 7 | −41.67% |
| Uruçuí | 9 | 2 | −77.77% |
| Total | 73 | 20 | −72.60% |
S.R., São Raimundo.
The results of this study indicate that a model of neonatal care can be implemented to drive an improvement in the structuring of delivery rooms and the performance of healthcare professionals involved, even in places with high socioeconomic vulnerability. Some countries indicated by the World Health Organization as having the highest neonatal mortality rate in the world, all located in Africa and South Asia, have previously recorded some interventional studies and governmental actions aimed at reducing maternal–infant mortality.5,24–29
This study involved the training of 431 healthcare professionals through 700 training courses in a Brazilian state with one of the highest rates of early neonatal mortality in the country. It is important to highlight the change in the structure of delivery rooms after the intervention. All five cities subsequently acquired 100% of the fundamental items for newborn resuscitation. In addition to the fundamental items, all sites registered significant improvements, such as the regional hospital in the city of Uruçuí, which had only 18.1% of the materials cited in Ordinance 371 at the pre-intervention period and had 81.8% of the materials at the end of training, an improvement of 63.7%. Similarly, improvements were registered in Corrente (60.6%), Bom Jesus (54.6%), São Raimundo Nonato (51.5%), and Floriano (30.4%). The improvement results remained significant even 12 months after the intervention. This study highlights the teams’ care in constructing and maintaining the golden minute, which is the most important period after the birth of a newborn.
At the five study sites, managers from administrative and financial departments participated in meetings and discussions regarding neonatal care. Thus, through resources granted by the management of the regional hospitals, in addition to the release of materials by the Health Department of the State of Piauí (SESAPI; Piauí Health Secretariat), at the end of each stage of the intervention, the delivery rooms were organized by the training participants. The participation of all the healthcare professionals, together with local managers in the structuring of the delivery rooms, resulted in effective team motivation.
The results obtained in the structuring of research sites showed that implementation of the PRN-SBP through team training can directly influence the improvement of hospital management for newborn care, showing the need for a fundamental organizational model for newborn resuscitation in the delivery room. Analysis of the performance of the 431 healthcare professionals showed satisfactory acquisition of knowledge related to neonatal resuscitation and high-risk transportation, in addition to specific knowledge related to premature newborns born at <34 weeks. Knowledge acquisition proved to be even more significant 12 months after the intervention with the evaluation of a group of 167 healthcare professionals who attended the course on the resuscitation of ≥34-week-old newborns. In this sample, the difference between the periods was minimal, because the value between the means and medians was not higher than one point, showing a satisfactory retention of knowledge over the 12 months following the intervention. Therefore, the PRN-SBP methodology of using theoretical and practical courses has the potential to improve healthcare professionals’ knowledge regarding neonatal resuscitation and transport, promoting better care for newborns at birth in terms of both stabilizations after resuscitation and high-risk transport.
The improved delivery room structure, better knowledge retention of the trained healthcare professionals, and increased motivation of the teams seem to have directly contributed to the reduction of neonatal mortality in the study region. Although there is no record of the number of newborns resuscitated at the study site in the pre-intervention period, the researchers believe that the extremely precarious structure, non-compliances recorded, and health teams’ scarce knowledge of neonatal resuscitation would have resulted in the impossibility of appropriate resuscitation of a newborn. One of the most relevant oversights the researcher observed was the absence of an auto-inflatable balloon in 80% of the places studied during the pre-intervention period, which meant that it was impossible to perform positive airway pressure (PAP) on newborns with poor vitality at birth, a fact that may have contributed to an increase in neonatal mortality. Soon after the implementation of a neonatal care model in the region through the PRN-SBP, a considerable increase in appropriate neonatal resuscitations likely occurred at the study sites. Although it is impossible to establish a comparison between the two periods mentioned, the registration of 479 resuscitations in the post-intervention period, with 414 ≥34-week-old newborns (86.43%) and 65 premature newborns <34 weeks old (13.57%) may have contributed to the reduction in neonatal mortality in the region.
The assessment of records made by nursing teams during the pre-intervention period and spreadsheets prepared by the researcher, which the teams filled out at the post-intervention period, showed a 72.60% reduction in delivery room mortality. The post-intervention records showed that the practice of PAP, which was not previously practiced in four of the five cities, became a frequent procedure used for newborns with compromised vitality at birth. PAP practice is a crucial factor in reducing documented deaths.
The admission of resuscitated newborns in the five study sites at neonatal intensive care units (NICUs) in the state and in neighboring regions strongly corroborates the evidence of reduction of delivery room mortality rate after the intervention, considering that an expressive increase in admissions was recorded 12 months after the study, with emphasis on the CIAMCA municipal NICU, which recorded a 100% increase in admissions. It is likely that this increase also proves the improvement in the quality of high-risk transport of the population studied.
The presence of a nursing professional trained in neonatal resuscitation and at least one physician on call throughout 24 h—thus following the PRN-SBP recommendation of a minimum team of 2–3 healthcare professionals trained and able to resuscitate an RN quickly and effectively—was achieved.
The regulation of compliance with the guidelines commenced in the five health regions of Piauí only after the execution of this interventional study, proving the ability to modify neonatal outcomes via the implementation of the PRN-SBP in Brazilian maternity hospitals.
Numerous discussions involving all governmental levels are required for a more accurate assessment of the factors related to difficulties in the management of newborn care at delivery rooms in more critical regions of the country. This study proves the efficiency of the PRN-SBP instructors’ dissemination of knowledge for the best practice of newborn care and may also contribute directly to the structural organization of Brazilian maternity services. This type of action may soon reverse the current neonatal mortality rates observed in remote regions through the implementation of a model aimed at improving Brazilian neonatal outcomes.
In conclusion, the intervention involving the training of healthcare professionals in the region through the PRN-SBP promoted significant advances in neonatal outcomes by improving the structure of delivery rooms and the knowledge of neonatal resuscitation of professionals involved in neonatal care. The achieved actions contributed to the advancement inequity of healthcare by improving neonatal survival as there was a proven reduction of deaths in delivery rooms in the region, despite a significant increase in ICU admissions. This study, which was implemented in a region of high socioeconomic vulnerability in Brazil and demonstrated a significant improvement in neonatal outcomes, may serve as a model for implementation in other less economically stable regions of the country, especially in more remote regions, where mortality rates remain alarming.
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors would like to thank the Piauí State Department of Health Neonatal Resuscitation Program of the Brazilian Society of Pediatrics and Campinas State University for their aid in implementing this study.