To review the literature about the environmental impact on children's mental, behavior, and neurodevelopmental disorders.
Sources of dataA nonsystematic review of papers published on MEDLINE-PubMed was carried out using the terms environment and mental health or psychiatric disorders or neurodevelopmental disorders.
Summary of findingsPsychopathology emerges at different developmental times as the outcome of complex interactions between nature and nurture and may impact each person in different ways throughout childhood and determine adult outcomes. Mental health is intertwined with physical health and is strongly influenced by cultural, social and economic factors. The worldwide prevalence of psychiatric disorders in children and adolescents is 13.4%, and the most frequent are anxiety, disruptive behavior disorders, attention deficit hyperactivity disorder and depression. Neurodevelopment begins at the embryonic stage and continues through adulthood with genetic differences, environmental exposure, and developmental timing acting synergistically and contingently. Early life experiences have been linked to a dysregulation of the neuroendocrine-immune circuitry which results in alterations of the brain during sensitive periods. Also, the environment may trigger modifications on the epigenome of the differentiating cell, leading to changes in the structure and function of the organs. Over 200 million children under 5 years are not fulfilling their developmental potential due to the exposure to multiple risk factors, including poverty, malnutrition and unsafe home environments.
ConclusionsContinued support for the promotion of a protective environment that comprises effective parent-child interactions is key in minimizing the effects of neurodevelopmental disorders throughout the lifetime.
According to the World Health Organization (WHO) there is no health without mental health. Mental health is an essential component of general health and wellbeing. On the other hand, psychopathology emerges at different developmental stages and as the outcome of the complex interactions between nature and nurture and may impact each person in different ways throughout childhood and determine adult outcomes.1
A meta-analysis of 41 studies conducted between 1985 and 2012 estimated that the worldwide prevalence of psychiatric disorders in children and adolescents was 13.4% and that the most frequent disorders were: anxiety disorders (affecting 6.5%); disruptive behavior disorders (5.7%); attention deficit hyperactivity disorder (ADHD) (3.4%); and depressive disorder (2.6%).2 These numbers are even higher when the authors consider the prevalence of children who do not meet the full diagnostic criteria for a disorder but who present clinical symptoms, with an estimated prevalence of 26% of children.3
Psychiatric disorders have also been described as mental, behavior and/or neurodevelopmental disorders (MBDDs) and many studies have reported that they are very frequent. Most of them start early in life. For example, a nationally representative study in the USA reported that 17.4% of children aged 2–8 years had a psychiatric diagnosis.4 The largest metanalysis on the age of onset of psychiatric disorders found that the onset of a first mental disorder occurs before age 14 in one-third of individuals with autism spectrum disorder (ASD) emerging in infancy, while ADHD emerges in preschool years. In contrast, anxiety disorders emerge in childhood and peak in early adolescence, with separation anxiety emerging before generalized anxiety.5
In Brazil, a recent study assessed a representative sample of 4 to 5-year-old children in Embu das Artes, São Paulo, and found that at least 25% of the preschool children presented psychiatric symptoms. Additionally, children with mental, behavioral and/or neurodevelopmental disorders (MBDD) in this sample faced higher parental stress, parental psychopathology (i.e. anxiety and/or depression), and lower social capital, when compared to children without these disorders.6
Many studies have also reported that the prevalence rates varied according to the social and environmental conditions in which children lived. For instance, estimates of mental, behavior and/or neurodevelopmental disorders ranged from 13.9% among children in the highest income levels to 22.1% among those in the lowest income levels. Other factors that increased the prevalence rates were: having a parent with a psychiatric disorder; parents with financial and/or employment problems; lack of access to health services; lack of family/and/or neighborhood support; and living in a neighborhood with limited social resources (such as sidewalks, parks, community centers, or libraries.4
Decades of epidemiological, clinical, developmental, and basic research studies have demonstrated that the environment has a strong impact on the physical, cognitive, social, and emotional development as well as on the mental health of all individuals throughout their lifetime. Advances in understanding the environmental risk and protective factors for mental health have caused a significant paradigm shift transposing the old nature-nurture question to a nonlinear, multisystemic, dialectic model, where nature and nurture mutually contribute to one another.7
The main objective of this article was to review and describe the main findings of the literature about the environmental impact on the neurodevelopmental disorders during childhood
The bioecological modelAccording to the WHO over 200 million children under five years are not fulfilling their developmental potential due to the exposure to multiple risk factors, including poverty, malnutrition and unsafe home environments.8
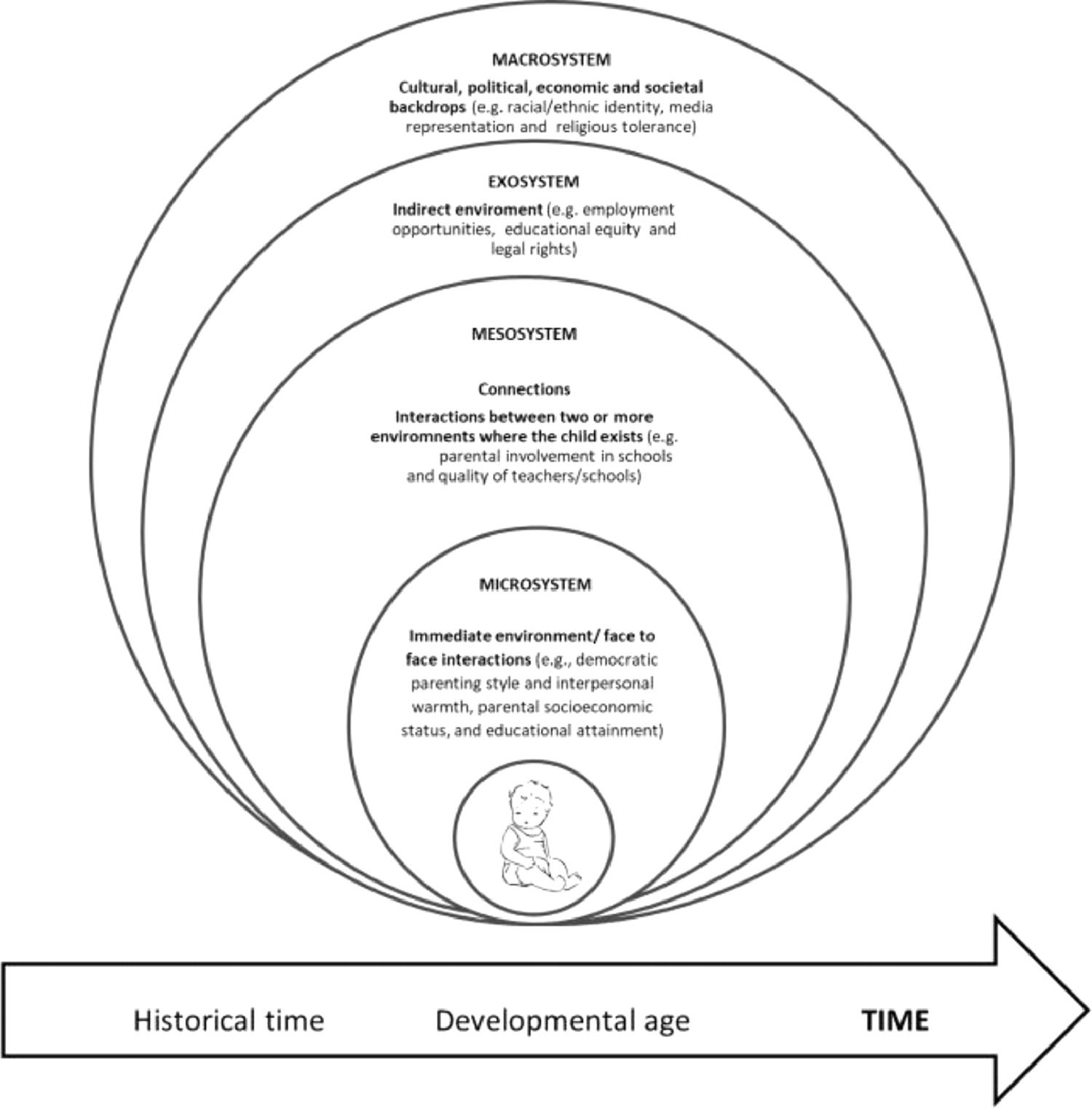
In the bioecological model proposed by Bronfenbrenner, the environment where a child lives are dynamic and composed of systems classified according to the proximity with the child, one influencing and being influenced by the others. In this “ecological environment” children have an active role in their own developmental process and some characteristics will influence their development.9Figure 1 presents a simplified version of Bronfenbrenner's model that exemplifies the importance of the different contexts in the child's development. For instance, the child lives in a family that functions in a society and it is essential that the families are supported by the community to provide effective nurturing care. Also, individual attributes (i.e., temperament, intelligence, problem-solving skills, emotional regulation, verbal communication, social skills, empathy, self-confidence, positive ethnic identity, religiosity and educational commitment) are interconnected with environmental factors such as social and economic status.
Very early life exposure to environmental factorsThe prenatal environment may trigger modifications on the epigenome of the differentiating cell, leading to changes in the structure and function of the organs. For instance, poor fetal growth is an important marker of an adverse intrauterine environment and has been associated with increased risks for developmental delays and/or psychiatric disorders. Maternal factors such as the mother´s age, socio-economic status, maternal physical and mental health, and substance abuse can affect fetal growth.10
Prematurity is an adverse event that contributes to poor socioemotional development. The premature brain may present with dysmaturational disturbances such as changes in synaptic efficacy, loss of volume, enlarged ventricles, and alterations in myelination.11 The effects of prematurity are seen in all gestational age subgroups but a meta-analysis demonstrated that extremely low birth weight children have a more robust association with inattention, hyperactivity, and internalizing problems in childhood and adolescence and higher rates of social problems, depression, and anxiety in adulthood.12 Additionally, premature children have higher rates of emotional and behavioral problems at school entry and even preschoolers with a history of prematurity showed a twice higher chance to be above international cutoffs in a social-emotional screening instrument (the Ages and Stages Questionnaire–Social Emotional) in an epidemiological sample of an urban setting in Brazil.13
Intrauterine exposition to substance abuse, smoking, maternal psychological stress, and/or parental psychiatric disorders during pregnancy may have a strong negative impact not only during pregnancy but throughout a lifetime. For instance, intrauterine substance abuse or exposure to tobacco can affect gene expression of selected fetal brain regulatory genes responsible for brain growth, myelination, and neuronal migration, altering brain structure and function. Prenatal smoking has been associated with a greater risk for bipolar disorder, ADHD, depression, and addiction in later life.14
Prenatal maternal anxiety increases fetal exposure to maternal cortisol. This exposure affects offspring neurodevelopment involving the amygdala, pre-frontal cortex, and hypothalamic-pituitary-adrenal axis which can increase the risk for behavioral and mental health problems later in life.15
The exposure to high rates of air pollution during pregnancy has been associated with changes in both global and locus-specific DNA methylation and with telomere length shortening. Also, low-dose exposure to chemicals during pregnancy and/or early childhood has a greater impact on health than high-dose exposures to the same chemicals during adulthood. Examples of chemicals qualified as toxic include organophosphate pesticides, polychlorinated biphenyls, phenols (including bisphenol A), phthalates and certain metals.16
The first face-to-face interactions between the child and his/her main caregiversTo reach their full potential, children need to experience the five inter-related and indivisible components of nurturing care: good health, adequate nutrition, safety and security, responsive caregiving, and opportunities for learning. Nurturing care may reduce the detrimental effects of social disadvantage on brain structure and function which, in turn, improves children's health and development.17
Nurturing care and support from adult caregivers are essential for human infants’ survival. Since Bowlby's studies, it has been well established that infants develop bonds or attachments that play a key role in normal development and that a secure attachments with caretakers improves the capacity of emotional connectivity, the ability to build safe and secure relationships, and the development of positive self-esteem later in life.18 On the contrary, a meta-analysis involving more than 5,000 individuals found a significant association between insecure attachment and externalizing problems (i.e. hyperactivity and/or aggression), with larger effects on boys.19
The English and Romanian Adoptees’ studies followed children adopted by families in the United Kingdom after living in Romanian orphanages during the Ceausescu regime. Initial reports documented a pervasive effect of deprivation on cognitive and social development for most children that were recovered up to the age of 6 years. However, children who spent more than six months in Romanian institutions subsequently displayed a severe and highly impairing combination of higher symptom rates of neurodevelopmental disorders, including ADHD, ASD, and a pattern of indiscriminate friendliness towards strangers and lack of selectivity in attachment-related behaviors which persisted until young adulthood.20
More recently, the research on attachment has linked the consequences of an insecure attachment with other mediating factors, such as self-regulation skills. Self-regulation can be defined as the ability to adjust personal behaviors by controlling thoughts, feelings, impulses, and performance in order to achieve specific goals.21 The development of self-regulation abilities is heavily dependent on parent-child interactions and on attachment style. Insecure attachment reduces the child's effort to self-regulate in a coherent and flexible manner. Furthermore, self-regulation difficulties have been associated with teenage pregnancy, drug addiction, educational failure, domestic violence, depression, anxiety, and stress.21
Additionally, the child's wellbeing is closely linked to his/her caregivers’ mental health. Parental mental health acts as a buffer or protective factor from adversities and promotes early childhood development. On the contrary, having a parent with a psychiatric disorder, such as depression, is a strong risk factor for disruptive and/or depressive disorders in their offspring.22 A recent population-based cross-sectional study of 3,566 children aged 0−66 months conducted in Ceará, Brazil, found a 8.4% prevalence of mother's psychiatric disorder and an association of these diagnoses with lower child development scores.23
Chang at al. (2007) accompanied for ten years a cohort and observed that the adverse effects of maternal depression on their children were also affected by other variables such as the child's age, sex and race/ethnicity; the maternal educational level and age at childbirth; the number of children; poverty status; urban residence; and father's residential status.
The above studies reinforce the need to study individual trajectories over time and the relevance of implementing preventing interventions from improving the quality of the caregiver-child interaction.
In this context, the American Academy of Pediatrics highlights the importance of assessing the mental health and adjustment to parenting. For instance, perinatal depression is a depressive disorder with an episode occurring during pregnancy or within the first year after the child´s birth. Overall prevalence is 12% but these rates are higher for women with low income (25% prevalence), and for low-income adolescent mothers (40%-60%). Therefore, recommendations include screening for perinatal depression during the well-infant visits at 1, 2, 4, and 6 months of all new parents, regardless of gender or marital status, and making appropriate referrals for needed care.24
The family environment has a major impact on children's development since parents are the most enduring influence in children's lives and child-rearing methods can significantly affect the incidence of children's externalizing (e.g., hyperactivity, rule-breaking behaviors, and/or aggression) and internalizing (e.g., anxiety, withdrawal, and/or depression) symptoms.25 Child-rearing methods are also called “parenting styles” and can be defined as a constellation of parental attitudes and behaviors towards children or as the context that moderates the influence of specific parenting practices on the child.26 Parental styles can be classified as:
- •
Authoritarian: characterized by high demandingness and low responsiveness, firmly enforced rules, and strong control over children's autonomy.
- •
Permissive: has low demands and high responsiveness, lack of monitoring, control, and discipline, yet it is warm and nurturing.
- •
Neglective: low in both responsiveness and demandingness.
- •
Overprotective: low demandingness and interference on the gradual development of independence and self-sufficiency.
- •
Authoritative: parents are demanding and responsive allowing children to develop autonomy by providing not only support and warmth, but also clearly defined rules and consistent discipline.
Although the authoritative parental style has been demonstrated to be the optimal parenting style and related to positive child outcomes such as self-reliance and adjustment, parents can shift from one parenting style to another in different situations.26 For instance, the ways parents interact with their children are strongly influenced by stressors. Parental stress is a multidimensional concept that is cumulative, highly influenced by the environment, and can be classified according to three domains: parental, child, and contextual domains.27 Parents of premature children or with a history of adverse events in the neonatal period or with chronic diseases have a higher incidence of stress.12,27
Low income can also affect children by limiting material resources or by increasing familial interpersonal distress. Parents facing economic problems are at an increased risk for emotional distress (e.g., depression, anxiety, anger) and consequently increased conflict between caretakers, which, in turn, disrupts supportive parenting. These disruptions in the relationships can lead to a higher frequency of parenting behaviors marked by hostility, irritability, rejection, coercion, or inconsistent and explosive discipline behaviors.28
All the above studies reinforce the need for developing and implementing interventions that empower the parents as promoters of the integral development of their children, that reduce their stress and psychopathological symptom scores. It is important to encourage the participation of pediatricians and other health and education professionals in the screening of these potential risk factors and also on activities to provide support for the parents and to identify children's difficulties and potentialities.
Impact of the mesosystem, exosystem and macrosystemChildren are exposed not only to the parental influence but also to the experiences provided by other family members, friends, teachers, peers, community members and social institutions.
The exposure to the student-teacher and student-peer relationships has been associated with long-term academic and behavioral functioning. Negative experiences with peers (such as rejection, neglect and lack of friends during elementary school have been associated with higher levels of loneliness, negative self-esteem, depression, anxiety, school avoidance and antisocial behaviors.29
The exposure to some factors defined as Adverse Childhood Experiences (ACEs) has been associated with deleterious effects on child development. This term was initially used in a study that investigated the impact of childhood abuse and neglect and household challenges on later health and wellbeing outcomes. The original study investigated personal (i.e., physical abuse, verbal abuse, sexual abuse, physical and emotional neglect) and familial (i.e., an alcoholic parent, domestic violence, a family member in jail or diagnosed with a mental illness, and the absence of a parent due to divorce, death, or abandonment) traumatic types.30
Study findings described not only that childhood trauma was very common but showed that as the number of ACEs increases so does the risk for negative health and wellbeing outcomes in adulthood. There was a direct link between childhood trauma and adult onset of depression, suicide, being violent, and/or being a victim of violence.30 It is important to mention that approximately one-third of all mental disorders worldwide are attributable to exposure to Adverse Childhood Experiences.31
A more recent approach investigated the impact of early life adversities. They are defined as experiences that require significant adaptation by the developing child in terms of psychological, social and neurodevelopmental systems and which are outside of the expected normal environment.32
Early life adversities have been linked to a dysregulation of the neuroendocrine-immune circuitry, which results in alterations of the brain and/or other organ systems during sensitive periods of development.33 Examples of adversities that are associated with low-socioeconomical status comprise of material deprivation (varying from the lack of opportunities to have a cognitively enriched environment in the form of toys and books to the quality and quantity of early educational opportunities); a less complex language environment; psychosocial stress (that can be associated with interpersonal violence, crowding or neighborhood violence) and more frequent exposure to toxic chemicals such as tobacco smoke.34
The adverse effect of poverty is better understood using a multidimensional approach such as the Child Well-Being Index created by UNICEF that uses factors related to child income poverty/monetary deprivation, health and safety, educational, peer and family relationships, housing and environment. Pickett et al. compared rates of childhood wellbeing in wealthy countries and showed that wellbeing was lower where child poverty rates were higher. However, child poverty rates were highly correlated with the degree of income inequality, concluding that a child's well-being is highly dependent on the reductions in inequality.35
In Brazil, a UNICEF publication showed that, despite important changes over the last decades, 27 million children and adolescents still experience multiple deprivations and that 10,2 million children experience extreme deprivations. Of these, 18 and 10,2 million, respectively, are black.36 These data probably are worse after the COVID-19 pandemic since many families had a significant decrease in their family income during the pandemic period.
Neuroscience of the environmental impact on child's developmentNeurodevelopment begins at the embryonic stage and continues through adulthood. The brain is the primary organ of stress and adaptation, responsible for interpreting and regulating behavioral, neuroendocrine, autonomic, and immunological responses to the events (adverse or protective), changing structurally and functionally in response to significant adversity or to positive experiences. The interconnection between these experiences and the individual responses to them during the first years of life will be the foundation for all the future developmental processes.37
The early childhood brain is extremely plastic, but this enhanced plasticity also provides an enhanced vulnerability to all types of experiences. The nature and timing of these experiences influence the course of the developing brain in many ways, especially if they occur during the “sensitive or critical periods”. Sensitive periods may be defined as restricted windows of development when experiences have strong influences on the neural circuit formation. The critical periods represent a short and sharply defined window of opportunity during which the exposure to environmental input causes irreversible changes in brain function and structure.37
During early childhood, there are cascades of these sensitive periods for specific complex developmental domains.38 Identifying these periods is key to understanding how the timing of environmental events may increase the risk for aberrant development.
Research with rodents and nonhuman primates has demonstrated that the effects of adverse experiences target brain structures that are intimately involved in physiological stress and behavior, such as the amygdala, prefrontal cortex, and hippocampus.39
To better understand how the type and the timing of environmental experiences influence the brain is essential to understand the two different contexts in which neuroplasticity occurs:
- •
Experience-expectant: the brain has developed through evolution to “expect” some early stimulating experiences and uses them to shape neuronal responses. For instance, healthy infants need visual input to develop the visual system, and infants who fail to receive such an input develop permanent blindness (i.e., infants with congenital cataracts)
- •
Experience-dependent: this definition of neuroplasticity states that exposure to different experiences can yield different developmental outcomes. For instance, studies have shown that infants whose mothers suffer from post-partum depression have more difficulty in recognizing emotional expressions than infants whose mothers are not depressed, probably because depressed mothers express a smaller number of different facial expressions.40
In a series of studies with non-human primates, infants were separated from their mothers at an early age and reared in isolation or with peers. These separated animals exhibited symptoms of depression and motor stereotypies, tended to be anxious, impulsive, and displayed abnormal stress responses when adults. However, animals reared with peers appeared to reverse many of the negative effects of the early maternal separation.39
Below the authors present a summary of three different ways in which the powerful and complex interplay between genes and the environment may happen.15
- Gene-environment correlations: in this case, genes that influence a trait also influence the exposure to environmental risk. For instance, a mother with high anxiety levels will also display anxious behaviors at home, which will ultimately influence the child
- Genotype–environment interactions: occur when the person's genotype has an effect on the response to environmental factors. Therefore, individuals with a “sensitive” gene polymorphism will be at a higher risk if exposed to a predisposing environment than individuals with an “insensitive” gene polymorphism. For example, individuals with at least one copy of the short allele of the promoter region of the serotonin transporter (5-HTT) gene polymorphism (in contrast with people with too long alleles) were more likely to be diagnosed with depression. Furthermore, when children (with 52 months) had short 5-HTT allele and their mothers had a low responsive care, they were less competent in academic skills, school engagement and social functioning with peers than children whose mothers had a more responsive care.41 Interestingly, good maternal responsiveness had no effect on children with two long alleles.41
- Epigenetic gene-regulatory processes: early life experiences can modify the chromatin function affecting gene expression. One way for this to happen is through DNA methylation that functions as a molecular memory of each individual environment. As an example, maternal smoking during pregnancy influences differences in DNA methylation at birth with effects that can persist during the whole life and can also have potential transgenerational effects.14
A balanced approach to understanding how genes and environmental conditions interact, focus on the study of resilience and risk factors considering that genetic differences, environmental exposure, and developmental timing act synergistically and contingently. In this context, good health is a result of the interactions between key protective and risk influences during critical or sensitive developmental stages.
When there is a balance between protective and risk factors there is a healthy neurodevelopmental pathway. On the contrary, when there are delays or deviations on these neurodevelopmental pathways the person has a much higher chance of having a neurodevelopmental disorder, which may start presenting the symptoms in the first childhood years or much later in life.34
The co-occurrence of risk and protective factors entangle the identification of the specific elements responsible for the onset and continuity of mental health problems. Distal factors (i.e., non-specific factors that affect the likelihood of subsequent risks) work together with proximal causes through a probabilistic model that is conditioned by issues such as intensity, context, and timing.1 Therefore, no developmental influence, whether biological or environmental, should be regarded as rigidly deterministic.
There is a series of evidence-based interventions focused on nurturing care that was tailored for high-risk children because of low socioeconomic status and limited stimulation at home or children with neurodevelopmental disorders or preterm birth. These interventions are based on the power of parental support programs that promote nurturing care, particularly those employing several behavioral change techniques.42
A metanalysis that assessed the effectiveness of behavioral and cognitive-behavioral group-based parenting programs for improving child conduct problems, parental mental health and parenting skills found significant improvements in parental mental health and positive parenting skills. Parent training also produced a statistically significant reduction in negative or harsh parenting practices.43
Neurodevelopmental disorders with early onsets tend to be more severe, particularly if not identified and treated early. Therefore, screening tools and early interventions may allow more effective healthcare, education and social pathways by taking action before health problems worsen or by preventing their onset and reducing developmental inequities.44 Also, it is important that interventions in early childhood also include strategies to reduce social inequality. These programs can lead to higher levels of human capital and social mobility and they have economic advantages since the return for investment in early childhood is much greater than the investment at later ages.35
ConclusionsA robust body of evidence confirms the significance of the quality of childhood experiences on lifelong health. These experiences occur in multiple systems that are strongly influenced by risk and protective factors, such as cultural, social and economic factors, ethnic identity, parental and social support.
All parents are capable of promoting their children's integral development since they have the adequate social conditions to thrive. It is important to recognize that continued support for the promotion of a protective environment that comprises effective parent-child interaction is key to minimizing the effects of neurodevelopmental disorders over early childhood.