To describe the consequences of social inequalities on children's health as a global and persistent problem, demonstrating its historical and structural roots in different societies.
Data sourcesRelevant articles in the PubMed/MEDLINE database, in addition to those found in a manual search and in the bibliographic references of selected studies and consultation to the websites of international organizations to obtain relevant data and documents.
Data synthesisTo understand how inequities affect health, it is necessary to know the unequal distribution of their social determinants among population groups. In the case of children, the parental pathway of determinants is central. The non-equitable way in which many families or social groups live, determined by social and economic inequalities, produces unequal health outcomes, particularly for children. This is observed between and within countries. Children from the most vulnerable population groups consistently have worse health conditions. Interventions aimed at children's health must go beyond care and act in an integrated manner on poverty and on social and economic inequalities, aiming to end systematic and unfair differences.
ConclusionsDespite the considerable advances observed in children's health in recent decades at a global level, the inequalities measured by different indicators show that they persist. This scenario deserves attention from researchers and decision-makers, especially in the context of the global health crisis caused by the COVID-19 pandemic, which has further intensified the situation of vulnerability and social inequalities in health around the world.
In the history of human societies, the existing differences between individuals or between the groups that make them up are persistent characteristics or even worsening ones. In this context, the importance of the differences generated by the unequal access to and distribution of what society produces and by the ways in which different groups relate to each other is emphasized. Thus, while a small portion of the population concentrates a large part of what is produced or of the mechanisms of power, the majority has to accept a smaller part. Then, inequities are established, as asymmetrical accesses and relationships are defined regarding the fruits of collective efforts. These inequities are transmitted through generations, existing at present and having existed in the most diverse historical moments of humanity.1 While economic inequalities has been essential to explain these inequities, more recent analyses emphasize the importance of other factors, particularly the-racial and gender issues.2
Inequalities and inequities, material or non-material, verified in different spheres of life in different societies, are frequently observed and registered due to their effects on the health of individuals and populations. Inequalities, in theirdifferent forms, will be expressed as what has been called the social determinants of health. These determinants are expressed not only in the material world (housing, sanitation, transportation, access to adequate food, access to health services, education, etc.) but also in the immaterial relationships that are established between individuals and social groups and that generate ways of oppression and psychosocial suffering.3
It is not by chance that the observed health inequalities have been consistently related to those seen in other planes of social life. Therefore, the most different health problems, whether infectious, chronic, mental, violence, etc., consistently occur with greater frequency among the most vulnerable groups in any society, even in the wealthiest ones. The effects can be seen at all stages of the life cycle, from birth to death. However, children, due to their characteristics, constitute a sensitive group that is also vulnerable to social adversities that affect their health and development.
Brazil is a country characterized by its high degree of inequalities, which places it among the most unequal countries on the planet.4 The effects of these inequalities on the living conditions of the vast majority of the Brazilian population are striking, as are their effects on health,5 whether of the population in general or of children, in particular.6
The aim of this article study to describe the consequences of social inequalities on children's health as a global problem that afflicts populations not only in poor countries, but also in wealthyones, where its persistence demonstrates the historical and structural roots of this problem. Although related, it differs from the discussion on poverty and health.7 Poverty refers to absolute deprivation and manifests itself through hunger and malnutrition, limited access to education and other basic services, discrimination and social exclusion, as well as lack of participation in decision-making instances. In turn, inequality is a relational concept and refers to the existence of unfair differences between individuals and social groups, even without the existence of poverty, as it occurs in some wealthy societies. It is certainly one of the most relevant problems in the field of population health at a global level, being an enormous challenge for all who seek to develop solutions.
Social inequalities and health inequalitiesDifferences in health levels between individuals and population groups are observedin any society. This can occur due to factors such as genetic variations, aging, gender-related biological issues, among others. However, the variations or differences in health may not be random or generated by purely biological factors. Therefore, when they are systematic, presenting consistent patterns in their distribution, and when they are socially produced, constituting unfair differences, which are generated and maintained by unfair models of social organization, such “differences” are, in fact, health “inequities”.3
Health inequities are, therefore, generated by socioeconomic and environmental factors and by lifestyles, influenced by the social structure, and, in principle, subject to change. In the opposite sense, health equity is related to the idea of justice, in which all people could reach their full health potential, and no one should be harmed by their social position or other socially determined reason.3 The concept of equity includes the idea of need, assuming that there are different individual needs and resources should be shared accordingly.3,5
Prejudice and racial discrimination are examples of factors that lead to unfair differences in access to health resources and opportunities between different groups. There is evidence of how black people have a worse health situation than white people, from birth to death.8,9 Gender inequalities are also able to cause unfair health situations and are well documented in the scientific literature.10 In addition, it has been conclusively demonstrated how material circumstances in general – such as educational disadvantage, poverty, and poor working conditions – can increase the chances of illness and death.11
Access to health services can also be hindered by social inequities. This is of fundamental importance since, without effective health care that provides health prevention and promotion and treatment of diseases, all other human activities are affected.3 There are three types of barriers to health service access: geographic access barriers, when the location of the service is worse in less favored regions; economic access barriers, related to the high amounts charged for services unavailable in the public system; and finally, cultural access barriers, related to inadequate treatment offered to socially vulnerable groups by health professionals, interfering with the quality of care.3
Health inequities occur from a global perspective, affecting all human societies, but they are not always considered unfair and subject to global political actions.1 Global health inequities maintain the historical conditions of disadvantage among more favored regions of the world, where, for instance, infant mortality is a very rare condition, and the poorest regions, where it is still an alarming problem.12
To change this reality, policies that aim to eliminate all systematic differences in health between population groups are required, considering their different needs. However, it is necessary that actions be focused not only on the most vulnerable groups but aims at reducing health differences between the more and the less privileged, always seeking to increase the improvement of the health status without reducing the general level. The social determinants of health that influence the emergence of inequities should receive special attention from political strategies, which are built on the principles of equity.
Child health and its determinantsSince before birth, children whose parents live in a situation of socioeconomic vulnerability may have worse health conditions than those who live in better circumstances.13 The ways in which living conditions affect children's health are complex and are driven by social inequities, that is, by the unequal and unfair distribution of power and resources, which determine the circumstances in which children will grow up.
To understand how inequities affect a population's health, it is necessary to understand their determinants, that is, the conditions under which people are born, grow, work and live, and take into account the unequal distribution of these determinants among population groups.14 In the case of children, it is essential to consider the parental pathway of social determinants, as they depend on the accountable adults to survive.
A model of the social determinants of child health is shown in Figure 1, with health outcomes resulting from the interrelationship of factors at different levels.15,16 The model starts with the health outcomes, directly influenced by the biological conditions of the child (gender, congenital anomalies) and of the mother (multiple pregnancy, previous pregnancies) and, based on that, other levels that can be modifiable are described. The next level, the intermediate one, shows elements that mediate the relationship between structural factors and health outcomes, consisting of material and non-material circumstances.
Among the material circumstances, we can highlight the example of inadequate housing regarding size and conditions, characterized by overcrowding and lack of sanitation, risk environments for diarrhea, respiratory problems, and other communicable (infectious) diseases.17 Families living in poverty may not have the resources to purchase hygiene products, medicines, or food, or when they obtain the latter, they are of low nutritional quality.7 Occupations that do not guarantee basic rights such as maternity leave or parental leave when the child becomes ill make child care insufficient and expose them to adverse conditions.7,13
Among the non-material factors are the mental health of caregivers, their health behaviors, parenting, and social cohesion. The caregivers'mental health is an important determinant, as it can affect the child's physical and mental health through two ways: when negative feelings generated by inequity affect the neuroendocrine pathways, harming them;18,19 or when stressors generated in contexts of social inequality influence health behaviors.13
As they do not yet have control over the decisions, or the developed behaviors themselves, the child depends on the caregivers' health behaviors. The choice of less healthy foods, smoking, poor knowledge about the importance of immunization, and not adopting practices to prevent diseases and promote health may be more common in more vulnerable groups.20 Moreover, the late decision to seek health services by guardians and poor adherence to the recommended treatment for the child isassociated with the socioeconomic status and can increase the risk of death or aggravate existing diseases.21,22
Parenting, which concerns the care activities performed by adults for the child's survival and full development, can result in inconsistent care under negative social circumstances.23 There is evidence that high depressive symptoms in mothers are associated with less childcare up to 12 months of life, more child hospitalizations, less positioning of the baby to sleep on the back, less updated vaccinations,24-26 early weaning27 and greater risk of malnutrition.18
Communities with weak social cohesion that is, without sufficient solidarity ties to form connections and support networks can negatively affect health.16 The relationships between the child's caregivers and the community have the potential to provide a supportive environment for healthy and positive parenting. Social cohesion can play a protective role in situations of neglect, being capable of meeting the child's basic needs.28
Child health is sensitive to several aspects related to health services, the last element at the intermediate level of the model. Poorer families may find worse access, such as geographic barriers, having to travel long distances, or economic barriers, when the service has some cost, or cultural when professionals are prejudiced against the caregivers/children.7 The unavailability of services such as prenatal consultations, childbirth care, or pediatrics, and/or inputs, such as medicines, vaccines, and nutritional supplements, may be greater where the poorest are treated.7 Worse organizational quality can also be found, such as a long waiting time for care, for instance.7
At the last level of the model are the structural factors, comprising the socioeconomic status of caregivers, transversally determined by social class, gender relations, and racism and influenced by culture, public, social and macroeconomic policies. As children do not have an occupation or income, they do not have a socioeconomic status but live under a socioeconomic circumstance provided by the status of the adults with whom they live.13
Structural factors determine the distribution of all resources at the intermediate level of the model. Racism, for example, has a strong influence over the entire chain of social determination, resulting in social inequities in child health. In Brazil, black, brown and indigenous mothers, for instance, have a lower frequency or late start of prenatal care and more difficulty in accessing care during childbirth when compared to white mothers.8,29,30 This results in a higher risk of low birth weight, being born small for gestational age or preterm birth, factors that increase the risk of infant mortality.8
Inequality can be observed even in a context of nutritional and epidemiological transition when determinants that did not seem to have such an influence on child health in contexts of greater poverty start to show prominence. For example, even with the reduction in the infant mortality rate, mainly due to causes related to poverty, black, brown, and indigenous children still suffer more hospitalizations due to infectious and parasitic diseases.31 Indigenous children are still more affected by malnutrition, although the rates of malnutrition are being replaced by an increase in overweight rates in the pediatric population in general.32 In addition, morbidity and mortality from chronic diseases, accidents, and violence are gaining prominence and should become the focus of health actions.33,34
Knowing in detail the pathways through which social determinants affect health is essential to identify how health inequities are produced and how they can be prevented.13 Associated with this idea, it is necessary to consider that none of these pathways overlaps the others.35 Social and health policies and actions, which are structural determinants of health, are essential to improve the living conditions of the most socioeconomically vulnerable populations and, consequently, to prevent and minimize negative outcomes in child health, reducing social inequities in health.
Child health problems: main indicators and new challenges in the context of the COVID-19 pandemicChild health problems are unevenly distributed across the world, with the worst levels consistently observed in the poorer regions. As they reveal levels of inequality and poverty, health indicators are also used to monitor social and economic development, as they are related to living conditions, food and nutrition security, and access to health services. Among the relevant and most frequently used indicators are: mortality rates in children under five years, infant and neonatal mortality rates, preterm birth and low birth weight, and measures of nutritional status, such as short stature or chronic malnutrition (stunting), acute malnutrition (wasting) and overweight.36
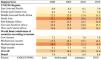
It is important to highlight the decline in under-5 mortality rates in all regions of the planet, with reductions of more than 40% between 1990 and 2019, although not all places have reached acceptable levels.37Figure 2 shows the rates of under-5, infant and neonatal mortality rates for 1990 and 2019.37 In 2019, the global under-5 mortality rate (38.0/1,000 live births) was still far above the target established for 2030 by the Sustainable Development Goals (SDGs) (25.0/1,000 live births).38 By geographic region, this rate varied considerably between the regions of the planet, reaching 96.8/1,000 live births in West and Central Africa vs. 6.3/1,000 live births in North America. This difference of approximately 15-fold in an important child health indicator is a strong expression of the high levels of global inequalities that exist worldwide.37 The same gap is observed when comparing the average under-5 mortality rate between low-income countries (67.6/1,000 live births) and high-income ones (average rate of 5.0/1,000 live births). Brazil has maintained average levels, expected for groups of upper-middle-income countries (13.9/1000 live births).37
When the analysis is performed by age subgroups, it is observed that the post-neonatal periods (28 days to 1 year) and 1 to 4 years are more vulnerable to the social and economic context, while in the neonatal period, they are more sensitive to the characteristics of the birth and the pregnancy.39 It is not an inadvertent fact that low-income countries havehigher average under-5 (67.6/1,000 live births) and infant (47.9/1,000 live births) mortality rates than the average neonatal mortality rate (26.6 / 1000 live births).37
Regarding the causes of death, disparities are also observed. Globally, the four leading causes of death among children in 2017 were preterm birth (6.9/1,000 live births), acute respiratory infections (5.8/1,000 live births), asphyxia, and trauma during childbirth (4.8/1,000 live births), and diarrheal diseases (3.0/1,000 live births). However, when analyzing the geographic regions, the African continent has the highest burden of death from each of these causes (reaching a mortality rate from preterm birth of 8.9/1,000 live births, from acute respiratory infections of 11.5/1,000 live births, due to asphyxia and trauma during childbirth of 8.9/1,000 live births and due to diarrheal diseases of 6.4/1,000 live births), while Europe has the lowest burden (preterm birth: 2/1,000 live births, acute respiratory infections:0.8/1,000 live births; asphyxia and trauma during childbirth: 0.8/1,000 live births; and diarrheal diseases: 0.3 /1,000 live births).40
Preterm birth, low birth weight, and acute malnutrition are among the main causes of death in children under fiveyears of age.36,41 Chronic malnutrition, on the other hand, is responsible for irreversible physical and cognitive damage, and overweight is more related to chronic diseases.36 Global estimates for preterm birth are limited due to the quality of information about the delivery, particularly the difficulty in obtaining the gestational age. The most current data, available globally, date from 2014, with the prevalence rate ranging between 13.4% in North Africa and 8.7% in Europe.41 The persistence of high prevalence rates of preterm birth in wealthier countries is often related to greater survival due to adequate care for live births.41
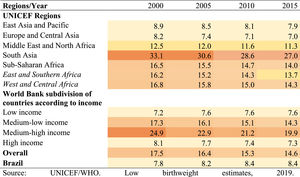
In 2015, the incidence of low birth weight at the globallevel was 14.6% (approximately 20.5 million live births), 91% of which were born in low- and middle-income countries.42 The downward trend ofthe prevalence of low birth weight was not very significant, with a slight reduction being observed in the period of 2000 to 2015 (Figure 3).
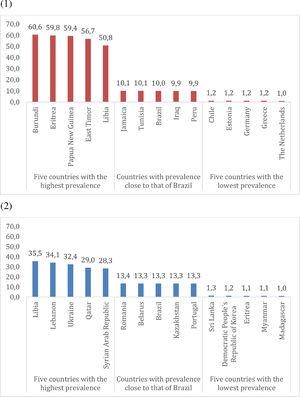
Over the last 20 years, the prevalence of chronic malnutrition at the global levelranged from 33.1% in 2000 to 22.0% in 2020, that is, a reduction of 67% in the considered period.43 In contrast, the global average prevalence of overweight showed a slight increase, from 5.4% in 2000 to 5.7% of the children in 2020.43 East Asia and the Pacific and the Middle East and North Africa accounted for almost 50% of all children affected by overweight worldwide and had the largest increases in the number of children affected by overweight between 2000 and 2020.43
The estimates of chronic malnutrition and overweight, according to the countries with the highest and lowest prevalence rates for the year 2020, are shown in Figure 4. The estimates of acute, chronic malnutrition and overweight according to the regions for the year 2020 can be seen in Table 1.43 The lower the degree of development, the worse levels of malnutrition can be observed. The prevalence of acute malnutrition ranged from 6.9% in low-income countries to 0.4% in high-income ones. The prevalence of chronic malnutrition was 34.6% and 3.4%, according to the worst and best income levels, respectively. In contrast, the prevalence of overweight was higher in countries classified as high-income (7.8%) when compared to low-income ones (3.7%). Malnutrition can result in more immediate and lifelong problems, and the maintenance of high rates is one of the consequences of poverty and the set of factors related to it.
Prevalence of short stature (1) and overweight (2) in children under 5 years old, according to countries with the highest and lowest prevalence rates, 2020.
Notes: Overweight (moderate and severe): Percentage of children aged 0 to 59 months who are above two standard deviations from the median weight-for-height of the WHO Child Growth Standards.
Short stature (moderate and severe): percentage of children aged 0 to 59 months who are below minus two standard deviations from the mean height-for-age of the WHO Child Growth Standards.
Estimates of acute malnutrition, short stature and overweight according to the regions, 2020.1
Source: UNICEF, WHO, World Bank Group Joint Malnutrition Estimates, April 2021 Edition. https://data.unicef.org/topic/nutrition/malnutrition/
1. Estimates for the year 2020 do not consider the impact of COVID-19. Household survey data on children's height and age were not collected in 2020 due to social distancing policies.
2. Eastern Europe and Central Asia, except Russia.
3. For moderate and severe acute malnutrition estimates, the North American regional average is based only on data from the United States.
Notes:
Acute malnutrition (moderate and severe): percentage/number of children aged 0–59 months who are below minus two standard deviations from the mean weight-for-height of the WHO Child Growth Standards.
Short stature (moderate and severe): Percentage of children aged 0 to 59 months who are below minus two standard deviations from the mean height-for-age of the WHO Child Growth Standards.
Overweight (moderate and severe): Number (millions) of children aged 0 to 59 months who are above two standard deviations from the median weight-for-height of the WHO Child Growth Standards.
In 2020, the COVID-19 pandemic triggered a series of events that had consequences for the global economy and resulted in the aggravation of social inequalities.44 Among the several events resulting from the pandemic are the discontinuity of health services and care, interruption of learning or changes in the school environment, interruption of social protection systems, increase in unemployment and informal employment, increase in food prices, among others.44-46 Taken together, they represent anactual threat with the potential to affect the health, nutrition, development, and well-being of children, especially those who belong to the most vulnerable groups of the population.44,47
The existing evidence demonstrates that children and pregnant women were the most affected groups by the pandemic, especially those who were already living in crisis-ridden areas, in a situation of food insecurity and/or with low coverage, quality, or access to health systems.45,46 The abrupt interruption of income that occurred during this period, especially among the poorest, exacerbated existing health inequalities and made others, such as gender violence, strongly emerge, affecting the physical and mental health.45,47 These conditions can lead to adverse consequences for the family's long-term mental health, especially for women,48 and may also affect the child's health outcomes, as these have an important determinant in the mental health of the accountable adults.
Despite the advances observed in child health in recent decades, adverse outcomes can be exacerbated again in times of worsening of poverty, food insecurity, and hunger, such as those currently occurring as a result of the global health crisis. The impacts of the COVID-19 pandemic are far-reaching, with a probable worsening of health indicators, even compromising the achievement of targets set out in the Sustainable Development Goals (SDGs) established by the United Nations.36,38,41,42
Therefore, social policies and those aimed at dealing with the crisis aggravated by the COVID-19 pandemic, with the intention of mitigating its effects on child health, must focus on the implementation of strategies for immediate relief of poverty and hunger, in addition to prioritizing measures to guarantee food security in the medium and long term and ensure access to education and health services.
Interventions to reduce child health inequitiesAs seen in the previous chapter, health problems affect children unequally across regions and countries worldwide, and this also happens within each country, state, or municipality. These inequalities are preventable, and there is no biological reason why, for instance, children up to 5 years living in low-income countries are 15 times more likely to die than those living in high-income countries.37 In other words, if the cause of illness and death is a social one, it is important that the remedy also bea social one. Treating existing diseases is essential; however, no treatment should exclude interventions on the social determinants of health.
Policies aimed at reducing health inequities require the articulation of a large number of actionsfrom different areas and levels. Therefore, a comprehensive approach must: 1) consider the levels of social determinants of health; 2) include the intersectionality of policies; and 3) promote social participation.16 Thus, fighting inequalities requires the coordination of different actors with different interests, vertically as well as horizontally, with the ability to attenuate differences and identify solutions, always guided by the inequity reduction principle.
Currently, it is possible to identify three distinct political approaches to reduce health inequities: those that seek to improve the health of poorer groups through targeted actions; closing health gaps between the least and the most advantaged groups; and those that address the entire health gradient. All these lines of work are effective and are not exclusive and can be complementary; however, they have structural differences. The first and the second are more focused on poverty, aiming to alleviate the burden of disease borne by the most disadvantaged. The third is concerned with the generalized effect that inequality has on health across the entire socioeconomic hierarchy. Although it is much more comprehensive, this model faces more political and technical difficulties than the first one.16 A combination of these three lines of action should be relevant in countries with a lot of poverty and inequality.
To promote maternal and child health, policies that address the different levels of determinants and address both poverty and health inequalities are required. For instance, policies that act to improve income and access to education and health services are crucial, such as redistributive policies, positively associated with lower infant mortality and longer life expectancy.5 Added to that, more specifically, conditional cash transfer programs that act on poverty are positively associated with the improvement of the nutritional and health status of children,49 as well as with the increased use of health services and preventive behaviors.50 Since the impact of programs on the health and nutrition status of families depends, to a large extent, on the supply and quality of basic services,51 an intersectoral approach, combining a cash transfer program with effective primary care, can considerably reduce morbidity and mortality, especially from poverty-related causes.49
The prevention of adverse outcomes related to childbirth and childhood also requires consideration of the structural causes related to poverty and social inequalities.52 Most government actions and health programs are still mainly concerned with a posteriori interventions that respond to incidental demands of individuals, with these responses being ineffective for public health problems, which continue to be reproduced.53
Therefore, depending on the political and social context of the country, the fight against social inequalities in health can include three distinct levels of action:5
- 1)
Macrosocial policies, such as economic and social policies that reduce poverty and increase equity: There is ample evidence that developed countries with positive indicators of childhood health underwent important changes before medical and health technologies were available. For example, the Western Europeancountries at the end of the 19th century had very high infant mortality rates, but a series of transformations took place on the economic, social, and environmental planes, causing these rates to be significantly reduced in the 20th century.54 However, when one observes from the perspective of equity in the course of these historical processes of intense socioeconomic transformation, even in developed countries, certain racial-ethnic groups or even the lower social classes benefitedless from these changes, showing the maintenance of large inequalities regarding child health.55
- 2)
Policies that modify the conditions of exposure and vulnerability of social groups: For advances in child health to occur and to accompany social transformations, it is necessary to activate a series of compensating mechanisms focused on a strategy to seek equity, which can not only reduce the existing inequalities in a sustainable way, as well as stop the forces that stimulate their expansion. Health in a population or country is linked to a complex series of determinants, as mentioned before. Policies focused on specific determinants have helped to improve child health and even existing inequities. Thus, policies aimed at improving sanitation conditions,56 nutrition57 and, in particular, measures to reduce poverty have contributed to improving child health.58,59 Special emphasis should be placed on recent poverty reduction interventions that have become frequent in many developing countries, called the cash transfer programs, whether conditional (when they establish requirements for recipients, generally related to the health and education of children and pregnant women) or not. Recent reviews show that they have played an important role in child health improvement.60,61 In Brazil, the Bolsa Família program has played an important role in reducing child mortality.58
- 3)
Health policies that act on the negative consequences of inequalities, seeking to minimize their effects on health: Health actions, especially primary care, have been of immense relevance to child health. This includes everything from prenatal care, childbirth care, and monitoring the child's health in the first years of life. The lack of this assistance or its inequitable distribution contributes to health inequalities among children. Health care includes access to adequate treatments for different types of diseases, immunization that currently covers a wide range of diseases, education, and caregivers’ education. In Brazil, the Unified Health System (SUS, Sistema Único de Saúde) and the Family Health Strategy, in particular, have made important contributions to improving overall and child health,in particular62 and to reduce inequities.63
The consequences of social inequalities on child health are among the major global health problems, not being specific to poor countries but also persisting when countries become wealthier and developed. Inequalities are produced through the complexity of the relationships of a group of social, economic, and health determinants, resulting in health problems and their unequal distribution. This may partly explain why, even when “old problems” such as hunger and diarrhea are solved, the persistence of inequalities makes “new problems” emerge; as an example, maternal mental health, which is relevant for the care and health of the child.
Despite the considerable advances observed globally in children's health, in recent decades, the inequalities expressed by the child's health indicators remain. The persistence of low levels of health in socially vulnerable groups of the population (expressed in the high rates of neonatal, infant, and under-five mortality, malnutrition, preterm birth, and low birth weight, among other adverse outcomes), makes it difficult to achieve the Sustainable Development Goals (SDG). This whole scenario was further affected by the COVID-19 pandemic, strengthening and increasing the need for integrative social and health policies to deal with the multidimensionality of children's health problems.
IRF and PRM receive a postdoctoral grant through the research project:NIHR Global Health Research Group on Social Policy and Health Inequalities, funded by the National Institute of Health Research, UK (Ref Number 16/137/99).